What is Wet Age-Related Macular Degeneration (AMD)?
The retina is a part of your eye that transforms light into signals that your brain can understand as images. In the retina, there’s a section called the macula that’s dense with cones – these are key for clear, direct vision. Wet age-related macular degeneration (AMD) mainly affects the macula. This condition is a prevalent cause of blurred or lost vision in the middle of the visual field in older people in developed countries.
There’s a protein called vascular endothelial growth factor (VEGF) that stimulates the growth of new blood vessels, a process known as choroidal neovascularization (CNV). In this process, new vessels grow underneath or through a layer of cells at the back of the eye which can lead to vision impairment if not treated correctly. Regular intake of anti-VEGF medications can prevent blindness in the majority of those with wet AMD. Without these medications, there’s a risk of serious, irreversible vision loss.
What Causes Wet Age-Related Macular Degeneration (AMD)?
Age-related macular degeneration (AMD) is a disease caused by a combination of different factors. A range of things can increase your risk of developing this disease, such as:
- Getting older
- Having high cholesterol
- Being deficient in certain micronutrients
- Smoking
- Having a family history
- Having high blood pressure
- Having heart disease
- Being exposed to certain types of light
Your genes can also play a big role in getting AMD. Research shows that at least 34 different positions on our DNA (called “genetic loci”) and 52 different versions of genes are linked to the disease.
Inflammation, or the body’s response to injury or infection, is thought to play a big role in causing wet AMD, a particular type of the disease. Some people have changes in a gene that normally helps to control inflammation, called the Complement Factor H gene. These changes, or “mutations”, could lead to more inflammation and hence contribute to developing AMD.
Risk Factors and Frequency for Wet Age-Related Macular Degeneration (AMD)
In 2015, Age-related Macular Degeneration (AMD) was listed as the third most common cause of serious vision loss worldwide. Generally, about 8.7% of people between the ages of 45 to 85 are affected by AMD, with a smaller percentage (0.4%) having an advanced form of the disease. It has been observed that the early stage of AMD is more common in those of European ancestry in comparison to Asians, and it is less common in people of African origin. Experts predict that the number of people affected by AMD will escalate from 196 million in 2020 to 288 million by 2040.
- About 10% to 15% of those with AMD will develop a form of the disease known as neovascular disease.
- Without a specific treatment called anti-VEGF therapy, between 79% to 90% of eyes affected by neovascular disease will become legally blind due to complications.
Signs and Symptoms of Wet Age-Related Macular Degeneration (AMD)
Wet Age-Related Macular Degeneration (AMD) can cause issues with a person’s eyesight. It’s typically marked by issues with near or central vision, with blurring or distortion commonly reported. Some people might see distorted images, smaller-than-normal objects, or might experience blind spots. However, others might not have any obvious symptoms or might only have a vague feeling that their vision isn’t quite right.
During a check-up, a person with wet AMD might not have perfect vision, even with glasses or contacts. The Amsler grid test, a tool used to detect vision problems, might show blind spots or distorted vision. When the front part of the eye is examined, everything often appears normal. Age-related cataracts or artificial lenses might also be noticed.
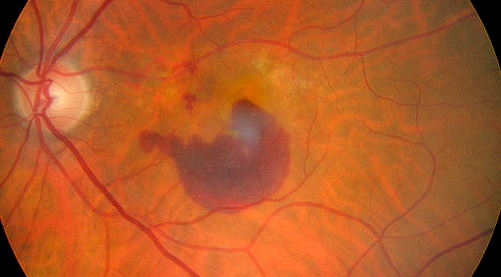
In more detailed examinations, a few distinct signs of wet AMD might appear:
- A gray-green layer deep in the retina with potential retinal detachment on top
- Blood, lipids, or fluid under the retina
When the layer of cells at the back of the eye (RPE) is removed from its usual flat shape, it might be filled with fluid, blood vessels, tiny yellow deposits, or blood. This detached RPE can appear very sharp and dome-shaped. If there are large bleedings under the retina, central vision loss can occur. Sometimes, the bleeding can break into the gel-like substance that fills the eye, causing peripheral vision loss.
If there are large bleedings under the retina (at least the size of 4 disc areas), it’s important to check whether the patient is using blood thinners or has any blood disorders.
Testing for Wet Age-Related Macular Degeneration (AMD)
Wet AMD, or wet age-related macular degeneration, is a condition that affects the eye. To diagnose and make decisions about treating wet AMD, doctors use a variety of eye imaging techniques that allow them to see changes in the retina and choroid, which are parts of the eye. Here are some of the tests they might use:
Optical Coherence Tomography
Optical Coherence Tomography, or OCT, is a test that uses light to create detailed images of the retina and other structures in your eye. This technology allows doctors to see fluids or other changes in your eye that could indicate wet AMD. When your doctor uses OCT to investigate your eye, they might see specific patterns that suggest the presence of fluid in and around the retina, or other changes related to the health of the eye.
Optical Coherence Tomography Angiography
Optical Coherence Tomography Angiography, or OCTA, is a newer test that allows the doctor to see images of the blood vessels in the retina. This method can help doctors find any abnormalities in the blood vessels even before these are visible on other tests like OCT or fluorescein angiography.
Fundus Fluorescein Angiography
The Fundus Fluorescein Angiography, or FFA, uses a fluorescent dye to illuminate the blood vessels in the retina, giving doctors information about the blood flow and highlighting any changes that could be indicative of wet AMD. This diagnostic method is especially useful as it can classify lesions in the eye, helping doctors decide the best course of treatment. However, relying only on OCT for diagnosing active wet AMD may result in overtreatment, which implies the importance of FFA.
Indocyanine Green Angiography
Indocyanine Green Angiography, or ICGA, uses a different type of dye that is particularly good at showing the choroidal circulation – the network of blood vessels supplying the choroid, a part of the eye. With this test, doctors can see details that might not be evident with other methods, such as ‘hidden’ abnormal blood vessels. This method allows for early diagnosis and helps determine the patient’s prognosis, or likely outcome.
All of these techniques used together provide your doctor a complete picture of what’s going on in your eyes and help him or her to make the best treatment decisions for you.
Treatment Options for Wet Age-Related Macular Degeneration (AMD)
Wet age-related macular degeneration (AMD) is commonly treated using a group of drugs known as anti-VEGF (vascular endothelial growth factor) therapies, which can prevent vision loss and, in some cases, improve vision.
Pegaptanib sodium was the first anti-VEGF drug approved by the FDA to treat wet AMD, but this drug has largely been replaced with improved alternatives like bevacizumab, ranibizumab, and aflibercept due to better results shown in various trials.
Ranibizumab specifically binds all forms of the protein VEGF-A and is effective in treating the condition. However, bevacizumab, though officially approved for treating colorectal cancer, is frequently used for AMD treatment and has proven to be noninferior to ranibizumab.
Similarly, aflibercept effectively traps all forms of VEGF; the FDA approved its use for wet AMD and its dosage can prove as effective as ranibizumab taken monthly. Brolucizumab, a low-molecular-weight VEGF antagonist, is another FDA-approved treatment for wet AMD, although questions have been raised about its safety after reports of severe inflammation following administration.
Other recent drugs approved by the FDA for AMD include ranibizumab-nuna, ranibizumab-eqrn, and aflibercept biosimilars aflibercept-jbvf and aflibercept-yszy. Faricimab-svoa, another FDA-approved drug, shows promising results and is used to bind VEGF and angiopoietin-2, another factor that contributes to the development of choroidal neovascularization, which is a condition associated with AMD.
When these anti-VEGF agents are administered, they often follow a fixed dosage schedule that varies by drug, or an “as needed” schedule where a patient receives injections only when the disease appears active. There also exists the “treat-and-extend” protocol, where injection frequency is slowly extended as long as the disease is controlled. The most effective treatment options are chosen collaboratively by the patient and the doctor.
Like all treatments, intravitreal anti-VEGF agents come with several risks, including common adverse events like subconjunctival hemorrhage, discomfort, and the presence of floaters. Serious adverse events, though rare, can include vitreous hemorrhage or endophthalmitis. Some studies also suggest potential systemic adverse events such as myocardial infarction, stroke, nonocular hemorrhage, and thromboembolic events, but the current evidence does not suggest an increase of these risks.
Several other potential therapies are being studied. For example, abicipar pegol may be limited in use due to higher reported rates of inflammation, while conbercept, a VEGF decoy protein similar to aflibercept, appears to some potential advantages and will likely undergo FDA trials in the future. Other up-and-coming treatments include sustained-release delivery devices and gene therapy.
Prior to the introduction of anti-VEGF therapy, surgical interventions like submacular surgery, laser photocoagulation, and photodynamic therapy played a significant role in the treatment of wet AMD, although they’ve lost their importance due to the efficacy of anti-VEGF treatments.
Radiation therapy has also been considered, but studies have not found a clear benefit. Finally, gene therapy, especially with drug RGX-314, shows promise as a future treatment method for wet AMD.
What else can Wet Age-Related Macular Degeneration (AMD) be?
When trying to identify the cause of ‘choroidal neovascularization’ (CNV) due to wet age-related macular degeneration (AMD), doctors must also consider other possible causes. Such conditions, which might lead to similar symptoms, are as follows:
- Wet AMD
- Pathological myopia
- Angioid streak
- Presumed ocular histoplasmosis syndrome
- Punctate inner choroidopathy
- Serpiginous choroiditis
- Serpiginous-like choroiditis
- Multifocal choroiditis
- Sympathetic ophthalmia
- Vogt-Koyanagi-Harada syndrome
- Ocular tuberculosis
- Toxocariasis
- Toxoplasmosis
- Rubella
- Choroidal rupture
- Laser burns
- Iatrogenic (after vitreoretinal surgery)
- Best vitelliform macular dystrophy
- Fundus flavimaculatus
- Optic disc drusen Tumors
- Choroidal osteoma
- Choroidal hemangioma
- Choroidal nevus
- Choroidal metastasis
- Combined hamartoma of the retina and retinal pigment epithelium (CHRRPE)
Diagnosis might become difficult if there’s excessive bleeding in the eye’s vitreous (the clear part in the back of the eye), a condition also associated with wet AMD. In such cases, the doctors can consider the patient’s history or evaluate the other eye. Some other conditions that can cause bleeding in the vitreous include:
- Proliferative diabetic retinopathy
- Retinal tear or retinal detachment
- Hemorrhagic posterior vitreous detachment
- Neovascularization due to other causes like vein occlusions, radiation retinopathy, or sickle cell retinopathy
It’s also important to remember that some other eye conditions like peripheral exudative hemorrhagic chorioretinopathy and retinal angiomatous proliferation (RAP) might cause similar symptoms. Peripheral exudative hemorrhagic chorioretinopathy, most common in older people, often presents with blood or fluid accumulation in the back of the eye. RAP, a variant of wet AMD, generally starts deep within the retina and then grows outward. Both these conditions can be managed with treatments similar to other types of CNV.
What to expect with Wet Age-Related Macular Degeneration (AMD)
If wet age-related macular degeneration (AMD) remains untreated for 2 to 3 years, about half to more than half of those affected could lose significant vision. This condition is specifically termed ‘subfoveal choroidal neovascularization’ or ‘CNV’. In comparison, 20-30% of individuals with any form of submacular CNV poses the risk of substantial vision loss.
CNV can come in different types, with ‘classic CNV’ being a more severe version. Patients with classic CNV experience worse visual outcomes than those with less severe versions and without classic lesions. What’s more concerning is that up to 50% of patients initially diagnosed without classic lesions might develop classic CNV within the first year after diagnosis.
Large subretinal hemorrhages, particularly those affecting the fovea (the part of the eye responsible for sharp central vision), often result in poor vision. Regardless, some patients have shown surprisingly good recovery in their vision. This implies that prompt treatment, such as intravitreal anti-VEGF medications or surgery, can be beneficial.
If retina pigment epithelium (RPE) tears affect the fovea, it usually leads to lower visual acuity, or clearness of vision. On top of that, it increases the chances of vision loss from an RPE tear in the other eye.
Possible Complications When Diagnosed with Wet Age-Related Macular Degeneration (AMD)
Not treating wet AMD (Age-related Macular Degeneration) can result in permanent vision loss for most people. Vision loss can still happen even if you’re getting treatment. It’s often noticed that people with vision loss from AMD indicate their quality of life has been degraded. They typically report higher levels of emotional distress, worse health, and less ability to independently perform day to day activities when compared to people suffering from other lasting illnesses.
Here are some reported effects of vision loss from AMD:
- Permanent vision loss
- Lower quality of life
- Increased emotional distress
- Poorer health
- Less independence in daily activities
Preventing Wet Age-Related Macular Degeneration (AMD)
If you are a patient with macular drusen (small yellow deposits that form under the retina), it’s important to regularly use an Amsler grid. This is a simple check-up tool that you can use at home to monitor your vision for any changes such as distortions (metamorphopsias) or blind spots (scotomas). These changes could be signs that your condition is progressing from dry to wet age-related macular degeneration (AMD), which involves new blood vessels growing under the retina. If you notice any changes in both your near or far vision, make sure to contact your eye doctor as soon as possible.
Making certain lifestyle changes can also be beneficial. This might involve eating a balanced diet rich in various nutrients, wearing sunglasses to protect your eyes from excessive light, and doing regular exercise. Make sure to visit your primary doctor regularly to manage any other health conditions you might have. Some patients might also be advised to take particular vitamin supplements known as Age-Related Eye Disease Study (AREDS) or AREDS2 ingredients. Research has shown that these vitamins can help stop AMD from getting worse in patients who have a medium or advanced level of the disease in one eye.
If your vision is already quite impaired, you may find it helpful to use visual aids and access resources designed for people with limited vision. A low-vision clinic can provide educational resources and various tools to help you manage, such as handheld magnifiers, devices that magnify images on an electronic screen (closed-circuit television viewers), and accessibility apps on devices like smartphones and tablets. Don’t forget that libraries often have materials like large-print books and audiobooks. Social services can also provide assistance to help you maintain as much independence as possible.