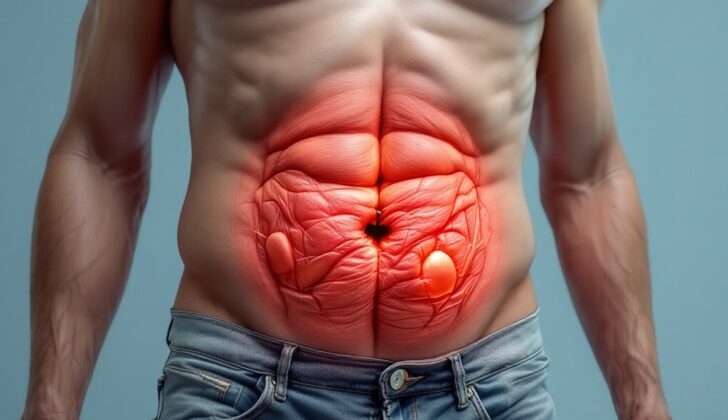
What is Rectus Sheath Hematoma?
A rectus sheath hematoma is a rare condition that usually happens after an injury to the abdominal wall or when a person is taking blood thinners. Although this condition has been well-studied, it can still be hard to diagnose because its symptoms can appear similar to many different types of abdominal problems.
What Causes Rectus Sheath Hematoma?
A rectus sheath hematoma is a condition that happens when there’s an injury to a specific artery or smaller branches within a muscle in the abdomen, called the rectus muscle. This muscle is supplied blood by two main arteries known as the superior and inferior epigastric arteries.
The superior epigastric artery comes from an artery located in the chest called the internal thoracic artery. It travels downwards within the covering of the rectus muscle, known as the rectus sheath, where it meets and connects with the inferior epigastric artery.
On the other hand, the inferior epigastric artery comes from an artery in the lower part of the body called the external iliac artery. It travels upwards along the back side of the rectus muscle, without any protective sheath until it reaches a point called the arcuate line.
The arcuate line is located about a third of the distance between your belly button and the pubic bone. This positioning is where the inferior epigastric artery gains some protection from a covering known as the posterior rectus sheath.
Risk Factors and Frequency for Rectus Sheath Hematoma
Rectus sheath hematoma is a condition causing severe abdominal pain, but it only contributes to about 1% to 2% of all abdominal pain cases. In a 2016 study, it was found that this condition is more common in women than in men, with a ratio of 1.7 to 1. The average age of patients in the study was 67 years. The chance of dying from rectus sheath hematoma is less than 2%, based on recent studies.
Several known risk factors increase the likelihood of developing a rectus sheath hematoma. The highest risk is for people who are on blood-thinning (anticoagulation) medication. The study revealed nearly 70% of patients were on some form of blood-thinning medication. With increased use of these medications in recent times, it would be logical to assume a surge in rectus sheath hematoma cases. However, current scientific literature does not support this claim. The study also found that about 60% of patients with this condition also had chronic kidney disease of stage III or more. Other risk factors include:
- Abdominal wall injections
- Treatment with steroids or immunosuppressants
- Chronic cough
- Femoral puncture (needle insertion into the thigh)
- Antiplatelet therapy (medication to prevent blood clots)
Signs and Symptoms of Rectus Sheath Hematoma
Rectus sheath hematoma is a condition that can lead to different symptoms. In a study of 126 patients, the most common symptoms observed were abdominal pain (84%) and a detectable lump in the abdominal wall (63%). This abdominal pain is often sudden, sharp, intense, constant, and worsens with physical activity. There are also two specific signs, the Carnett sign and the Fothergill sign, that help identify this condition. The Carnett sign is when pain intensifies with the flexion of the abdominal wall muscles, which suggests that the pain is coming from the abdominal wall and not inside the abdomen. The Fothergill sign is when a detectable lump in the abdomen does not cross the middle of the abdomen and remains detectable when the abdominal wall is flexed. This indicates a rectus sheath hematoma.
- Abdominal pain
- Abdominal wall lump
- Pain worsens with abdominal muscle flexion (Carnett sign)
- Lump in abdomen remains with abdominal wall flexion (Fothergill sign)
About 55% of patients also experience a decrease in their hemoglobin levels from their normal range. Other less common symptoms include a bruised abdomen (17%), rapid heart rate (13%), low blood pressure (7.9%), fainting (1.6%), and the patient developing a peritoneal condition (9.5%) when the hematoma grows and impacts the peritoneum below the arcuate line.
- Decrease in hemoglobin levels
- Bruised abdomen
- Rapid heart rate
- Low blood pressure
- Fainting
- Possible peritoneal condition
In most cases of hemorrhagic shock, patients usually don’t show any vital sign changes until they lose 15% to 30% of their blood volume. While this could occur in patients with rectus sheath hematoma, it only happens in about 1% to 13% of cases. Therefore, even if a patient doesn’t show vital sign changes like rapid heart rate, low blood pressure, or orthostatic hypotension, clinicians should still consider rectus sheath hematoma as a potential diagnosis.
Testing for Rectus Sheath Hematoma
When you’re being assessed for a condition known as rectus sheath hematoma, your doctor may request some specific laboratory tests. These can involve measuring your levels of hemoglobin/hematocrit (which are parts of your blood), as well as looking at how well your blood is clotting. A drop in hemoglobin levels can sometimes indicate a condition like a hematoma, but this isn’t always a completely reliable way to judge, as it doesn’t always happen. To better understand what’s happening over time, your doctor might request regular hemoglobin tests.
In addition to these tests, if you’re suspected to have a rectus sheath hematoma, you’ll also be asked to undergo a test that checks how well your blood is clotting. This is because a large number of people with this condition are taking blood-thinning medication. If you’re on a common drug like warfarin, the results of this blood test can help your doctor decide if they need to use a drug to reverse the effects. Now that more people are using different types of blood-thinning drugs, this blood test might not give as much information, but your doctor will still likely to include it as part of your treatment.
If they decide it’s necessary, your doctor might also order an ultrasound of your abdominal wall. Studies have shown that this can provide useful information about 80% of the time. That said, the quality of the information the ultrasound gives can depend on the skill of the person operating the machine, as well as your individual characteristics. A typical finding in an ultrasound might be a collection of fluid in your abdominal wall, which can appear differently depending on how old the hematoma is. Follow-up ultrasounds can monitor the size of the hematoma, but this is also dependent on the ultrasound operator.
Another imaging method, the CT scan, has been reported to be almost 100% accurate at diagnosing a rectus sheath hematoma. A CT scan might reveal a mass behind the rectus abdominis muscle, which is a major muscle in the abdomen. The appearance of this mass will depend on how old the hematoma is and whether you had a special dye injected into your veins for the scan. This contrast dye can reveal whether there’s active bleeding within the hematoma. However, it’s not always possible to use contrast dye because of how common kidney disease is among patients with a rectus sheath hematoma.
Despite the high accuracy of CT scans, there can be instances where an ultrasound may be more suitable, like if you’re pregnant or have kidney disease.
Treatment Options for Rectus Sheath Hematoma
Fortunately, most cases of rectus sheath hematoma, a condition where blood collects in the abdominal wall, can be successfully managed without surgery. Studies have shown that about 80% of patients can be treated with simple measures such as rest, ice, compression, and pain relief. For patients with coagulopathy, a condition that affects blood’s ability to clot, stopping or reversing the effects of blood thinners is usually enough to allow the bleeding to stop on its own.
In cases where the patient has severe anemia or is in a unstable condition due to low blood pressure, it may be necessary to transfuse blood. If, despite these measures, the patient continues to bleed, the most appropriate initial course of action usually is angioembolization. This is a procedure where the doctor uses a catheter to block the blood supply to the area that’s bleeding. This procedure has been reported to successfully stop ongoing bleeding in virtually 100% of cases.
Surgical intervention for rectus sheath hematoma is rare. In fact, surgery can pose a bigger risk of bleeding, especially in patients with coagulopathy. Therefore, it’s only considered when less invasive treatments have failed.
What else can Rectus Sheath Hematoma be?
A rectus sheath hematoma is a rather rare cause of abdominal pain, and its symptoms can vary greatly. This means a doctor also has to think about other possible causes for the pain. Depending on where the pain is, the doctor might consider several different conditions, including:
- Appendicitis
- Diverticulitis
- Biliary colic
- Urinary tract infection
- Tumors
- Hernia
These are all potential reasons a patient may be feeling pain, and need to be ruled out before a final diagnosis can be made.
What to expect with Rectus Sheath Hematoma
Most patients recover effectively without experiencing any complications since their body naturally absorbs the hematoma, or the local collection of blood, within 2 to 3 months.
For patients who require therapeutic anticoagulation, a treatment using medications to prevent blood clots, it’s important that they are made aware of the risk of the condition recurring if therapy resumes.