What is Hypospadias?
Hypospadias is a birth defect in boys where the opening of the urethra, the tube that carries urine from the bladder to the outside of the body, isn’t located in the usual place. Instead of being at the tip of the penis, it might be found somewhere along the underside. This happens because of abnormal development of the urethral fold and the foreskin on the underside of the penis.
With hypospadias, the location the urethra opens can vary and there may be a bend in the penis. Depending on where the opening is, the child may have additional birth defects in their urinary tract.
Recent medical advances mean that babies younger than 12 months can undergo a single-stage operation to correct the defect. This procedure tends to have good outcomes.
What Causes Hypospadias?
The exact cause of hypospadias, a condition where the opening of the urethra is on the underside of the penis instead of at the tip, isn’t fully known yet. However, we believe that it could be influenced by a combination of genetic factors, hormonal influences, and environmental factors.
It is known that genetics play a role since this condition is more commonly seen in boys who have a family history of hypospadias. This means that if another male in the family has the condition, the chance the boy might have it increases.
There’s also a connection between hypospadias and the hormones known as androgens. Some boys may have low levels of these hormones, or their bodies may not respond as strongly to these hormones, and this can contribute to the development of hypospadias.
Recent studies suggest that exposure to certain substances in the womb, like estrogens found in pesticides on fruits and vegetables or in the lining of plastics, can also influence the development of hypospadias.
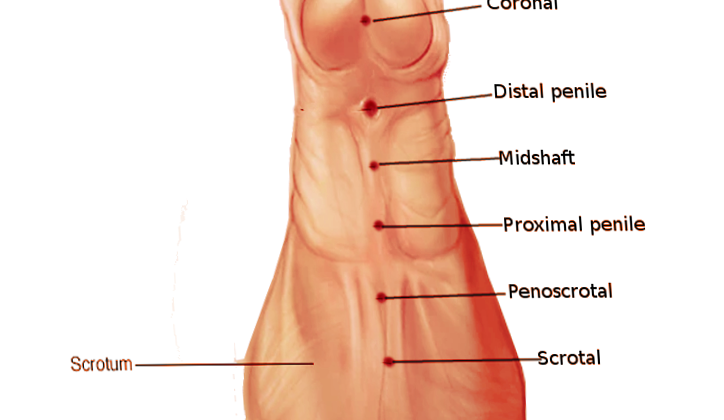
Hypospadias can be categorized by the location of the urethral opening. It’s usually classified into three types:
1. Anterior: the opening is near the tip of the penis.
2. Middle: the opening is in the middle of the penis.
3. Posterior: the opening is near the base of the penis.
In nearly half of the cases, the opening is in the anterior location. Around 20% of cases happen in the middle location, and the rest happen in the posterior location. The most common is the anterior or subcoronal position, which is just underneath the head of the penis.
Risk Factors and Frequency for Hypospadias
Hypospadias is a common birth defect in males, second only to cryptorchidism. However, when it comes to abnormalities specifically related to the penis, it’s the most frequent one seen.
- In the US, out of every 250 males, one is believed to have hypospadias (0.4%).
- In Denmark, the condition’s estimated prevalence is between 0.5% and 0.8%.
- A study conducted in South America has suggested that globally, out of every 10,000 newborns, roughly 11.3 typically have hypospadias (less than 0.1%).
Signs and Symptoms of Hypospadias
Hypospadias is a condition usually diagnosed soon after a baby boy is born. Its main characteristics are a groove on the top end of the penis, an incomplete foreskin on the underside and an abnormally placed opening for urination (urethral meatus). If the baby has a complete foreskin, hypospadias might become evident only after a circumcision. For this reason, if hypospadias is discovered during circumcision, the process should stop immediately, and the baby should be referred to a urologist. Sometimes, some patients may also have a bend in the penis, which becomes more noticeable when the penis is erect. It’s beneficial to gather a detailed patient and family history, including if there were any previous cases of hypospadias in the family.
Testing for Hypospadias
Hypospadias is a condition that affects the way the penis is formed. There are three common types of this condition: distal, midshaft, and proximal.
– Distal hypospadias is the most usual type, and it occurs in about 60% to 70% cases. Sometimes it’s called anterior or minor hypospadias and it involves the gland and sub-coronal areas of the penis. It’s usually less severe.
– Then, we have midshaft hypospadias which also affects the middle and proximal sections of the penis. This type of hypospadias is also known as penile hypospadias.
– The third type is posterior hypospadias. It involves the peno-scrotal, scrotal, and perineal areas of the penis.
Regardless of the type, people with hypospadias often have an unusual appearance of the foreskin – it appears more abundant on the upper side of the penis and is either absent or scant on the lower side.
If the hypospadias is mild, it might not affect the direction of the urine flow, but if it’s severe, it can result in a downward stream due to a narrowed opening (meatus) of the penis. Severe hypospadias can cause painful erections, issues with fertility due to irregular ejaculation, and even difficulties during intercourse because of penetration problems.
Typically, hypospadias occurs on its own, but sometimes it can come along with other genito-urinary abnormalities. When hypospadias is proximal, it may often be accompanied by cryptorchidism (a condition when one or both of the testes fail to descend) or inguinal hernias. There could also be kidney and urinary tract issues, but that’s usually quite rare.
Remember, hypospadias can also be a part of nearly 200 different syndromes, including WAGR syndrome, Denys-Drash, Smith-Lemli-Opitz, Wolff-Hirschhorn, CHARGE. These syndromes might have symptoms such as tumors, heart defects, growth delays, and other abnormalities.
Treatment Options for Hypospadias
If a baby is diagnosed with a condition called hypospadias (where the opening of the urethra is on the underside of the penis, rather than at the tip), it is advised to consider surgical evaluation within the first few weeks of the baby’s life. If parents wish to have their newborns circumcised, they should be aware that any abnormality in the penis suggests that circumcision should not be performed. This is because the foreskin can be useful during surgical repairs.
Hypospadias located near the base of the penis (referred to as proximal hypospadias) is often connected with other issues in the genital and urinary systems. To rule out a condition called intersex (where the physical characteristics of sex are not typical of male or female), doctors typically order a test called a karyotype if one or both testes are undescended. An ultrasound of the kidney, bladder, and abdomen may also be performed to check for any abnormalities in the internal organs.
In cases where the hypospadias is located in the middle or near the tip of the penis (midshaft and distal hypospadias), a surgical evaluation is necessary. However, no additional tests are typically required in this case, as the likelihood of kidney anomalies is the same as in the general population.
The goal of surgery for hypospadias is to straighten the penis and create a urinary opening of the right size. This aims to achieve the look of a typical circumcised penis or a penis with a foreskin, along with ensuring a good cosmetic result.
The main treatment for proximal hypospadias is surgery. This typically involves a two-stage repair procedure. The first surgery focuses on straightening the penis, while the second stage of surgery involves constructing a new urinary channel.
In some instances, before the surgical repair can take place, the patient may be given a course of treatment with testosterone derivatives. This is done to increase the size of the penis, which can make the surgical repair easier and possibly reduce complications. The exact guidelines for the use of testosterone are not defined.
Surgery is usually recommended when the baby is between 6 and 18 months old, as carrying out the treatment at a later stage in life may lead to psychological stress and behavior problems. Delaying the procedure may also increase the risk of complications such as the formation of abnormal connections between the urethra and the skin (urethrocutaneous fistulas). The process of repairing hypospadias is complex and involves several steps.
What else can Hypospadias be?
Conditions related to:
- Abnormalities of the genital organs
- Conditions causing abnormal sexual development
What to expect with Hypospadias
The outlook for the condition known as hypospadias, a birth defect in males where the pee hole is not at the tip of the penis, has greatly improved over the last 30 years. Earlier treatments were not ideal due to lacking technical abilities, incomplete understanding of the anatomy and poor timing of the surgery.
Research from the last two decades suggests that short term results are good, but long term results are more uncertain. Many adults continue to face psychological challenges related to how their genitals look after surgery, and others continue to experience unsatisfactory sexual lives.
New techniques for treating hypospadias keep emerging, with the use of tissue glues and laser devices leading to improved and quicker healing of wounds. However, it’s crucial to remember that this condition can significantly impact a person’s mental well-being. So, long term monitoring and support are key.
Possible Complications When Diagnosed with Hypospadias
As people get older, they tend to have a higher chance of experiencing complications after surgery. For best results in treating hypospadias (a birth defect where the opening of the urethra is on the underside of the penis), it is optimal to have a medical team experienced in this condition. Right after the surgery, it’s normal to see some swelling and a little bit of blood. But if there’s a lot of blood, the patient might need to go back into the operating room. Infections almost never happen.
One of the main things to watch out for in the long run is the development of urethrocutaneous fistulas (an abnormal connection between the urethra and the skin). These are less likely to occur when the entire surgery is done at once. It’s rare for these fistulas to close on their own, so they may require surgical closure using a skin flap. It’s important, though, to make sure no hair-bearing skin is used for this procedure because it could lead to recurrent urinary tract infections and an area prone to stone formation. Unfortunately, it is common for the fistula to come back, even after it has been repaired. Other potential complications after the operation include narrowing of the opening of the urethra (meatal stenosis), a stricture/obstruction in the urethra (urethral strictures), a pouch forming in the urethra (urethral diverticula) and difficulties with erection (erectile dysfunction).
Post-Surgery Effects:
- Swelling
- Minor blood spotting
- Potential necessity to return to the operating room if there’s severe bleeding
- Low chance of infection
- Possible development of urethrocutaneous fistulas
- Likelihood of fistula recurrence
- Potential for urinary tract infection and stone formation if a hair-bearing skin flap is used
- Possible narrowing of the opening of the urethra
- Potential for an obstruction in the urethra
- Chances of a pouch forming in the urethra
- Difficulty maintaining an erection