What is Vitreous Hemorrhage?
The vitreous humor is a clear, jelly-like substance that helps keep the eye’s shape and clarity. It fills about 80% of the eyeball and is made up of 98-99% water, with the remainder being collagen, hyaluronic acid, and electrolytes.
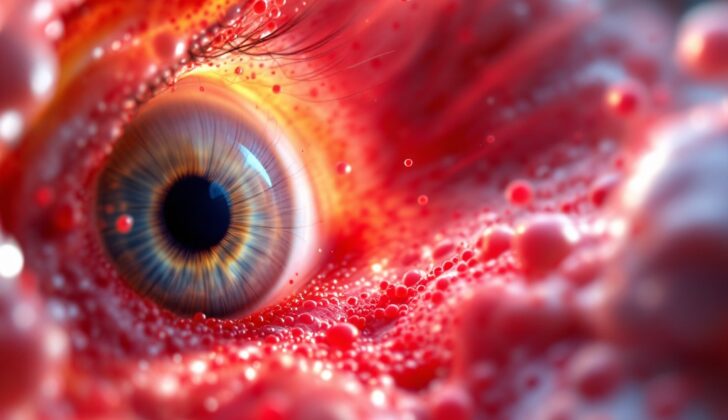
When there is blood in the vitreous humor, it’s referred to as a vitreous hemorrhage. This condition occurs when blood seeps into the space in the eye that is surrounded by the lens in the front, the internal limiting membrane (a thin layer that lines the inner surface of the retina) at the back, and the ciliary body (part of the eye that produces a fluid called the aqueous humor) at the sides.
Vitreous hemorrhage can appear in several areas of the eye:
- Preretinal or Subhyaloid hemorrhage: The blood is located between the clear hyaloid and the internal limiting membrane. This typically looks like a boat shape and does not move. It’s most commonly seen in conditions like proliferative diabetic retinopathy, a complication of diabetes that affects the eyes.
- Sub-Internal Limiting Membrane (Sub-ILM) hemorrhage: The blood is present between the nerve fiber layer of the retina and the internal limiting membrane. This condition might look very similar to subhyaloid hemorrhage, and in some cases, it might be impossible to differentiate between the two. Sub-ILM hemorrhage is more frequently seen in conditions such as Terson syndrome, retinal macroaneurysm, and Valsalva retinopathy.
- Intragel (Inside the jelly-like substance of the eye): The blood is scattered within the gel of the eye, and can turn from red to yellow over time as red blood cells break down.
There are also other fluid-filled spaces in the eye, such as the canal of Hannover, Berger’s canal, the canal of Petit, and Cloquet’s canal. These spaces are filled with a fluid called aqueous humor. If blood gets into any of these canals, it’s also considered vitreous hemorrhage.
What Causes Vitreous Hemorrhage?
Vitreous Hemorrhage (VH) can happen for a range of reasons, and it’s important that you know what they are. That’s why we’ve compiled this list, detailing all the various causes of VH.
– Proliferative Vascular Retinopathy: This is when new blood vessels grow due to lack of oxygen in the retina, causing them to bleed. This can be caused due to various health conditions such as diabetes, a blockage in a vein of the retina, inflammation of the vessels in the retina, inflammation inside the eye, a type of anemia called sickle cell, and a condition that affects the development of blood vessels in the retina of premature babies.
– Neovascular Age-related Macular Degeneration (AMD): This occurs due to abnormal blood vessel growth in the part of the eye responsible for sharp, central vision.
– Idiopathic Polypoidal Choroidal Vasculopathy (IPCV): In this condition, abnormal blood vessels in the eye can cause bleeding.
– Trauma: You might find it surprising but trauma is the most common cause of VH in people under 40 years old, especially in males. This can come from any blunt or penetrating damage to the eye, rupturing blood vessels and leading to VH.
– Intracranial Hemorrhage (Terson Syndrome): This is a complex one – it’s when there’s bleeding within the eye due to a brain hemorrhage. According to research, it was seen in 19.3% of patients with a type of stroke, 9.1% of patients due to bleeding in the brain, and 3.1% of patients with a traumatic brain injury.
– Retinal Arterial Macroaneurysm (RAM): This is a condition in which a large swelling of a blood vessel in the retina can result in bleeding within the eye.
– Posterior Vitreous Detachment (PVD): This can cause VH in some cases. This condition happens when the gel at the back of your eye shrinks and separates from the retina, sometimes leading to a tear or bleeding.
– Tumors: Sometimes, tumors in the eye can cause VH, although this cause is quite rare.
– Blood dyscrasias: These are conditions that affect blood cells or plasma and cause bleedings, such as leukemia, anemia, low blood platelets, and hemophilia.
– Valsalva retinopathy: Sudden increases in pressure in the chest or abdomen can cause VH. These pressure surges could be caused by lifting something heavy, coughing, vomiting, or straining too hard.
– Complications of Surgeries: Like any surgery, eye surgeries can come with complications, and this includes VH.
– Shaken Baby Syndrome: This is a severe form of child abuse that results in brain injury. Trauma to the eye causing VH is a common symptom.
As always, getting regular eyecare is essential to detect and treat these conditions as early as possible.
Risk Factors and Frequency for Vitreous Hemorrhage
Spontaneous vitreous hemorrhage is a condition where blood leaks into the clear gel-filled space in the eye. Each year, around 7 out of every 100,000 people experience this issue. However, in China, the rate is much higher, with nearly 5 out of every 10,000 people experiencing this problem. It’s most common in people aged 40 to 59, particularly in males and people who take blood thinners.
- Every year, around 7 in every 100,000 people experience a spontaneous vitreous hemorrhage.
- In the Chinese population, the rate is almost 5 in every 10,000 people.
- The condition is most common in people aged 40 to 59.
- Men are more likely to experience this condition than women.
- People who take blood thinners have a higher risk of having a spontaneous vitreous hemorrhage.
Signs and Symptoms of Vitreous Hemorrhage
A vitreous hemorrhage is a condition where there’s bleeding into the jelly-like substance that fills the back of your eye, known as the vitreous. A person with this condition may typically mention seeing floaters, shadows, or cobwebs, or experiencing a haze in their vision. The condition is usually painless and how much it affects the clarity of one’s sight can depend on the quantity of blood involved. Note however, even a tiny amount of blood can significantly reduce vision down to just being able to perceive hand motions. If a person also notes seeing flashes, this could be indicative of a tear in the retina or retina detachment.
Evaluating a person suspected of having a vitreous hemorrhage also involves recording their best-corrected vision, checking for a relative afferent pupillary defect, and using a slit lamp examination to further assess the front part of the eye. During the slit lamp examination, signs of abnormal blood vessels or inflammation may be seen. The pressure within the eye should also be measured.
Vitreous hemorrhage appears as blood in the vitreous obscuring the view of the retina. A subhyaloid hemorrhage, if present, may have a distinct boat shape. A thorough check of the retina, particularly if a tear or detachment is suspected, is necessary. It’s also recommended to check the other eye, as similar issues might be present.
Finally, it’s essential to inquire about a person’s medical history, including systemic diseases like hypertension and diabetes, or any family history of blood disorders. Information regarding any eye trauma, instances of violent cough, heavy weight lifting, or previous eye surgery is also important.
Testing for Vitreous Hemorrhage
When dealing with laboratory investigations, common tests include checking for blood sugar levels, analyzing a complete blood count (which is a blood test that counts all the cells in your blood), assessing how quickly your blood clots, and evaluating your platelet count (the cells in your blood that help it clot). A peripheral blood smear test might also be done, where a drop of your blood is examined using a microscope to study the cells in detail.
In the case where the doctor can’t obtain a clear view of the back of the eye due to excessive blood leakage into the vitreous (or clear jelly-like substance in our eyes), an ocular ultrasound is typically performed. This uses sound waves to form pictures of the inside of the eye and can help doctors determine the source and characteristics of the hemorrhage. The characteristics of the ultrasound can differ based on whether the hemorrhage is fresh or old, and whether the eye has previously undergone vitrectomy, a surgery to remove some or all of the vitreous.
Optical Coherence Tomography (or OCT), is a commonly used test, particularly when there is bleeding in front of the macula (the part of the eye that gives us sharp, clear vision). It helps doctors determine the exact location of the bleed to plan for treatment.
Fundus Fluorescein Angiography (FFA) and Indocyanine Green Angiography (ICGA) are types of imaging techniques that use a special dye and camera to look at blood flow in your retina and choroid (the layer of blood vessels and connective tissue in the middle part of the eye). They are performed in cases where doctors can get a view through mild to moderate amounts of blood leakage in the vitreous. This helps them pinpoint areas where blood flow is blocked, or where there are abnormal blood vessels, to plan laser treatment. ICGA is also useful for examining specific eye conditions because it provides better clarity due to the use of a more extended light wavelength as compared to FFA.
If doctors suspect Terson syndrome, where the blood leakage is associated with bleeding in the brain, or in cases of an open globe injury where the outer coat of the eye is breached, CT and MRI scans of the brain and orbit can be performed. These scans can also help the doctor to examine other aspects, like checking for any injury in the bone surrounding the eye, any foreign bodies within the eye, and to assess the condition of the eye wall.
Lastly, in rare instances, a test called flash visual evoked potential (VEP) or bright flash electroretinogram (ERG) may be done. This test measures the electrical responses of various cells in the eye, including the light-sensing cells in the retina, to predict the visual potential in cases with dense vitreous hemorrhages.
Treatment Options for Vitreous Hemorrhage
Treatment plans for vitreous hemorrhage, a condition marked by bleeding inside the eye, should be formulated based on the individual patient and the identified cause of the condition.
If the cause of bleeding is unknown, the patient may be recommended to await further treatment under specific circumstances. This could involve maintaining an upright position, allowing the blood to settle at the bottom of the eye, and then conducting a re-evaluation within a week. Alternatively, if the cause is known, medical professionals may choose to observe the patient for a few weeks to see if the condition improves. In these cases, they would also monitor for complications, such as a detached retina. Patients who have new blood vessels developing inside their eyes may be advised to avoid strenuous activities.
In some instances, laser photocoagulation may be recommended to treat diseases causing blood vessel growth, like diabetes. This method uses a laser to burn the retina, reducing the release of chemicals that stimulate blood vessel growth. The treatment reduces the risk of vision loss.
There’s also an option of using a process called cryotherapy, which uses very cold temperatures to treat the peripheral areas of the retina. But caution is maintained since this process can lead to inflammation. Therefore, it’s often avoided if there are other options available.
Another technique used to treat vitreous hemorrhage is pars plana vitrectomy (PPV). This involves a surgery to remove and replace the vitreous, a clear fluid that fills the eye. It’s traditionally administered when there are complicated factors involved, such as retinal detachment, infections, prolonged bleeding, or damage due to an injury.
Anti-vascular endothelial growth factor (VEGF) injections are another potential treatment. These are administered before surgery to reduce the risk of bleeding. They can also be used in situations when progress cannot be visually monitored due to blood within the eye.
Finally, some experimental treatments are being researched, such as injections of various agents and oral medications. However, these are yet to be established as effective treatments. Along with these techniques, it’s important for the doctor to help the patient manage any underlying health conditions that could be contributing to their eye issue. For instance, patients with inflammation in their eyes may need steroid treatments in conjunction with other therapies to manage their vitreous hemorrhage.
What else can Vitreous Hemorrhage be?
Vitreous inflammation, or vitritis, can be caused by either infection or inflammation. Patients typically experience a reddening and discomfort of the eye. An eye examination might reveal signs of inflammation such as keratic precipitates, anterior chamber cells and flare, posterior synechia, complicated cataract, and anterior vitreous cells. The back of the eye could display signs of retinal or choroidal inflammation or blood vessel inflammation. An ocular ultrasound might shows dots or cobweb-like lines in the vitreous. If the condition is severe, the ultrasound may also show thick, reflective membranes. Other signs may include widening of the Tenon’s space, thickening of the outer layers of the eye, choroidal detachment, exudative RD, or optic disc elevation. Vitritis can be seen in conditions like panuveitis, endophthalmitis, and retino-choroiditis.
Primary intraocular lymphoma, which can present similarly to long-term vitreous hemorrhage, is another condition that can mimic vitritis. Asteroid hyalosis is another condition that resembles vitrous hemorrhage on an ultrasound. It is seen as multiple, small, highly reflective echoes that move, with a clear gap seen between these echoes and the back wall of the eye. In most cases, patients do not have any symptoms with asteroid hyalosis.
Retinal Detachment (RD) can also seem like a blood lined PVD (posterior vitreous detachment) on a B scan. A retinal detachment is uniformly reflective, evenly thick, and has limited movements. A blood lined PVD, on the other hand, may display moderate to high reflectivity, variable thickness, and usually has a high level of mobility.
What to expect with Vitreous Hemorrhage
The process of clearing blood from the vitreous, which is the clear, jelly-like substance that fills the middle of the eye, happens at a slow rate of about 1% per day. The progress and outcome of a case with vitreous hemorrhage, or bleeding into the vitreous, depends on the cause of the condition.
Certain eye conditions that do not cause repeated bleeding, like when a blood vessel is pulled off due to a tear in the retina or the posterior vitreous detachment (which is when the vitreous shrinks and pulls away from the retina), tend to have positive outcomes.
However, in cases where the vitreous hemorrhage is caused by diabetic retinopathy, an eye disease that can occur in people with diabetes, the prognosis is usually worse. Studies have shown that vision improved in 30% of these cases, stayed the same in 28%, and got worse in 42%. Most of the eyes (71%) had a vision of 5/200 or less. The reasons for this poor vision include persistent or recurring bleeding, the retina detaching due to pulling force (tractional retinal detachment), scar tissues on the retina (pre-retinal fibrosis), and increased pressure in the eye (neovascular glaucoma).
With retinal vein occlusions, or blockages in the small veins of the retina, central retinal vein occlusion is the worst, branched retinal vein occlusion is the best, and hemiretinal vein occlusion lies somewhere in between in terms of prognosis. Repeated hemorrhages were noticed in 28% of cases with branched retinal vein occlusion.
People with proliferative sickle cell retinopathy, an eye disease that can occur in people with sickle cell disease, generally have a better prognosis compared to those with diabetic retinopathy regarding recurring bleeding and vision loss, with rare instances of permanent visual loss. In Terson syndrome patients, 75% were found to have a vision better than 20/50 at the end of 3 years.
The prognosis is typically bad for eyes with vitreous hemorrhage caused by age-related macular degeneration, another eye condition more common in older people, with vision rarely better than seeing hand movements. The cause for the poor vision is usually a large hemorrhage under the retina at the macula, the part of your eye responsible for sharp, detailed vision. However, cases with retinal macroaneurysm, or abnormal enlargement of a blood vessel in the retina, usually have a good prognosis in terms of vision and rebleed.
Possible Complications When Diagnosed with Vitreous Hemorrhage
“Hemosiderosis Bulbi” is a condition that’s similar to siderosis bulbi, which happens when a foreign body gets inside the eye. It starts when iron is released from the breakdown of red blood cells. This takes place inside special cells known as macrophages where iron is stored in two forms: ferritin and hemosiderin. Eventually, this iron is released into a part of the eye called the vitreous.
Meanwhile, other proteins in the vitreous latch onto this iron. Because the breakdown of red blood cells is slow, only a small amount of iron is released at any one time. These proteins in the vitreous are able to bind with this iron, making the chance of getting hemosiderosis bulbi very low.
However, the iron can bind permanently to various structures in the eye, particularly those derived from the outer layer of the optic cup– including parts like the retinal pigment epithelium, lens epithelium, ciliary body, iris dilator and sphincter muscles, structures around the blood vessels of the retina, optic nerve, and trabecular meshwork.
Retinal changes in hemosiderosis can result in decreased amplitude of the b wave in an Electroretinogram (ERG), followed by peripheral vision loss, night blindness, loss of central vision, color perception disturbance, and finally full ERG extinction.
Another condition, “Glial and Fibrivascular Proliferation,” is caused when blood, blood products or iron lead to proliferation or growth along the vitreous and retinal surface. This can cause traction or pulling force on these parts.
Patients with a posterior penetrating injury in the eye coupled with vitreous hemorrhage are at higher risk of developing a tractional retinal detachment. This theory is supported by experiments conducted on rabbit eyes.
Another eye condition after vitreous hemorrhage is Ghost Cell Glaucoma, which happens when red blood cells lose their shape and flexibility over time. These cells obstruct the eye’s drainage system, leading to a type of glaucoma.
Signs of this condition include cells appearing Khaki-colored in a deep anterior segment of an eye, which may color the trabecular meshwork. They may settle at the bottom of the eye giving a false appearance of a hypopyon.
Other types of glaucoma like Hemolytic Glaucoma can be caused by red blood cell debris and macrophages loaded with hemoglobin blocking the trabecular meshwork. Hemosiderotic Glaucoma is a rare condition where iron released from red blood cells reaches the trabecular meshwork, causing damage and obstruction.
As a consequence of this condition, a child’s visual development (called Amblyopia) may be affected and a shift towards myopia might occur. This is particularly observed in infants; therefore an early procedure known as vitrectomy is recommended to prevent these conditions.
Preventing Vitreous Hemorrhage
When people have a condition called a vitreous hemorrhage, they may notice symptoms like floaters in their vision, or a mild blurriness. However, many people tend to overlook these symptoms at first. Usually, they will seek help only when their vision has gotten significantly worse, and by then, surgery is typically the only treatment option.
Seeking advice from an eye doctor – an ophthalmologist or optometrist – sooner rather than later could help avoid complications and may even reduce the chance needing surgery. If it’s decided to just observe the condition for the time being, it’s crucial for patients to understand how important it is to keep their head raised. Compliance with this instruction is key.
Often, this eye issue is caused by some underlying illness that isn’t being managed properly. Thus, it is crucial for patients to understand that managing their overall health is key in preventing such complications from arising.