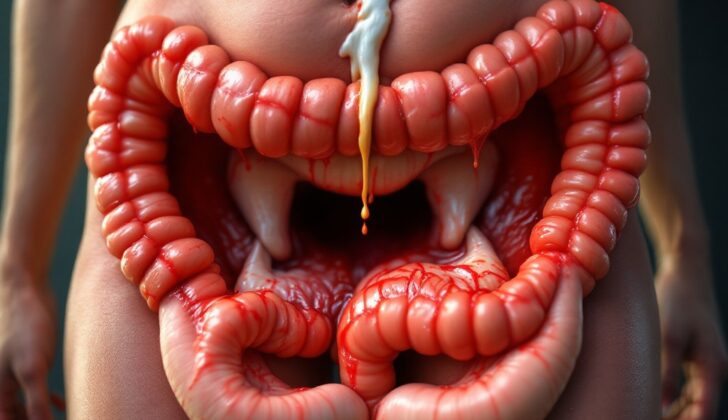
What is Fistula-in-Ano (Anal Fistula)?
An anal fistula is a tunnel connecting the anal canal to the skin around the anus. Most commonly, they’re caused by an abscess, which is a collection of pus, in the rectal area. The type of anal fistula is identified based on its location in relation to the muscles that control the anus (anal sphincters). While the condition isn’t life-threatening, it can cause significant discomfort and embarrassment. The goal of treatment is to control the infection and help maintain normal bowel movements. There are numerous treatment options available, and new ones are continuously being developed and tested. This article discusses the basic principles of diagnosing and treating an anal fistula.
What Causes Fistula-in-Ano (Anal Fistula)?
A fistula, which is an abnormal connection between two body parts, sometimes forms after an abscess, a pocket of pus, occurs in the anus or rectum. This can unfold when a small anal gland gets blocked and gets infected, leading to an abscess. The infection occurs near a group of muscle ring (sphincters) in the lower rectum and anus that control bowel movements, and so, the fistula could pass through these muscles.
Approximately a third of people who undergo a medical procedure to drain an abscess in their anus or rectum might later develop a fistula. Furthermore, between 30% to 70% of individuals who are diagnosed with such an abscess already show the presence of a fistula during their examination.
Risk Factors and Frequency for Fistula-in-Ano (Anal Fistula)
Fistula-in-ano, a common disease affecting the rectal area, is more prevalent in men than women. This condition often occurs between the ages of 20 and 40, with the average age of diagnosis being 38. Certain factors such as obesity, diabetes, smoking, high cholesterol, and a lack of physical activity can increase the risk of developing a fistula.
- Fistula-in-ano is frequently seen in the rectal area.
- The disease occurs more in men than in women, with 12.3 cases per 100,000 in men and 5.6 cases per 100,000 in women.
- The disease is most common in people aged 20 to 40, with an average diagnosis age of 38.
- Certain lifestyle and health factors can heighten the risk of developing a fistula. These include:
- Obesity
- Diabetes
- Smoking
- High cholesterol (hyperlipidemia)
- Lack of physical activity (sedentary lifestyle)
Signs and Symptoms of Fistula-in-Ano (Anal Fistula)
People with an anorectal abscess often feel intense pain in the area between the rectum and the genitals, which can be so severe that it hinders them from sitting or having a physical examination. Sometimes, pus might drain from the abscess. While signs like a fever are rare in people with healthy immune systems, deep abscesses could lead to lower back pain or a feeling of pressure.
A detailed medical history and physical check-up are essential for diagnosing the condition and planning the correct treatment. Past experiences with inflammatory bowel disease, rectal or anal tumors, previous anorectal diseases, or surgeries all play an important role in the diagnosis. It’s also important to assess and record baseline fecal continence, which means checking how well a patient can control their bowel movements. In cases where multiple fistulas are present or keep recurring, an inflammatory bowel disease might be the underlying cause.
Testing for Fistula-in-Ano (Anal Fistula)
If your doctor suspects you have a fistula-in-ano, a type of abnormal connection between your rectum and the outer skin surface near your anus, they will likely conduct a rectal exam to confirm the diagnosis and rule out any other conditions. As this exam can be uncomfortable, it’s often done under anesthesia in an operating room, which also allows the doctor to treat the condition right away, if it’s confirmed.
The doctor will then thoroughly examine your perianal skin (the skin around your anus) and any visible fistula openings. The doctor will use their finger to check for any lumps and evaluate the tightness of your anal muscle. They may also try to feel the fistula’s opening within the anal canal. If this is unsuccessful, the doctor can use an anoscope, a viewing instrument, to find and evaluate the internal opening. If they still can’t locate it, the doctor might inject your fistula with hydrogen peroxide, which increases their chances of finding the internal opening.
Once the fistula is located, your doctor will classify it based on its anatomical relation to your anal muscle complex. This classification is essential for choosing the best treatment while also preserving your bowel control. The classifications are as follows:
– Intersphincteric (make up about 45% of cases): the fistula penetrates the internal sphincter (internal anal muscle) but stays clear of the external one.
– Transphincteric (about 30% of cases): the fistula passes through both the internal and external sphincters (anal muscles).
– Suprasphincteric (around 20% of cases): the fistula goes through the internal sphincter and then ascends between the sphincters to reach above the external sphincter before travelling to the skin surface. This classification also includes horseshoe abscesses, another type of anal condition.
– Extrasphincteric (5% for this rare type): the fistula forms a connection from the rectum to the skin surface while extending outwards to the sphincters. Treating this type can be particularly challenging to ensure the sphincter muscles are preserved.
In addition to a physical examination, your doctor may also recommend imaging tests, such as magnetic resonance imaging (MRI), endoanal ultrasound, fistulography, or computed tomography (CT scans), particularly in complicated cases involving recurring disease or if Crohn’s disease is present. MRI is the most sensitive of these tests, yielding a more than 90% accuracy rate, with a combination of two imaging types yielding a 100% diagnostic accuracy rate.
Treatment Options for Fistula-in-Ano (Anal Fistula)
Treatment for an anal fistula, which is a small tunnel that forms between the end of your bowel and the skin around your anus, depends on where it’s located and what caused it. Most anal fistulas need surgery, though the type of surgery depends on a lot of different factors. However, complex fistulas, especially those caused by Crohn’s disease (an inflammatory bowel disease), are usually treated with medication.
Let’s talk about some common treatments:
Fistulotomy – This a surgical procedure where the fistula tract, the connecting tunnel, is opened and at times, a muscle called the sphincter is divided. This treatment works well for simple fistulas which have minimal involvement of the sphincter. About 90% of the patients who receive this treatment heal properly. A process called Marsupialization, which is basically stitching the cut edges to create a pouch, can help reduce bleeding and control pain after the operation.
Endorectal advancement flap – This procedure is more difficult than a fistulotomy and involves closing the internal opening of the tract, cleaning out the tract, and moving some of the lining of the rectum to cover the defect. During this procedure, the sphincter isn’t divided, but might be damaged while performing the flap, and there have been cases where up to 35% have experienced incontinence, which is the loss of control over bowel movements. The results of healing after this procedure have varied between studies but are generally between 66% to 87%. The treatment is less successful with patients who have Crohn’s disease, cancers in their past medical history, and those who have tried repairs before.
Seton Placement – This involves placing a thin piece of thread called a Seton through the fistula to help it drain over time. This procedure is usually used for complex fistulas and is a two-part process. The first part is placing the Seton and the second usually involves a fistulotomy. The Seton can be a ‘draining’ one which is placed loosely to promote long-term drainage, or a ‘cutting’ one which is tied tightly and gradually tightened over time to divide the sphincter with less risk of incontinence. Drainage and Setons can be made from various materials. The two-stage Seton placement heals the fistula completely in 94% of patients.
LIFT – Short for ligation (tying off) of the intersphincteric (between the sphincters) fistula tract, this procedure has an average success rate of 71%. The surgeon finds the internal opening of the fistula, ties off the part of the fistula between the sphincters, removes the infected gland and cleans the wound. This procedure does not involve dividing the sphincter, so incidences of incontinence are rare.
Fibrin plug and glue – This treatment involves using a collagen matrix (a fibrous protein that provides structure) to block or plug the internal opening of the fistula tract. This treatment does not involve cutting or dividing the sphincter, so should not result in incontinence. However, it has less than a 50% success rate in treating anal fistulas. Likewise, fibrin glue used to promote healing in the fistula has low success rates ranging from 14% to 69%. More recent studies have combined surgical treatment of the fistula with fibrin plugs and glue, showing more promise.
Medical management – Antibiotics are typically unnecessary for uncomplicated and drained rectal abscess, a pocket of pus that forms near the anus. They are reserved for those with weakened immune systems, those showing signs of severe illness, and the presence of skin infection around the abscess. Medication should also be considered in patients with Crohn’s disease, with certain medications showing a promising 36% rate of fistula closure after 54 weeks of treatment. If this does not work, a staged fistulotomy might be needed.
What else can Fistula-in-Ano (Anal Fistula) be?
When experiencing certain symptoms, it’s important to be aware that a variety of different conditions might be causing those symptoms. Here are some possibilities:
- Acute proctitis (inflammation of the rectum)
- Anal carcinoma (cancer in the anus)
- Anorectal abscess (a collection of pus in the area of the anus and rectum)
- Constipation
- Diverticulitis (inflammation of small pouches in the digestive tract)
- Hidradenitis suppurativa (a chronic skin condition with small, painful lumps)
- Inflammatory bowel disease (disorders that cause inflammation in the digestive tract)
- Pilonidal cyst (a cyst or abscess near or on the natal cleft of the buttocks)
- Pilonidal sinus (a small hole or tunnel in the skin, usually at the top of the buttocks)
Always consult with a healthcare professional for accurate diagnosis and treatment options.
What to expect with Fistula-in-Ano (Anal Fistula)
A fistula-in-ano is not a condition that threatens life, but it might greatly affect a person’s day-to-day life. Treatment aims to eliminate the fistula – an abnormal connection between the anus and the skin, while preserving the core muscle controlling the release of stools.
However, the treatment can have significant side effects that can dramatically change a patient’s life. These include fecal incontinence (an inability to control bowel movements), recurrence of the fistula, and anal stenosis (a narrowing of the muscular opening of the anus).
The likelihood of the fistula returning ranges from 3% to 57%, depending on the specifics of the fistula’s location and the type of treatment used.
Possible Complications When Diagnosed with Fistula-in-Ano (Anal Fistula)
One of the main risks of surgery for treating an anal fistula is the potential damage to the external sphincter, which could lead to an inability to control bowel movements. Before surgery, it’s important to understand the patient’s current control over their bowel movements and to measure the tightness of the sphincter muscle before it is numbed for surgery. The specific type of fistula and the surgical plan greatly determine the risk of experiencing bowel control issues after surgery. To lower this risk, the surgical method is chosen based on the specific details of the patient’s condition.
Complex fistulas, particularly those that pass above the sphincter muscles or outside the sphincter muscles, carry a higher probability of causing bowel control problems since they involve the sphincter muscles.
People with particular characteristics like being overweight, smoking, or having previously had anal surgery have a higher chance of the anal fistula coming back. Recurrence also depends on the specific properties of the fistula; for example, presence of multiple fistula tracts, a high fistula crossing the sphincter muscle, not being able to find the internal opening of the fistula, placement of a drainage seton, or the presence of horseshoe-shaped abscesses are all associated with a higher chance of recurrence. Most often, if the fistula comes back, it does so within the first year of treatment.
Common Risks and Factors Associated with Anal Fistulas:
- Damages leading to inability to control bowel movements
- Complex fistulas pose higher chances of bowel control problems
- Being overweight or a history of smoking increases recurrence
- Previous anal surgery can lead to a higher chance of recurrence
- Multiple fistula tracts, high fistula, unidentified internal opening, placement of seton, or horseshoe abscesses, all potentially lead to higher recurrence rates.
- Recurrence often occurs within the first year of treatment