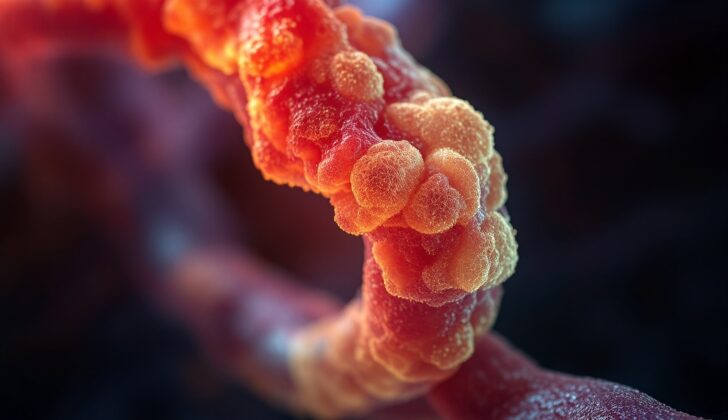
What is Biliary Duct Hamartoma?
“Von Meyenburg complexes” or multiple biliary duct hamartomas are rare, non-cancerous liver malformations, which are unusual formations in the liver that appear as small, dilated or swollen bile ducts. These were first identified in 1918 by a researcher named Von Meyenburg. Typically, these are discovered by chance during post-mortem examinations or during surgery for other conditions as they usually don’t cause any noticeable symptoms. They show up on scans as one or many small, cyst-like formations ranging from 0.05 cm to 1.5 cm in size. These formations can often be mistaken for liver cancer spreading or other significant health conditions on initial observation. This can lead to a detailed diagnostic process and even surgical procedures. Therefore, it’s crucial that specific imaging results or tissue sample evaluations are used to correctly diagnose these liver malformations.
What Causes Biliary Duct Hamartoma?
Biliary duct hamartomas, also known as Von Meyenburg complexes, are tiny, dilated channels found in the liver that weren’t correctly formed during embryo development. They are small (<5mm), present in multiple areas across the liver, and often described as resembling "a starry night."[8] They don't usually cause symptoms and generally don't lead to any serious health problems. They are most often discovered during surgery for another condition, through imaging tests, or in autopsies. The cause of these hamartomas is not known, but they're believed to occur when certain small ducts in the developing embryo do not form correctly.[9] Some research suggests that these hamartomas can become more common in damaged livers caused by long-term viral hepatitis or liver disease caused by alcohol, inflammation, or lack of blood flow. This suggests that environmental factors might be important in their development.[2][4][5] Additionally, they are more commonly found in people with polycystic (meaning many cysts) liver and kidney diseases or those with a disease called congenital hepatic fibrosis which causes scarring in the liver.[2]
Risk Factors and Frequency for Biliary Duct Hamartoma
Multiple biliary duct hamartomas are a medical condition that can be found in a small percentage of adults and children. These hamartomas are not very common, with rates ranging from 0.6% to 5.6% in adults observed at autopsy, and just 0.35% observed in needle biopsies for liver issues.
- About 0.9% of children suffer from this condition
- While it can be found in infants and children under two, it’s most commonly seen in people older than 35
- Interestingly, females suffer from this condition three times more than males
- According to one research, nearly 5% of people may have bile duct hamartomas
Signs and Symptoms of Biliary Duct Hamartoma
Most of the time, people who have this condition don’t show any symptoms and it’s usually discovered by chance during an operation for another issue. There’s not usually anything unusual discovered during a physical examination. However, on rare occasions, they might have symptoms such as fever, yellowing of the skin or eyes (jaundice), a swollen belly, or pain in the right upper abdomen or middle of the upper belly.
Abdominal pain is usually the first symptom to appear in people who do have symptoms. When doctors carry out physical examinations, although they usually appear normal, they sometimes find signs such as positive Murphy’s sign or tenderness when pressing in the right upper quadrant of the abdomen.
- Fever
- Jaundice (yellowing of the skin or eyes)
- Swollen belly
- Pain in the upper right abdomen or middle of the upper belly
- Positive Murphy’s sign (pain or tenderness when examining the right upper abdomen)
- Tenderness when pressing the right upper abdomen
Testing for Biliary Duct Hamartoma
Multiple biliary duct hamartomas are usually harmless findings that often do not require specific evaluation. However, while most patients with these hamartomas will show normal lab test results, some may show slightly high levels in liver function tests, specifically aspartate aminotransferase (AST), which is an enzyme that helps metabolize amino acids, and gamma-glutamyl transpeptidase (GGT), another enzyme present in the blood associated with liver functionality. A baseline level of a compound called CA 19-9, which can slightly increase with these hamartomas, is generally assessed. In some cases, patients may exhibit higher levels of bilirubin in the blood, lower albumin levels, and higher levels of C-reactive protein, a marker of inflammation.
These small growths are often discovered by accident during an ultrasound or a computed tomography (CT, a type of X-ray) scan done for another medical reason. On an ultrasound, they appear as various bright and dark areas within the liver, resembling the tail of a comet. CT scans depict them as multiple irregular cyst-like spots in the liver that are low in intensity and do not become brighter when contrast (a special dye used in imaging) is injected. However, for optimal detection, magnetic resonance imaging, or MRI, a technique that uses magnetic fields for creating detailed images of the body, is recommended. The hamartomas show up as multiple dark small to medium-sized cyst-like formations on T1-weighted images (a type of MRI image), and bright spots on T2-weighted images. These formations do not communicate with the bile ducts and do not change in appearance with the injection of gadolinium, a type of contrast used in MRIs.
The most unique MRI feature of these hamartomas is the presence of mural nodules, which are tissue projections appearing due to connective tissue partitions that are of equal intensity on T1-weighted images and increased intensity on T2-weighted images. The presence of these nodules can accurately diagnose these hamartomas and prevent misdiagnosis. Although they generally do not need to be biopsied to establish a diagnosis, many patients will undergo biopsies as part of the overall assessment. A biopsy, which involves taking a small sample of tissue for examination, is the most reliable way to rule out cancer.
Treatment Options for Biliary Duct Hamartoma
Multiple biliary duct hamartomas is a condition where small, benign (non-cancerous) growths form in the bile ducts of the liver. In general, this condition is harmless and does not cause any symptoms or long-term problems. Therefore, for most people, no treatment is needed.
However, because these growths may have a small chance of turning into cancer, it’s important to monitor them. This means having regular imaging tests, such as scans, to see if the growths have changed. Doctors may also recommend a liver biopsy (a procedure where a small piece of the liver is removed and tested) to make a diagnosis.
If there are changes to the growths, or if the patient shows warning signs – such as losing weight without trying – further examinations may be necessary. Additionally, if a patient’s levels of a specific protein called CA 19-9 (a tumor marker that could indicate cancer) rise from their usual levels, then further investigation is needed. If it’s then confirmed that the growths are cancerous and the area is operable (or suitable for surgery), doctors may recommend removing them through surgery.
What else can Biliary Duct Hamartoma be?
Multiple biliary duct hamartomas, which are benign growths in the liver, are often found unexpectedly during autopsy or medical imaging procedures. It’s important to correctly diagnose this condition since it closely mimics the appearance of metastatic disease, or cancer spreading to the liver. This resemblance is particularly important if the patient has malignant tumors elsewhere in the body.
Generally, liver metastases show fuzzy outlines with variable sizes on basic computed tomography (CT) scans and may look different with injected contrast dye. In contrast, bile duct hamartomas don’t tend to change with contrast dye, are usually of regular shape, and range from 1 mm to 15 mm in size.
Besides metastatic liver disease, multiple biliary duct hamartomas may also be mixed up with other liver conditions. Here’s how some of these can be distinguished:
- Bile duct adenomas: these have small rounded tubes with tiny hidden openings, while biliary duct hamartomas have widened openings with thick bile.
- Peribiliary cysts: these cysts are specifically located within connective tissue along the portal vein in the liver hilum, do not interact with the bile duct tree and usually get larger over time, compressing the biliary tree. This is contrasted with the varied scattering of biliary duct hamartomas.
- Microabscesses of the liver typically manifest as multiple round pockets of infected tissue which look less dense on CT scans. They typically occur in patients with suppressed immune systems, fever, and upper abdominal pain, which can be distinguished from bile duct hamartomas by signs of infection that are usually not seen with hamartomas.
- Caroli’s disease is characterized by widening of the intrahepatic bile ducts that communicate with the bile duct tree. It can be distinguished from bile duct hamartomas using MRCP, a type of imaging technique, by contrast enhancement with intravenous gadolinium, a type of contrast dye.
Surgical Treatment of Biliary Duct Hamartoma
This benign tumor, also known as a hamartoma, can often present a clinical challenge to surgeons and surgical oncologists who come across it during a surgical procedure intended for a different malignant (cancerous) condition. Typically, the doctor may take a small sample of liver tissue, known as a liver biopsy, for immediate examination or ‘frozen section’. The purpose is to rule out other serious conditions.
However, distinguishing between benign hamartomas and metastatic disease in the liver, which means the cancer has spread to the liver, can be tricky. If the pathologist, a doctor who specializes in detecting diseases by studying cells and tissues, is not familiar with this kind of benign tumor, they might mistakenly label it as metastatic carcinoma (a term for cancer that has spread) or Caroli’s disease, a rare congenital condition that enlarges the liver’s bile ducts.
Unlike Caroli’s disease, these benign hamartoma tumors do not connect with the liver’s bile ducts, and typically no treatment is required as it’s not harmful.
What to expect with Biliary Duct Hamartoma
Most people with this condition do not show any symptoms, so it’s often only found during an autopsy for patients who pass away from unrelated diseases. In these cases, the outlook is generally good. However, if the condition turns into cancer, the outlook is less positive, with a 5-year survival rate of 15% to 40%.
Some patients with widespread non-cancerous growths in their bile ducts may have consistently high liver function test results. These tests help doctors check how well their liver is working. If this happens, a liver transplant may be suggested as the best course of action.
Possible Complications When Diagnosed with Biliary Duct Hamartoma
In some cases, patients with many biliary duct hamartomas (abnormal growths) may develop more dangerous conditions like intrahepatic cholangiocarcinoma (cancer within the bile ducts in the liver) and hepatocellular carcinoma (liver cancer). This risk is particularly higher in those who smoke over a long period, have large biliary duct hamartomas (more than 2 cm), or have a condition known as bile stasis, where the bile does not flow properly.[17]
Regular, long-term check-ups are vital for these patients. These check-ups should include evaluating levels of a protein called CA 19-9, which can be slightly high if a patient has many biliary duct hamartomas. If doctors notice any changes in MRI/MRCP imaging or in tumor markers, they may need to perform a liver lesion biopsy. They may also potentially need to remove the lesions if they can operate and confirm a diagnosis.[11]
Key Points:
- Certain patients with many biliary duct hamartomas may develop cancers like intrahepatic cholangiocarcinoma or hepatocellular carcinoma.
- Factors like long-term smoking, large biliary duct hamartomas, and bile stasis can increase this risk.
- It’s crucial for these patients to have regular check-ups.
- These check-ups may include testing levels of a protein called CA 19-9.
- Any changes in MRI/MRCP imaging or tumor markers require further testing, such as a liver biopsy.
- Surgeons may need to remove any confirmed lesions.
Preventing Biliary Duct Hamartoma
It’s important that patients, doctors, and other health care workers are made aware of the following details:
Firstly, they should fully understand the various possible causes for multiple biliary duct hamartomas. In simpler terms, this is the different conditions that could lead to the development of benign, or non-cancerous, growths in the bile ducts.
Secondly, they need to be aware of what these growths specifically look like on different types of medical imaging scans. These include ultrasounds, computed tomography (CT scans, commonly known as CAT scans), and magnetic resonance imaging (MRI scans).
Lastly, it’s extremely important for patients with this condition to have long-term monitoring by healthcare professionals. On rare occasions, these benign growths can turn malignant or cancerous. Regular check-ups can help catch that change early, which will ultimately help prevent negative health outcomes.