What is Hypothalamic Hamartoma?
Hypothalamic hamartomas are a type of birth defect that results in harmless growths, or lesions, in a part of the brain called the hypothalamus. These occur while the fetus is developing in the womb. There are two main types of these growths, categorized by where they are found in the brain.
The first type is found inside the hypothalamus, connecting to a part of the brain called the posterior hypothalamus and another part called the third ventricle. This type of growth is often found near the mamillary bodies, which are small round areas in the brain. They commonly lead to a specific type of seizure called gelastic seizures.
The second type of growth is located next to the hypothalamus, near the anterior hypothalamus, tuber cinereum or the pituitary stalk. This type only attaches to the bottom part of the third ventricle. It often leads to early puberty because they cause an increase in the release of gonadotropin-releasing hormone (GnRH), a hormone that triggers the process of puberty.
These growths typically lead to several difficulties over time, including different types of seizures, a decline in cognitive abilities (thinking, learning, and memory), and mental health symptoms.
What Causes Hypothalamic Hamartoma?
Hypothalamic hamartomas, which are rare abnormalities in the part of the brain known as the hypothalamus, typically occur randomly without any connection to other birth defects or family history. In fact, about 95% of these cases occur spontaneously. However, 5% of the cases are linked with Pallister-Hall syndrome, a condition that affects the hands, feet, voice box, anal area and the hypothalamus.
Pallister-Hall syndrome is related to a change or mutation in a gene known as GLI3. This gene is involved in a complex series of reactions within cells (an “intracellular pathway”) known as the sonic hedgehog pathway, which helps regulate the way our bodies grow and develop. About a quarter of people with hypothalamic hamartomas not linked to Pallister-Hall syndrome also show this same GLI3 mutation. In fact, somatic mutations, which are genetic changes that happen after conception and can affect certain parts of the body, are found in 40% of patients.
Risk Factors and Frequency for Hypothalamic Hamartoma
Hypothalamic hamartoma, a rare condition, mostly affects around 1 in every 100,000 children and is slightly more common in boys (with a ratio of 1.3 to 1). It doesn’t favor any particular region or ethnic group. So far, no risks associated with the mother or exposures during fetal development have been found.
Signs and Symptoms of Hypothalamic Hamartoma
Hypothalamic hamartomas are medical conditions that can manifest in two main ways: epilepsy with related neurobehavioral symptoms or early onset of puberty, also known as central precocious puberty.
For those with epilepsy, the most common sign is gelastic seizures – a type of epilepsy that makes the patient have sudden bursts of laughter. These seizures typically begin during infancy. Additionally, they may experience developmental delays, cognitive decline, and psychiatric symptoms. It’s worth noting that about 40% of individuals experiencing these symptoms exhibit premature puberty. The presence of both symptoms tends to point towards larger lesions as revealed by magnetic resonance imaging (MRI) scans. The seizures often start at around one year of age and usually disappear by the age of ten. Other types of seizures may also occur. About 75% of people with this condition experience very debilitating seizures, like tonic-clonic seizures, complex partial seizures, drop attacks, and atypical absences. There have been cases where patients have seizures that mimic crying, known as dacrystic seizures. Exceptionally, a patient may have gelastic seizures without a hypothalamic hamartoma. In such cases, the seizures are usually attributed to a lesion in the frontal or temporal lobe.
It’s also common for patients with hypothalamic hamartomas and epilepsy to exhibit cognitive deficits. These individuals may struggle with short-term memory, slower processing speeds, or diminished intellectual capabilities. The cognitive impairment seems to be worsened by a higher number of antiepileptic medications, bigger hamartomas, an earlier onset of seizures, and a higher frequency of seizures. Psychiatric symptoms, such as oppositional defiant disorder, attention-deficit/hyperactivity disorder, conduct disorder, or mood disorder, are also common. Sadly, for most patients, these symptoms tend to worsen over time.
On the other hand, some patients do not exhibit the abovementioned symptoms of epilepsy but present with signs of early onset of puberty. These symptoms may include growth spurts, breast development, pubic hair growth, sexual organ maturation, voice deepening, and acne. It’s considered precocious puberty if these symptoms start before the age of 8 in girls and 9 in boys. The occurrence of these symptoms can sometimes be as early as one year of age. The lesions in these cases are usually attached to the anterior portion of the hypothalamus.
Testing for Hypothalamic Hamartoma
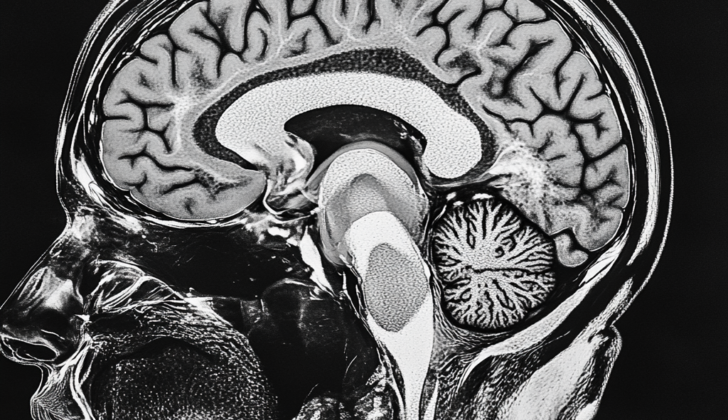
Brain MRI tests, with or without a special dye, are the go-to method for diagnosing hypothalamic hamartomas, a type of brain tumor. It’s vital to let the radiologist know they need to focus the imaging around the hypothalamus (a small area near the middle of the brain) to avoid missing the tumor. These tumors stand out in the pictures because they look less bright on T1 weighted images and more bright on T2 weighted images if we compare them to regular grey matter in the brain. This brighter appearance on T2 images is linked to a higher concentration of glial cells (a type of nerve cell). Additionally, these tumors could be associated with the presence of arachnoid cysts (fluid-filled sacs). So far, doctors are not sure whether these cysts grow inside or outside the tumor. Hypothalamic hamartomas don’t get bigger; they just expand as the brain grows, meaning their size compared to the brain remains the same.
A CT scan of the head might show a small lesion near the spaces filled with fluid in the brain, appearing similar in density to the brain. However, this method is no longer considered as reliable for detecting hypothalamic hamartomas and also exposes patients to unnecessary radiation.
Electroencephalography (EEG) tests, which monitor the electrical activity of the brain, usually show normal results during episodes of gelastic seizures (fits of uncontrollable laughter), which are a common symptom of hypothalamic hamartomas. However, the EEG could show signs of abnormal activity when other types of seizures are present. Continuous 24-hour EEG monitoring can record patients’ laughter spells, but don’t show any abnormal electrical activity during the seizure. In fact, some patients with hypothalamic hamartomas have been found to have these seizures originating from the tumors themselves, as seen with the use of depth electrodes (thin wires inserted into the brain).
Imaging techniques like single-photon emission computed tomography show increased blood flow to the hamartoma (tumor) after a gelastic seizure and normal blood flow during calmer periods. Specialists might employ magnetic resonance spectroscopy, a special type of MRI, showing a lower NAA/Cr ratio in patients with hamartomas compared to a healthy hypothalamus. This suggests an increased amount of scarring and a decrease in nerve cell concentration in hypothalamic hamartomas.
Treatment Options for Hypothalamic Hamartoma
The best way to address a medical issue will depend on the unique circumstances of each patient, including symptoms and the exact features of the condition. For example, if a patient is experiencing very minor seizures that don’t disrupt their life, it might be best to simply watch and wait. In some cases, surgery might be necessary to prevent seizures from affecting other parts of the brain.
Anti-epileptic medications are often used to control different types of seizures such as tonic-clonic seizures, complex partial seizures, drop attacks, and unusual gaps in consciousness. However, these medications typically don’t help control gelastic seizures (which are seizures involving sudden bursts of laughter). Seizures related to hypothalamic hamartomas (a rare benign brain tumor) are especially unresponsive to these medications, so surgery is often recommended for these cases.
When a patient experiences precocious puberty (i.e., puberty occurring at an unusually early age), it can usually be successfully treated with medications. One such medication is leuprolide acetate, which suppresses the body’s natural release of gonadotropin-releasing hormone (GnRH), which triggers puberty. This medication is usually injected once a month for as long as needed to keep puberty at bay.
The gold standard or the most effective treatment for hypothalamic hamartomas is complete surgical removal of the tumor. This treatment is most successful at stopping seizures and alleviating issues with cognition, behavior, and mood. The best approach to surgery will depend on factors like the size and location of the tumor and the patient’s age. The most common approach is removing the tumor via craniotomy (a procedure that involves creating an opening in the skull). This difficult procedure involves identifying and separating the tumor from other critical brain structures.
Another treatment option is Gamma knife radiosurgery (GKR), a non-invasive technique that damages the tumor. The exact mechanism by which GKR controls seizures isn’t fully understood, but it does not seem to cause necrosis or cell death in the tumor. This procedure can take significant time to produce effects, ranging from 6 months to 3 years. Nonetheless, it can completely eliminate seizures in 40% of treated patients, making it a good alternative treatment for small and medium-sized tumors.
Another method is stereotactic thermoablation, in which the tumor is heated to damage the tissue and stop it from causing seizures. Larger tumors might require multiple treatments. There are a couple of specific methods, such as radiofrequency thermoablation and laser-mediated ablation, which can control seizures in a significant number of cases.
What else can Hypothalamic Hamartoma be?
When diagnosing hypothalamic hamartomas, tumors found in the same region of the brain may cause similar symptoms. These should be ruled out by the physician:
- Craniopharyngioma
- Astrocytoma
- Optic glioma
- Meningioma
It’s important to note that while these tumors don’t trigger what are known as “gelastic seizures” (laughing seizures), they can disrupt the brain’s network that controls our hormones, leading to early onset of puberty.
What to expect with Hypothalamic Hamartoma
Surgery can potentially reduce the frequency of seizures by up to 90%. Gamma Knife Radiosurgery (GKR), a non-invasive procedure, results in complete stop of seizures in 40% of patients. Similarly, Radiofrequency thermoablation, another surgical method, can control seizures in up to 71% of patients. Likewise, Laser-mediated thermoablation reduces seizures in 67% of the patients.
Leuprolide acetate, a medicine, is used to delay early onset of puberty until the child reaches the right age. After reaching the appropriate age, the use of this medicine is then stopped.
Unusually, antiepileptic medications, which are usually prescribed to control seizures, do not seem to work well on gelastic seizures, a type of laughter-provoking seizure, and are also less effective in controlling other types of seizures.
Larger hamartomas (benign brain tumors), higher number of antiepileptic medications used, earlier age of seizure onset, and more frequent seizures can lead to greater cognitive impairment, affecting a person’s ability to think, remember, and make decisions.
Possible Complications When Diagnosed with Hypothalamic Hamartoma
Hypothalamic hamartomas can cause a variety of system-wide complications:
- Multiple types of disabling seizures (such as tonic-clonic seizures, complex partial seizures, and drop attacks)
- Cognitive decline
- Mental health issues (like oppositional defiant disorder, attention-deficit/hyperactivity disorder, conduct disorder, and mood disorder)
- Delayed development
- Short-term memory problems
- Slower processing speed
- Diminished intellectual ability
- Short stature
- Acne
Treatment for hypothalamic hamartomas may also present complications:
- Surgical measures may result in diabetes insipidus, meningitis, stroke, infection, bleeding, and short-term memory deficits
- SRS, or Stereotactic Radiosurgery, oftentimes provides a slow treatment response, leaving patients at risk of persistent seizures for upwards of three years
- Thermoablation may cause injury to the structures of the nervous system and blood vessels, issues with temperature control, excessive eating (hyperphagia), low sodium levels (hyponatremia), Horner syndrome, and memory loss (amnesia)
Preventing Hypothalamic Hamartoma
Parents of the patient need to understand the cause, symptoms, and likely outcome of hypothalamic hamartomas. A hypothalamic hamartoma is a rare, non-cancerous brain tumor affecting children and adults. Various treatment options are available, and parents need to know the risks and benefits of each. This knowledge is crucial in making informed decisions for their child. The treatments that are considered ‘invasive’ (meaning, they involve surgery or procedures inside the body) are typically the best options for preventing seizures, and they are highly recommended.
It’s important for parents to know that hypothalamic hamartomas are benign, or non-cancerous. They won’t turn cancerous or spread to other parts of the body. Also, the child should still be able to go through puberty normally even after the use of GnRH agonists (medications that affect hormone levels), and grow up normally after surgical or other treatments. If a chosen treatment doesn’t work, the child may continue to have destructive seizures and a decrease in brain function, along with increasing difficulties with psychological health. That’s why it may be necessary to try a combination of treatments.