What is Prune Belly Syndrome?
Prune belly syndrome, also known as Eagle-Barrett syndrome or the triad syndrome, is an uncommon birth disorder that is marked by three main characteristics: lack of abdominal muscles, undescended testicles (called cryptorchidism), and problems with the urinary tract. This condition can vary widely in its impact on those who have it, ranging from being life-threatening to allowing a normal lifespan and the ability to have children.
Whether someone with this syndrome lives, and how well they live, usually depends on how badly their kidneys were formed before birth (a condition known as renal dysplasia). Studies conducted recently show that 10 to 25% of babies with prune belly syndrome do not survive past birth, and this mortality rate is directly linked to how underdeveloped the baby’s lungs are (a condition known as pulmonary hypoplasia). This underdevelopment is often a result of low levels of amniotic fluid (known as oligohydramnios), which occurs because of reduced urine production from the problems with the kidney and urinary tract. This leads to a condition called Potter sequence.
What Causes Prune Belly Syndrome?
The exact cause of prune belly syndrome is still not clear, but there are several theories. One theory suggests that it might be due to an issue with the tube that carries urine from the bladder out of the body (the urethra) during early development inside the womb. This obstruction could cause the bladder to expand abnormally, affecting the development of the urinary tract, abdomen, and how the testicles descend.
Another theory believes that prune belly syndrome might be due to a problem with the yolk sac, a structure that nourishes the embryo in the earliest stages of growth. There’s also a theory that suggests that a defect in a specific layer of cells in the embryo, which normally develops into the ureters (tubes connecting kidney to bladder), bladder, prostate, urethra (passage for urine to exit the body), and gubernaculum (cord aiding in the descent of the testicles), could be the cause.
No single theory is universally accepted and some researchers think that more than one might combine to cause prune belly syndrome. Researchers are also exploring if the condition could be genetic, even though it’s not confirmed yet.
Risk Factors and Frequency for Prune Belly Syndrome
Prune belly syndrome is a condition that occurs in around 3.6 to 3.8 of every 100,000 live male births. It is considerably more common in males, with less than 5% of diagnosed cases being female. However, female patients with this syndrome will still show the usual urinary tract issues and characteristic abdomen appearance associated with prune belly syndrome.
Signs and Symptoms of Prune Belly Syndrome
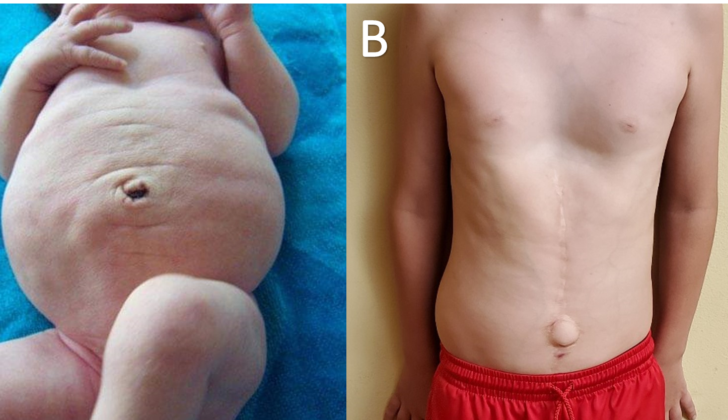
Prune belly syndrome is a condition known for its most visible physical sign: a wrinkled, dried-up, prune-like appearance of the belly. This is believed to be due to either weak or even entirely absent muscles in the abdomen. As children with this syndrome get older, they start to have more body fat in the abdomen, which can actually lessen this wrinkled look. This typically happens during their first year of life where their belly starts to look more like a potbelly due to the lacking underlying muscles.
Despite the weakness in their abdominal muscles, these children usually walk normally, but they might reach certain physical milestones, like starting to walk, a bit later than usual. Also, most patients with this condition tend to sit up by rolling to their sides and using their arms to push up from a lying down position. In some cases, the patients may also have an excessive inward curve of the spine, known as lordosis.
Testing for Prune Belly Syndrome
During the second three months of pregnancy, it might be possible to detect signs of a condition known as prune belly syndrome through an ultrasound. This test might show that there’s less amniotic fluid around the baby, which is called oligohydramnios. The ultrasound could also show problems with the baby’s urinary tract, such as a large bladder, widened tubes leading from the kidneys to the bladder (ureters), fluid-filled swelling in the kidneys (hydronephrosis), or an undeveloped or missing muscle in the abdomen.
If the baby has severe kidney problems (renal dysplasia), it’s common to find underdeveloped lungs (pulmonary hypoplasia). Such babies are either stillborn or die shortly after birth. They typically need urgent medical attention and help to breathe with a ventilation machine. A chest X-ray can assess the condition of the lungs, which will usually appear small and underdeveloped. It’s also necessary to run tests on the baby’s kidneys to assess their functionality.
Once the baby is stable, doctors can use ultrasound imaging to take a closer look at the kidneys and bladder. This could reveal a large bladder with a significant amount of urine leftover after urination due to weak bladder contractions. An early test to examine the bladder’s function (voiding cystourethrogram, or VCUG) can check for abnormalities such as urine flowing backwards from the bladder into the kidneys (vesicoureteral reflux, or VUR). It can also provide important information about the bladder’s outlet and emptying ability. Other findings could include a wide bladder neck and irregularities in the tube that carries urine out of the body (urethra).
A urodynamic study, which tests how well the bladder, sphincters, and urethra are storing and releasing urine, may suggest poor bladder muscle movement. Heart and abdomen screenings, which could include ultrasounds and contrasting x-rays, are done to assess the baby for any heart or gastrointestinal irregularities.
Treatment Options for Prune Belly Syndrome
If a child is born with prune belly syndrome, there’s a high chance (almost 80%) that they’ll experience a urinary tract infection at least once, with one in three of these children likely to develop a kidney infection. This susceptibility to infection is because children with this condition often have issues with their urinary system, such as urine refluxing from the bladder back to the kidneys, difficulties emptying the bladder completely, and weak urine flow. To reduce the chance of urinary infections, doctors often recommend preventive antibiotics and the consideration of circumcision.
Constipation is also common in children with prune belly syndrome because the weak abdominal muscles can make it hard for them to pass stools. Long-term constipation can increase the risk of urinary infections. In addition, these weak muscles can also cause an ineffective cough, which can make these children more vulnerable to respiratory infections that may require antibiotics.
In very severe cases where kidney function is severely reduced, a kidney replacement therapy may be needed.
The types of surgeries a child with prune belly syndrome might need include orchiopexy, urinary tract procedures, and abdominal wall reconstruction. The best timing and sequence of these surgeries will vary for each child, depending on the specifics of their condition and any other health problems they might have.
Orchiopexy is a surgery that’s usually recommended for boys with prune belly syndrome, and it should ideally be done around six months of age. This procedure corrects undescended testes, helping to preserve their function.
The need for urinary tract surgeries varies. Some experts believe that early surgery can improve kidney function by reducing the problems of urine reflux and weak urine flow. Others prefer to wait, closely monitoring the child for any improvements in these issues. Urinary tract surgeries are strongly recommended for children who frequently have high-temperature urinary infections or whose kidney function is worsening.
Lastly, children with visibly weak abdominal muscles may require an abdominal wall reconstruction. Often, this surgery is performed along with orchiopexy or urinary tract procedures. Apart from improving the child’s appearance, this operation can improve muscle tone, potentially aiding bladder emptying.
What else can Prune Belly Syndrome be?
Typically, the distinct set of symptoms and a specific physical finding in the abdomen make it easy to identify Prune Belly Syndrome, so doctors often don’t need to differentiate it from other conditions. But it’s still critical to figure out how severe the urinary tract problems are and what might be causing them. Doctors must also take into account all other health issues that can occur alongside Prune Belly Syndrome that aren’t part of the main three symptoms.
In some cases, patients may have the common urinary tract abnormalities seen in Prune Belly Syndrome but either their testes might be in the normal place (or just one might be undescended) or their abdomen might look normal (or may be only partially/unilaterally loose). This condition is referred to as pseudo-prune belly syndrome, which is essentially the same thing as megacystis-megaureter syndrome.
What to expect with Prune Belly Syndrome
As previously discussed, the outcomes for children born with prune belly syndrome can widely vary. Some may not be able to survive, whilst others may lead a healthy, normal life. Studies have found that between 10 to 25% of newborns with this condition do not survive, with premature birth and severity of underdeveloped lungs, often a direct result of urinary tract abnormalities, contributing to this statistic. Additionally, around 40% of these children born prematurely and almost half require assistance with breathing at birth. Furthermore, one in four may also have a congenital heart defect.
Prune belly syndrome is categorized into three groups based on their clinical characteristics. The first group, accounting for 20% of patients, has severe underdevelopment of the kidneys and lungs and most are either stillborn or die shortly after birth. The second group, about 40% of patients, have kidney function that is acceptable at birth but may experience deteriorating kidney function later in life due to significant kidney abnormalities, and may need aggressive treatment. The third group, also about 40%, have the best prognosis with normal kidney function despite slight urinary tract abnormalities and can lead a life that is almost normal.
Before 1992, men diagnosed with prune belly syndrome were believed to be infertile, as there were no recorded cases of a male patient fathering a child. This infertility was thought to primarily result from undescended testes, as well as other issues like an ineffective bladder neck which can lead to a disorder called retrograde ejaculation and underdevelopment of the prostate. However, due to advancements in treatments such as surgery to reposition the undescended testes, sperm retrieval techniques, and sperm injection, several men with prune belly syndrome have been able to become fathers.
Prune belly syndrome is very rare in females, with only 5% of diagnoses relating to this demography. Women with this condition typically only have an underdeveloped abdominal wall and abnormal urinary tract, with no abnormalities in the sex organs. There is limited information regarding fertility prospects for women with prune belly syndrome, however, there has been a reported case of a normal pregnancy and vaginal birth in a woman with this condition.
Possible Complications When Diagnosed with Prune Belly Syndrome
Given the complexity of the possible effects on various organ systems, there can be numerous potential complications. However, the most critical ones are those that doctors can significantly influence and improve outcomes.
In severe cases, complications typically involve underdeveloped lungs and kidney malformation. These complications require a team of various specialists to manage, including experts in maternal-fetal medicine, neonatal care, urology, nephrology, genetics, pulmonology, anesthesiology, and more. It is crucial to keep families well-informed about the baby’s condition, possible outcomes, and help them make informed decisions. Experienced specialists should address all ethical considerations.
Complications related to the urinary tract are common after the newborn period, with about a third of patients eventually needing a kidney transplant. A study of 35 patients with prune belly syndrome showed that having irregular kidneys, a low nadir creatinine (a component of blood used to evaluate kidney function), and kidney infection were indicators of a worse prognosis. Early diagnosis is of great importance, especially if the key symptoms are not present. It’s also imperative to consult a urologist for a detailed evaluation of any urinary tract blockages and to prevent further complications. Measures such as antibiotic prophylaxis and circumcision may be planned to prevent urinary tract infections.
Key Points:
- Complications may affect various organ systems
- Severe cases may include complications like underdeveloped lungs and kidney malfunction
- Various specialists manage these complications
- Families should be kept well-informed and involved in decision-making
- Urinary tract complications are common after newborn period
- Early diagnosis is essential
- Measures may be taken to prevent complications
Preventing Prune Belly Syndrome
Prune belly syndrome is a condition that doesn’t have a known cause. Since we don’t know what causes it, there aren’t any specific steps you can take to prevent it.