What is Spina Bifida?
Spina Bifida is a birth defect that happens due to incomplete formation of the spinal cord’s protective lining. The term is often referred to generally about any level of incomplete spinal cord development. It can be categorized into two forms: spina bifida occulta and spina bifida aperta.
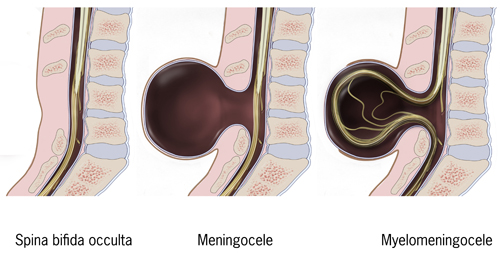
Spina bifida occulta, also known as closed spinal dysraphism, is the most mild form. It involves a hidden defect in the spine and minimal impact on the nerves. On the other hand, spina bifida aperta, or open spinal dysraphism, describes a condition where nerve tissues are exposed to the external environment. Examples are meningocele and myelomeningocele. The kind and severity of neurological effects vary depending on the extent of spinal cord development.
Spina bifida often comes with other developmental abnormalities, making it crucial to have a comprehensive healthcare plan for the best chance of survival and successful outcomes.
What Causes Spina Bifida?
Spinal dysraphisms are conditions where parts of the back do not join up completely while a baby is still in the womb. This is likely to happen between the 17th and 30th day of the baby’s development. The creation of the nerve system happens in two parts – firstly the brain and the upper section of the spinal cord, and secondly the lower part of the spinal cord. The incomplete development and joining of the lower part of the spinal cord can result in various types of spinal dysraphisms.
Problems with the development of the spinal cord tube are thought to be caused by both environmental and genetic influences. A common environmental cause is a lack of folate – most cases can be improved by increasing folate intake. Because of this, many countries have started adding folate to certain foods, which has reduced spinal dysraphisms and anencephaly (a serious birth defect of the brain) by 28%. Other risks include the mother being overweight, having diabetes, or taking certain types of medication, like valproic acid. This medication is thought to be particularly risky, increasing the chance of problems by around ten times. Various genetic issues have also been linked to poor spinal cord development, including abnormalities of chromosomes and issues with specific genes. In particular, research has suggested that polymorphism (when a gene can exist in multiple forms) of the MTHFR gene, which is involved in processing folate, is a probable genetic risk factor. While these problems usually occur on their own, sometimes they can be associated with abnormalities in the baby’s chromosomes, most often Trisomy 13 and 18 (chromosomal disorders).
Risk Factors and Frequency for Spina Bifida
The frequency of neural tube defects (NTDs), like spina bifida, has changed over time. However, overall it has been reduced due to increased early detection during pregnancy and other prevention programs. Between 1999 and 2007, in the U.S. there was an average of 3.17 cases of spina bifida for every 10,000 live births. Research shows that about 1,300 babies born healthily each year wouldn’t have been if folic acid use during pregnancy hadn’t become common.
- Hispanic women seem to be more likely to have pregnancies affected by NTDs.
- Across the globe, Hispanic people have higher rates of these conditions (3.8 cases per 10,000 live births).
- Non-Hispanic Blacks or African Americans have a lower rate of 2.73/10,000.
- Non-Hispanic whites have a rate of 3.09/10,000.
The risk of NTDs recurring increases with a family history of these conditions, geographical location, and the severity of the defect. The chances of having another child with an NTD increase to about 3-8% after one pregnancy is affected, or if the mother has a history of the defect. The risk becomes higher with an increased number of affected children.
Signs and Symptoms of Spina Bifida
Neural tube defects (NTDs) are conditions that should ideally be identified during prenatal screenings. Affected women, particularly those in underserved communities or from low socioeconomic backgrounds, should be given advice before they conceive to help improve the outcomes. However, sometimes these screenings aren’t accessible, so these conditions might only get detected at birth or while the child is still in infancy.
The standard test for NTDs during pregnancy involves measuring AFP levels in the serum between the 16th and 18th weeks. This is then followed up with an ultrasound, which has an 88-89% success rate at detecting these conditions. Due to the numerous variations of neural tube defects, there are a wide range of symptoms that patients might present with.
Physically examining the lower regions of the spine can be a useful way to tell if a patient has either an “open” or “closed” spinal dysraphism. Spina bifida occulta, for example, won’t show any obvious signs of deformation. However, there may occasionally be a hairy patch of skin or a dimple where we would expect to see a spinal defect. On the other hand, meningocele involves a defect that allows the meninges and cerebrospinal fluid (CSF) but not neural elements to push through the posterior part of the spine. Myelomeningocele is more serious, causing the meninges, CSF, and functional neural components, such as nerves or spinal cord, to extrude. This usually leads to greater future limitations because the nervous tissue is involved in the defect.
- Signs of muscle stiffness or tightness (spasticity)
- Pain
- Motor defects
- Issues with bowel and/or bladder control
- Cognitive defects
- Seizures
- Precocious puberty or other endocrine disorders
These neurological dysfunctions are particularly common in open dysraphisms, such as with a meningocele and myelomeningocele, where neural tissue can protrude outside of the defect and become affected. Interestingly, it’s also common to see latex allergies in these patients, appearing in between 10% and 73% of people with NTDs. As soon as any of these symptoms are noticed, it’s important to get a full history of their pregnancy, birth, and family. This can help identify possible contributing factors and provide valuable knowledge for family counselling.
Testing for Spina Bifida
For women, routine screening is advised to detect Neural Tube Defects (NTDs) – birth defects of the brain, spine, or spinal cord – at an early stage. This helps in planning treatments and providing the necessary advice for the woman. This screening usually starts with a blood test known as ‘serum AFP’. In cases where there’s a strong reason to suspect NTDs, a procedure called ‘amniocentesis’ might be carried out. This involves drawing a small amount of fluid from the sac surrounding the baby inside the mother’s womb.
However, due to the risks associated with amniocentesis, and the accurate results ultrasound can provide, ultrasound has become the recommended method for diagnosing NTDs while the baby is still in the womb. During an ultrasound, different signs may indicate the presence of an NTD.
Some of these signs include the ‘lemon sign’ and the ‘banana sign’. The lemon sign refers to a particular overlap of bones in the front of the baby’s head, caused by shifting of contents within the skull. The banana sign refers to a curved shape of the baby’s cerebellum, the part of the brain that controls balance, caused by it being displaced downwards. This is often linked to a condition that the baby may have at birth called Arnold-Chiari II malformation.
Changes in the fluid-filled spaces within the brain, even without the presence of a condition known as hydrocephalus (a buildup of fluid in the brain), can also be seen on the ultrasound. The ultrasound scan can continue down the spine to find out which parts of the spine are affected, and this can help predict how the defect might affect the baby’s bowel movements, bladder control, and ability to walk.
In about 60% of cases, the level of the spine affected seen in the ultrasound matches with the functional level after the baby is born. In cases where more detail is needed, a Magnetic Resonance Imaging (MRI) can be conducted after the baby is born. This can predict the level of the spinal defect within one to two parts of spinal bone in about 89% of the cases.
Treatment Options for Spina Bifida
When it comes to neural tube defects (NTDs), such as spina bifida, the best course of action is prevention. This is particularly important for women who are of childbearing age. It’s recommended that they include a vitamin, folate, in their diet, which is known to prevent NTDs. To assist with this, the U.S made fortifying grains with a form of folate, called folic acid, mandatory to reduce the number of NTD cases. Any woman planning pregnancy should consume 0.4mg of folic acid daily before conception, and those with a personal or family history of NTDs should take a higher dosage, 4mg of folic acid daily.
When it comes to living with spina bifida, most people with the milder form, spina bifida occulta, won’t require surgery. But for more severe or ‘open’ forms of this condition, several surgical options can alleviate the neurological effects. In some cases, surgery can be performed on the fetus while still in the womb to prevent future complications. The fetus must meet certain criteria for this high-risk procedure, such as being between 19-25 weeks old and having specific types of malformations. While this kind of surgery can reduce some future complications, it does also increase the risk of premature birth and serious complications for the mother.
When a newborn has spina bifida, doctors usually perform surgery within the first 72 hours to minimize the risk of infection and neurological decline. After surgery, the child is likely to need additional treatments, such as a ventriculoperitoneal shunt, a device to drain excess cerebrospinal fluid from the brain, to manage a side effect of spina bifida known as hydrocephalus or ‘water on the brain’. Other conditions associated with spina bifida, like Arnold Chiari malformations (a condition where brain tissue extends into the spinal canal), may also require treatment.
Managing spina bifida usually involves a whole team of doctors, as it can involve many different parts of the body. Often, the condition affects the nerves controlling the bladder and bowel, which can lead to incontinence or even, with poor management, renal (kidney) failure. Regular monitoring with renal ultrasounds every six months, and sometimes needing to use a catheter for urination, are common parts of long-term management. Learning to manage bowel movements with stool softeners, motility agents (which help the bowel to move stool along), and digital stimulation (stimulation with a finger) can help to achieve good control.
For children with NTDs, having weakness, low muscle tone (flaccidity), stiffness (spasticity), and joint stiffness (contractures) are quite common, affecting many different functions such as walking and hygiene. Certain surgical procedures to lengthen tendons can be considered if severe contractures affect these functions. Furthermore, foot deformities, such as clubfoot, flatfoot, and rocker bottom foot, are often seen in children with NTDs. These can be managed by splints, physical therapy, and a procedure called serial casting which involves periodic placement of plaster casts to gently stretch the muscles and tendons over time.
What else can Spina Bifida be?
The detection of spina bifida usually relies on the signs and symptoms shown by the patient. However, in some instances where these signs aren’t clear enough or the X-ray results are ambiguous, doctors might need to consider other medical conditions that could potentially explain the symptoms. These conditions might include:
- Compression of the spinal cord
- Diastematomyelia (a split down the middle of the spine)
- Chiari malformations that occur without any other related conditions
- Tumors or other masses in the spine
- A spinal cord that is stuck or “tethered” and can’t move freely
These alternative diagnoses need to be carefully considered to ensure the patient receives the correct treatment.
What to expect with Spina Bifida
There haven’t been many recent long-term studies on spina bifida, a birth defect where there is incomplete closing of the backbone and membranes around the spinal cord, which makes it hard to predict patient outcomes. This is especially true given the improvements in how we manage spina bifida. Many studies also mix data from patients with both types of this condition: open and closed dysraphisms.
The outcomes for people with spina bifida largely depends on whether they have excess fluid in the brain (hydrocephalus), where their defect is located on the spine, and the severity of a condition called Chiari malformation, which affects how the brain and spinal cord connect. A recent study found that overall, about 71% of children with spina bifida lived to their first birthday. Of those with and without hydrocephalus, 56% and 88% lived past one year old, respectively. The survival rates decrease slightly for those with hydrocephalus as they get older, to about 50% by age 20. Most deaths after age 5 are due to seizures, blood clots in the lungs (pulmonary emboli), hydrocephalus, and serious kidney disease or severe infections (sepsis).
However, there might be significant health problems related to neural tube defects (NTDs), if patients aren’t well cared for. The most common issue for those with this condition is urinary tract infections because their bladder might not work properly due to nerve damage. This affects about 48% of patients with about 6% ultimately ending up with kidney failure.
The severity of Chiari malformation can greatly affect a newborn with NTDs and can lead to several problems like sleep apnea, paralysis of the vocal cords, and slower than usual heart rate (bradycardia).
Patients often worry about how well they’ll be able to walk (ambulate). In a study called the Management of Myelomeningocele Study (MOMS), only 7% of the participants depended on a wheelchair to get around. The rest could walk with the help of devices and about 29% were fully independent.
Possible Complications When Diagnosed with Spina Bifida
Patients experiencing post-operation complications include, but are not limited to, acute kidney failure and urosepsis (infection in the bloodstream often due to urinary tract infections), scoliosis, chronic pain, epilepsy, tethered spinal cords or a medical condition called hydromyelia. It’s important to address urinary function issues quickly and thoroughly. Many patients may need help emptying their bladder regularly via a catheter. Other potential complications are heightened risk of fractures, usually due to conditions like osteopenia (a precursor to osteoporosis), contractures (muscle stiffness), decreased sensation, and immobilization. Another unusual but significant complication is a latex allergy, a common problem amongst patients with spina bifida.
Common Complications:
- Acute kidney failure
- Urosepsis
- Scoliosis (affects around 33% of patients)
- Chronic pain (affects around 29% of patients)
- Epilepsy (affects around 12% of patients)
- Tethered spinal cords or hydromyelia
- Increased fracture risk
- Latex allergy (Between 10% and 73% of patients with spina bifida have this)
Recovery from Spina Bifida
Starting rehabilitation as soon as possible can greatly help improve one’s health and quality of life. This early intervention can involve moving and stretching to help patients remain flexible and ready for normal activities such as walking, taking care of oneself, or doing daily tasks. The symptoms and level of motor control (ability to move specific muscles) can vary for each patient, meaning personalized therapy plans are crucial.
Most patients may need orthotics, which are devices that stabilize the joints, prevent physical disabilities, assist with walking, and generally improve function. To help with support, some patients may also require walking aids such as canes, walkers, or wheelchairs. Depending on the condition, some patients may also need help with their daily tasks.
Doing physical and occupational therapy over a long period can be beneficial. Some might also need speech therapy for issues like trouble swallowing (dysphagia), speech difficulties (dysarthria), vocal cord paralysis, and cognitive (thinking and understanding) training. Additionally, neuropsychology, the study of how the brain and the rest of the nervous system influence a person’s cognition and behaviors, can be really important, especially during adolescence, while adjusting to arising complications.
However, research shows that despite facing a number of potential complications, only 5% of patients experience depression.
Preventing Spina Bifida
Women who are of child-bearing age should be advised to take folic acid supplements to prevent Neural Tube Defects (NTDs), which are birth defects of the brain and spine. Women planning on getting pregnant should consume 0.4mg of folic acid every day, and if they have had a child with NTD before, or if there is a family history of NTD, they should take 4mg daily.
It’s important to provide useful information to caregivers in the early stages of their child’s life. This allows them to advocate effectively for their child’s needs. As the child grows, they can gradually participate more in their own care, based on their cognitive development. Both children and caregivers should feel like they’re part of the medical team involved in their care.
Training to families is crucial in managing their child’s condition as they grow. This includes learning how to move the patient safely, using medical aids such as orthotics (devices which support weak limbs) correctly, and maintaining good body posture. It’s also important to learn about warning signs and symptoms of serious issues that could develop, such as a urinary tract infection (UTI), fluid buildup in the brain (hydrocephalus), or seizures.
Once kids are old enough to understand their health condition, they should be included in making decisions about their care, and be educated about their own self-care. Some patients with spina bifida occulta, a mild form of spina bifida, may not have many associated health problems, but those with more severe forms may require closer monitoring and may need to learn skills like self-catheterization or manage their bowel program.
Walking (ambulation) is a common concern for these patients as they grow older. However, most patients can walk reasonably well, with only 7% needing to use a wheelchair.
It’s also essential to address the psychological aspects of patient’s health to encourage them to participate actively in their healthcare and get better outcomes. One study showed that cognitive behavioral therapy, a type of therapy that helps people manage their problems by changing the way they think and behave, can significantly improve outcomes in self-care, mental function, mood, and independence when used together with a high-intensity rehabilitation program.












