What is Shigellosis?
Shigellosis is a type of diarrhea caused by a bacteria named Shigella. This bacteria is usually found in countries where hygiene and sanitation aren’t quite good. It spreads from person to person or through eating or drinking contaminated food or water. Lately, there have been cases where Shigellosis was transmitted sexually, particularly among men who have sex with men. Anyone can catch this, but young children, old people, and those with a weak immune system are at a higher risk.
What’s alarming about Shigellosis is that the bacteria can tolerate stomach acid, which usually kills most other harmful organisms. This means that even a small amount of Shigella can cause the disease. Once they get past the stomach, they grow in the small intestine before moving to the colon or large intestine. Here, they release harmful substances that cause swelling and allow them to infest the lining of the colon. These substances also produce symptoms like watery or bloody diarrhea, discomfort, and fever.
If you’ve been infected by Shigella, you might start feeling sick, usually with bloody diarrhea that may have mucus, within 1 to 4 days. You might also experience stomach pain and vomiting. Shigellosis usually goes away on its own in about 5 to 7 days. However, in some cases, antibiotics may be needed to quicken recovery or prevent serious complications, like a severe form of kidney failure known as hemolytic-uremic syndrome or arthritis that happens after infection. However, doctors must choose antibiotics carefully as some Shigella are resistant to these medications. This is why it’s crucial to test the Shigella to identify what medication can effectively treat it.
What Causes Shigellosis?
Shigellosis, a type of food poisoning, is caused by a bacterium known as Shigella, a kind of bacteria that doesn’t move, doesn’t need oxygen to live, and doesn’t form spores in unfavorable conditions. There are four different types of Shigella bacteria, labeled as groups A to D, and each group has one or more subtypes with unique characteristics.
These four groups are:
* Group A – Shigella dysenteriae (has 12 subtypes)
* Group B – Shigella flexneri (has 6 subtypes)
* Group C – Shigella boydii (has 23 subtypes)
* Group D – Shigella sonnei (has only 1 subtype)
Among these, Shigella flexneri (group B) is the most common cause of diarrhea around the world and is particularly prevalent in lower to medium-income countries. Although Shigella boydii (group C) and Shigella dysenteriae (group A) are less common, they are usually found in sub-Saharan Africa and South Asia. Shigella dysenteriae type 1 is particularly deadly and can cause outbreaks in communities dealing with turmoil.
On the other hand, Shigella sonnei from group D is the most common cause of food poisoning in high-income countries and is often a cause of traveler’s diarrhea. Usually, Shigella sonnei only results in a mild disease with watery diarrhea, whereas Shigella flexneri and Shigella dysenteriae can result in dysentery, which is an infection of the intestines that results in severe diarrhea containing mucus and blood.
In the United States, Shigella is the most common cause of bacterial food poisoning with around 500,000 cases, 100,000 hospitalizations, and 500 deaths every year. The majority of these cases (77%) are caused by Shigella sonnei (Group D).
Risk Factors and Frequency for Shigellosis
Shigella, a bacteria that causes a disease called shigellosis, only affects humans. This bacteria is often spread in areas where hygiene is lacking or through contaminated food or water. It can also be passed on through direct contact between people or sexual contact. This is usually in places where there are crowds, people with poor hygiene, or where people cannot use the toilet properly, like in long-term care facilities or among young children.
- Each year, around 188 million cases of shigellosis are reported worldwide.
- About 164,000 of these cases result in death.
- Outbreaks of shigellosis often happen in conditions where cleanliness is poor, such as during wars or natural disasters.
- Increased temperatures may also raise the risk of diseases like shigellosis.
Shigellosis can affect anyone, regardless of gender or ethnicity. However, children between 6 months and 5 years old are the most affected group worldwide. In low and middle-income countries, a strain of Shigella called S flexneri is the most common cause of this disease in children under 5. The second most common cause is another strain called S sonnei.
Signs and Symptoms of Shigellosis
Shigellosis is a disease that typically starts 1 to 4 days after exposure. The severity and duration of the illness can vary depending on the type of bacteria involved and the patient’s overall health. The disease generally lasts 5 to 7 days in healthy individuals. However, it tends to be more severe and lasts longer in certain groups of people, such as young children, elderly individuals, travelers, people with HIV, and those living in crowded or unsanitary conditions. The bacteria S. sonnei usually cause a mild illness with watery diarrhea, while S. flexneri and S. dysenteriae type 1 can cause bloody diarrhea.
The kind of exposure, including sexual practices, people who have been ill, and recent travel, should be considered when diagnosing someone with the signs or symptoms of shigellosis. Most patients with this illness report abdominal pain and diarrhea. In fact, some patients describe the pain ranging from mild discomfort to severe, widespread, crampy pain. Other common symptoms include fever, loss of appetite, tiredness, general discomfort, and a constant need to pass stool.
- 1-4 days after exposure, symptoms will start
- Watery diarrhea (caused by S. sonnei)
- Bloody diarrhea (caused by S. flexneri and S. dysenteriae type 1)
- Abdominal pain
- Fever
- Loss of appetite
- Tiredness
- General discomfort
- Constant need to pass stool
Those with a severe case of the illness may experience more serious symptoms. During an examination, doctors will often check vital signs, as a fever, rapid heart rate, rapid breathing, and low blood pressure may suggest a severe case of the disease and possible dehydration. The abdominal examination can reveal bloating, widespread tenderness, and increased bowel sounds, especially in the left lower part of the abdomen. More severe cases can involve changes in mental status, hallucinations, seizures, stiffness of the neck, and coma. These more severe symptoms, along with signs of acute kidney injury, hemolytic uremic syndrome, toxic megacolon, or reactive arthritis, indicate a severe case of shigellosis.
Testing for Shigellosis
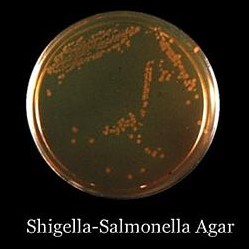
The presence of the Shigella bacteria, which causes shigellosis, is confirmed when it is found in the stool of a person showing signs or symptoms of the disease. When someone has symptoms like diarrhea, stomach cramps, or fever, doctors will usually ask for a stool sample for testing and analysis. Doctors prefer stool samples over rectal swabs because they provide more accurate results. If you have shigellosis, the test will typically show white blood cells and blood in about 70% of cases.
There are other types of tests, like stool alpha-1 antitrypsin assays, enzyme-linked immunosorbent assays (ELISAs), and polymerase chain reaction (PCR) testing, but they are not usually needed to diagnose shigellosis. That said, if the stool sample contains high levels of alpha-1 antitrypsin, a type of protein, it can suggest a person has shigellosis and the disease is not responding to medication. In rare cases, diagnostic tests like ELISA or PCR, which detect bacterial genetic material or toxins, might be used to confirm the diagnosis.
These diagnostic tests that do not involve culture can also help detect patterns of antibiotic resistance and prevent outbreaks by tracking where the bacteria is spreading.
In severe cases of shigellosis, blood cultures may be recommended. Normally, shigella bacteria does not travel in the bloodstream, but if it does, it can lead to higher risk of death. This usually happens in younger or older patients, or in those with weakened immune systems.
Blood tests are not always required to diagnose shigellosis. However, if a person appears to be very sick or dehydrated, or if there are complications, doctors may order laboratory tests. A complete blood count might show high numbers of white blood cells, and possibly low amounts of red blood cells and platelets. If there are broken red blood cells in the blood, it may suggest a condition called hemolytic uremic syndrome.
In the case of severe shigellosis, slight alterations in liver enzyme levels and electrolyte imbalances may be observed. Lower than normal sodium levels in the blood are usually due to a hormone imbalance caused by the syndrome of inappropriate antidiuretic hormone secretion. If there is a high level of waste products in the blood, it could suggest dehydration or hemolytic uremic syndrome. Additionally, signs of inflammation like an increased erythrocyte sedimentation rate and C-reactive protein are usually seen in severe cases of shigellosis but these markers alone aren’t specific enough to diagnose the disease.
Treatment Options for Shigellosis
Shigellosis, a bacterial infection that causes diarrhea, is primarily treated with supportive care, such as oral or intravenous rehydration to replace lost fluids and minerals. Severe cases might require hospitalization for intravenous-fluid rehydration. Certain medications that slow down the movement of the gut, like loperamide, paregoric, or diphenoxylate, are usually not recommended if you have a Shigella infection since they can worsen the condition and potentially cause toxic megacolon, an enlargement of the large intestines.
Antibiotics, which are medications that kill bacteria, are generally not used for mild Shigella infections. However, in certain situations, such as when the patient needs to be hospitalized, has an infection in their bloodstream (bacteremia), is dealing with a severe illness that weakens their immune system, or works with children or in institutions, antibiotics might be recommended. Antibiotics have been shown to decrease symptoms of Shigellosis and stop its spread to others. When choosing an antibiotic for Shigellosis treatment, physicians take into account local antibiotic resistance patterns and the patient’s individual risk profile, such as their recent travel history or previous use of antibiotics.
Antibiotic resistance, a situation in which bacteria can survive in the presence of an antibiotic, has been increasingly observed in Shigella, presenting a significant public health challenge. This resistance can be caused by certain biological mechanisms that occur within the Shigella bacteria or by the transfer of resistance-causing genes between bacteria. Recently, the emergence of extremely drug-resistant Shigella, with resistance to several types of antibiotics, has been reported, particularly in Great Britain and Europe. This has led to concerns about using some common antibiotics, like macrolides, penicillins, cephalosporins, and fluoroquinolones, to treat Shigellosis.
If a patient with Shigellosis does not require hospitalization and has a low risk of antimicrobial resistance, fluoroquinolones, azithromycin, and trimethoprim-sulfamethoxazole are often used as first choice antibiotics. For high-risk patients, such as those with HIV, those who live in Africa or Asia, or those who have a history of traveling to these places, third-generation cephalosporins are often recommended. More potent antibiotics, such as carbapenems, might be considered for patients who remain ill after receiving outpatient treatment or who require hospitalization.
In children, when it’s not possible to conduct an antibiotic susceptibility test (which determines the most effective antibiotic for a particular bacterial infection), azithromycin is often used to empirically treat Shigellosis. Other antibiotics like cefixime and ceftibuten are usually first-line treatments for Shigellosis in South Asia due to prevalent resistance to commonly used antibiotics in this region. Pivmecillinam can also be considered as it can effectively reduce the duration of diarrhea and eliminate Shigella bacteria from the stool.
Frequent handwashing with soap and water is essential to prevent the spread of Shigellosis, especially after using the restroom and before preparing food. People involved in food handling should refrain from engaging in food preparation if they continue to test positive for the presence of Shigella bacteria in their stool.
What else can Shigellosis be?
When trying to diagnose shigellosis, which results in symptoms such as fever, nausea, vomiting, and abdominal pain, doctors must consider other infections that could cause similar symptoms. These include:
- Non-typhoidal Salmonella
- Escherichia coli (E. coli)
- Campylobacter spp
- Clostridioides difficile
- Typhoid fever (Salmonella enterica serotype Typhi and, less frequently, Salmonella enterica serotypes and paratyphi A, B, and C)
- Entamoeba histolytica
- Aeromonas spp
There are also non-infectious causes of chronic diarrhea which should be considered when diagnosing shigellosis. These include:
- Inflammatory bowel disease
- VIPoma (a rare type of tumor)
- Hyperthyroidism
- Lactose intolerance
- Celiac disease
- Irritable bowel syndrome
In order to make an accurate diagnosis, the physician must carefully assess these potential sources of the patient’s symptoms.
What to expect with Shigellosis
Shigellosis, a type of infection, usually gets better on its own within 5 to 7 days. In more severe cases where patients need to seek medical help, it’s crucial that doctors consider shigellosis as a possible diagnosis and start treatment quickly. This is especially important if the patient has recently traveled. When detected and treated promptly, shigellosis has a good outcome and patients usually recover without any long-term health problems.
However, there are certain things that can make the disease more severe and increase the likelihood of complications. These include a delay in starting the right treatment, having a weakened immune system, having the illness for more than 7 days, being very young or very old, and having bacteremia, which is when bacteria enter the bloodstream. Bacteremia is particularly serious and is mostly seen in malnourished children, carrying a 20% risk of death.
Shigellosis can also lead to complications such as the hemolytic uremic syndrome, a condition characterized by a low platelet count (thrombocytopenia), destruction of red blood cells leading to anemia (hemolytic anemia), and sudden kidney failure (acute kidney injury). This syndrome is a type of anemia where red blood cells are destroyed and block the small vessels. This condition is serious, with a risk of death up to 50%.
Possible Complications When Diagnosed with Shigellosis
Shigella infection can lead to various complications. These are broken down into problems with the intestines (intestinal complications) and whole body (systemic complications).
Intestinal Complications:
- Colonic perforation: This is a rare event where a hole occurs in the large intestine, especially with S flexneri and S dysenteriae type 1 infections. It mainly happens in infants and malnourished patients.
- Intestinal obstruction: This often occurs in severe disease and S dysenteriae type 1 infection, and it involves a blockage in the digestive tract.
- Toxic megacolon: This condition, in which the colon expands dangerously, usually occurs in S dysenteriae type 1 infection.
- Proctitis or rectal prolapse: This is caused by the invasion of the bacteria into the lining of the large intestine. It most frequently affects infants and young children.
Systemic Complications:
- Bacteremia: This is when bacteria enter the bloodstream, and it often occurs in children younger than five years.
- Hemolytic uremic syndrome: Though uncommon, it’s one of the most common causes of sudden kidney damage in young children and infants.
- Moderate to severe hypovolemia: This is when there’s too little blood circulating in your body.
- Hyponatremia: This is when there’s too little sodium in the blood, and it often occurs with S dysenteriae type 1 infection.
- Leukemoid reaction: This condition involves an extreme increase in white blood cells and is common in children between two and ten years of age.
There are also neurological symptoms, such as generalized seizures, which are the most common neurological complication and are linked to a higher death rate. Reactive arthritis, a type of joint inflammation, can occur alone or together with eye inflammation (conjunctivitis) and urethra inflammation (urethritis), typically caused by S flexneri infection.
Other complications include vulvovaginitis in young girls, which can come with or without diarrhea and is marked by painless vaginal discharge. Keratitis, an inflammation of the cornea, is rare but should be considered in a young child with keratitis symptoms and a recent history of diarrhea. And finally, acute myocarditis, a condition marked by heart inflammation, commonly happens in children infected with S sonnei.
Preventing Shigellosis
If you have shigellosis, it’s crucial to understand how to stop the disease from spreading to other people. Shigellosis is a contagious illness, but it can be prevented from spreading by practicing cleanliness and hygiene. This includes using toilets safely, washing your hands properly, and using clean water to drink and prepare food. It can also be prevented by practicing good food hygiene and having suitable toilets and sanitation.
Doctors recommend that if you’re sick with shigellosis, you should avoid certain activities until you’re well again:
– If you’re still ill, don’t go to school or work, especially if your job involves taking care of children or handling food. Check with public health guidelines to know when it’s safe for you to return.
– It’s also important that you avoid any sexual activity while you’re still having diarrhea, and also for two weeks after it stops to prevent further spreading the disease to other people.
– Handwashing is essential, and you should do it often. Always wash your hands for at least 20 seconds with soap and water, particularly after going to the toilet or cleaning up after another sick person.
– During the time you’re unwell and even when recovering, don’t prepare food for others and avoid using public waters like swimming pools, beaches, lakes, and rivers to prevent spreading the bacteria in these waters.












