What is Hepatic Failure?
Acute liver failure (ALF) is a complex health problem that affects the liver. It results in high liver biochemistry values (which means there’s abnormal levels of certain chemicals in the liver), problems with blood clotting (coagulopathy), and mental confusion due to liver issues (hepatic encephalopathy), all this with no prior long-term liver disease. A commonly used system categorizes liver failure into three categories. This was proposed by O’Grady and his team and is based on the timeframe between when jaundice (a condition that causes yellowing of the skin and eyes) appears and when mental confusion begins. They labeled these categories as hyperacute liver failure (within 7 days), acute (from 1 to 4 weeks), and subacute (from 5 to 12 weeks).
What Causes Hepatic Failure?
The main cause of acute liver failure, a condition where the liver stops working quickly, differs between different parts of the world. In the U.S. and Western Europe, it’s most commonly caused by damage to the liver due to medicine. However, in developing countries, it’s usually due to viral hepatitis, an inflammation of the liver caused by a virus. Around 2,800 people every year suffer from acute liver failure in the U.S, largely due to the pain reliever acetaminophen.
Different types of hepatitis virus can also cause acute liver failure. Hepatitis A and E are common causes. More than 1.5 million people suffer from hepatitis A globally, but it’s rare for it to lead to acute liver failure (less than 1%). Due to improvements in hygiene and the use of vaccines, the number of people suffering from acute hepatitis A has decreased in developed countries. Hepatitis B is behind most severe virus-related cases of acute liver failure. Hepatitis C doesn’t usually cause acute liver failure, while Hepatitis D can cause it in people who also have Hepatitis B. Although Hepatitis E is a rare cause of acute liver failure in the U.S., it’s responsible for around 20 to 40% of cases in developing countries.
Herpes simplex virus (HSV) infection is an infrequent cause of acute liver failure, but if left untreated, it carries an 80% chance of death. HSV most commonly affects people with weak immune systems and pregnant women. Epstein-Barr virus, which causes mononucleosis, is a very rare cause (less than 1% of all cases). The cytomegalovirus is another virus that can lead to hepatitis; however, it’s uncommon, affecting 19 in 100,000 people. The Amanita phalloides mushroom often causes hepatotoxicity, a condition where the liver is damaged by chemical substances. Ischemic hepatitis is another common cause in patients in intensive care. It happens when there is a decrease in blood flow to the liver cells, causing harm to them.
Acute liver failure can also result from specific liver diseases related to pregnancy, such as acute fatty liver of pregnancy and a condition called HELLP syndrome. Budd-Chiari syndrome, cancer, and Wilson’s disease, a rare inherited disorder, can also lead to acute liver failure.
Risk Factors and Frequency for Hepatic Failure
Acute liver failure, although less common, has less than 10 cases per million people each year in developed countries. For instance, in the United States, around 2800 cases are reported yearly. This condition is more common in developing countries and tends to affect young people more often.
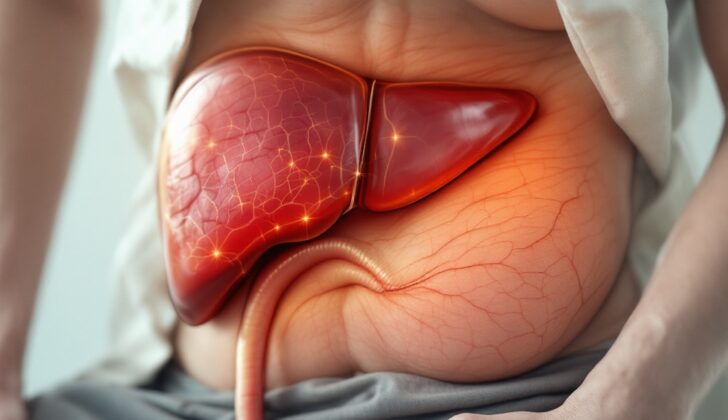
Signs and Symptoms of Hepatic Failure
Acute liver failure can show up differently in different people, depending on the cause and how long you’ve had this condition. Common signs and symptoms include:
- Yellowing of the skin and eyes (also known as jaundice)
- Pain in the upper right part of your abdomen
- Swelling in your abdomen
- Feeling sick (nausea)
- Throwing up (vomiting)
- Feeling generally unwell (malaise)
- Becoming severely thirsty and dry (dehydration)
Testing for Hepatic Failure
If you’re suspected of having acute liver failure, diagnosing starts with understanding your medical history and carrying out a physical examination. The doctor will then order laboratory tests and abdominal imaging.
Information such as previous jaundice episodes, your use of medication and alcohol, any family history of liver disease, and your risk factors for acute viral hepatitis are all essential.
Testing in a lab is necessary to pinpoint the cause and determine the severity of the condition. Lab tests may include liver blood tests, INR (a test that measures your blood clotting), checking your kidney function, a metabolic panel, blood count, and testing for viral hepatitis and HIV. They might also do a toxicology screen and measure your acetaminophen level, if relevant. If Wilson’s disease is suspected, your doctor may order a ceruloplasmin level test. If you have acute or chronic hepatitis, your doctor may request a test for anti-hepatitis D virus antibodies. If you’ve traveled to areas where Hepatitis E is common, they may also test for anti-hepatitis E virus antibodies.
An abdominal imaging evaluation, which usually involves an ultrasound, can help rule out any chronic liver disease or cirrhosis. This process ensures a detailed and thorough diagnosis.
Treatment Options for Hepatic Failure
Acute liver failure is a serious condition that can lead to various complications, with some individuals ultimately not surviving. People with this condition typically require intensive care and should urgently be transferred to a healthcare center that can perform liver transplants. It’s crucial to start treatment as promptly as possible, even while undergoing tests and scans to diagnose the condition.
The treatment typically depends on the cause of the acute liver failure. For instance, certain medications (such as N-acetylcysteine) may be given for poisoning from a common painkiller (acetaminophen), antiviral medications for a sudden outbreak of Hepatitis B, steroids for authorities-related liver issues, penicillamine for a rare genetic disorder called Wilson’s disease, or penicillin for certain types of mushroom poisoning. Interestingly, N-acetylcysteine also seems to help in cases of acute liver failure not caused by acetaminophen.
A key part of treating acute liver failure, regardless of the cause, is to prevent a condition called cerebral edema, which is swelling in the brain. This can be accomplished through methods like raising the head, using certain medications (like mannitol), helping with breathing, and taking steps to protect the brain. In severe cases, intracranial pressure monitors may be needed to keep track of the pressure inside the skull.
Complications such as metabolic acidosis (an excessively acidic body chemistry), coagulopathy (a condition that affects your blood’s ability to clot), low blood sugar levels, and kidney failure are also common. The ability of blood to clot is only treated if the patient is actively bleeding or needs an invasive procedure. Kidney replacement therapies may be initiated at an early stage for those experiencing kidney failure. Hypoglycemia, or low blood sugar, can be harmful and should be prevented with a dextrose infusion. The use of preventive antibiotics is a subject still under discussion.
The overall goal in managing acute liver failure is to take assertive supportive measures to avoid failure of several organs, until the patient either recovers or a liver transplant can be performed.
What else can Hepatic Failure be?
Here are some conditions that may be confused with each other due to the similarity of their symptoms:
- Acute fatty liver of pregnancy
- Amanita phalloides mushroom poisoning
- Acetaminophen poisoning
- Bacillus cereus toxin
- Fructose intolerance
- Galactosemia
- HELLP (HEmolytic anemia, Elevated Liver enzymes, Low Platelet count) syndrome of pregnancy
- Bleeding caused by viruses like Ebola, Lassa, and Marburg
- Unexplainable reactions to drugs
- Newborns with excessive iron storage diseases
- Tyrosinemia
What to expect with Hepatic Failure
Thanks to advancements in transplant techniques, survival rates have improved over time, as shown by an American study. According to a 2012 European report, the current survival rates after transplantation are 79% after 1 year and 72% after 5 years.
Several factors can impact these predictions when it comes to Acute Liver Failure (ALF). For example, encephalopathy, a condition that affects the brain’s function, is a crucial sign. Other important factors include the patient’s age and the severity of liver injury. Liver injury can be measured by the presence of coagulopathy, a condition that affects the blood’s ability to clot, or jaundice, which causes yellowing of the skin and eyes due to liver damage.
For predictions on how ALF will progress, medical professionals often use a system known as The King’s College Criteria.
Possible Complications When Diagnosed with Hepatic Failure
Cerebral edema, also known as swelling in the brain, can lead to a condition called Encephalopathy. This condition is usually categorized based on its severity, ranging from grade 1 to grade 4:
- Grade 1: Mood changes, abnormal behavior, difficulty focusing, problems with reasoning, irritability, and disrupted sleep.
- Grade 2: Temporary confusion, sluggishness, or a flapping tremor.
- Grade 3: Severe confusion, incoherent speech, strong drowsiness.
- Grade 4: Coma, unresponsive to verbal or painful stimuli.
When the pressure inside the skull rises above 20 mmHg, it often signals cerebral edema. This can worsen and lead to intracranial hypertension, found in 75% to 80% of patients with Acute Liver Failure (ALF) and grade 4 Encephalopathy. The earliest indications of this pressure increase are high systolic blood pressure and slow heart rate.
Coagulopathy, a condition affecting the blood’s ability to clot, often leads to bleeding from the upper part of the digestive tract. Hepatitis-associated aplastic anemia (HAA) is a rare but dangerous condition that impacts the blood and can occur alongside Hepatitis.
Infections are a frequent cause of death in ALF patients due to their reduced immunity. These are mostly bacterial (80%) with 20% to 30% being fungal infections. When there is a buildup of fluid in the abdomen (ascites), unexplained high body temperature and high white blood cell count warrant a diagnostic procedure called paracentesis. However, giving antibiotics as a preventative measure is not currently recommended.
Kidney failure, specifically Acute Renal Failure, is a common complication of ALF and a sign of poor prognosis. It’s often a result of alterations in blood flow and associated conditions like dehydration, low systemic vascular resistance, acute kidney tubular cell death, blood loss from the digestive system, and a liver-related kidney condition.
Due to the high metabolism of ALF, good nutrition is crucial. Early introduction of oral or IV nutrition is recommended. Balance of electrolytes like sodium, potassium, phosphate, magnesium, and correct pH (maintained by respiration), is frequently disrupted. Low sodium levels indicate a poor prognosis.
Finally, lung-related complications may occur, including fluid in the lungs, pneumonia, and inflammation in the airways.
Preventing Hepatic Failure
Get vaccinated for Hepatitis B and A as prevention is always better. Avoid taking medication on your own without a doctor’s advice. Don’t eat wild mushrooms – they may carry harmful toxins. When getting a tattoo or piercing, make sure that the equipment used is sterilized to avoid any infections.