What is Spigelian Hernia?
A spigelian hernia is a not-so-common type of hernia where parts of the abdomen, or the lining of the abdominal cavity, poke through a weak spot in the abdominal wall. This weak spot is specifically located in the Spigelian fascia, a part of the abdomen made up of the transversus abdominis and the internal oblique muscles.
What Causes Spigelian Hernia?
A Spigelian hernia often develops due to certain underlying health issues that cause a rise in the pressures inside the abdomen, an injury to the abdominal wall, or a weakening of the layers of the abdominal wall which generally happens with aging or diseases affecting the creation of collagen, a type of protein that gives structure to your body. In some cases, a Spigelian hernia can occur without any apparent cause and has once been termed a “spontaneous lateral ventral hernia.”
Risk Factors and Frequency for Spigelian Hernia
Spigelian hernias are very uncommon types of abdominal wall hernias, making up between 0.12% to 2% of all such hernias. This condition is mainly seen in women and those above 60 years of age. Certain health conditions can increase the risk of developing a Spigelian hernia. These hernias are often associated with chronic obstructive pulmonary disease (COPD), because the chronic cough it produces increases pressure in the abdomen. Similarly, those with liver cirrhosis who develop ascites (fluid accumulation in the abdomen) or people who are pregnant or obese can also be at a greater risk. Patients suffering from collagen disorders, such as Ehlers Danlos syndrome, or the elderly are also at a higher risk. Spigelian hernias are rare in children, but when they do occur, they may be connected with other health issues, like undescended testes.
- Spigelian hernias are extremely rare, making up 0.12% to 2% of all abdominal wall hernias.
- They are mostly seen in women and individuals over 60 years old.
- People with certain conditions leading to increased abdominal pressure or weakened abdominal layers are at higher risk. These conditions include COPD, liver cirrhosis with ascites, pregnancy, obesity, or collagen disorders such as Ehlers Danlos syndrome.
- These hernias are very rare in children, but can sometimes be linked to issues like undescended testes when they occur.
Signs and Symptoms of Spigelian Hernia
Spigelian hernias are often detected when they cause a bulge in the abdominal wall, which can be either painful or painless. This bulge is more noticeable when standing and can occur suddenly or over time. The level of pain can differ for each person, depending on what is trapped in the hernia. Generally, these hernias come to medical attention due to complications, so doctors should try to establish when the patient first became aware of the hernia and how the symptoms have changed, especially if there is a concern about incarceration or strangulation. Other important information to gather includes whether the patient has had any long-term increase in abdominal pressure due to a chronic cough because of Chronic Obstructive Pulmonary Disease (COPD), fluid in the abdomen (ascites), obesity, or pregnancy.
Spigelian hernias can be tricky to detect because they can be hidden deep under the muscles of the abdominal wall. The chances of detecting them during a physical examination can be improved by examining the patient while they are standing and trying to bear down. However, even then, a palpable mass may not always be present, making it impossible to diagnose around half of Spigelian hernias using only a physical examination. This is especially true for patients who are overweight.
Often, these hernias go unnoticed until they start causing pain or the patient begins showing more worrying symptoms associated with incarceration, strangulation, or bowel obstruction. These symptoms may include pain at the site of the hernia, which may or may not be accompanied by noticeable features on examination. Because Spigelian hernias have rigid boundaries, they have a higher risk of causing incarceration compared to other types of abdominal hernias. Studies have shown that around 27% of diagnosed Spigelian hernias end up causing incarceration.
Immediate surgical repair is required if the patient shows signs and symptoms of strangulation or inflammation of the abdominal lining (peritonitis). These signs include a hernia that can’t be pushed back in, red and tender skin over the hernia, and protective muscle spasms. If the patient also shows signs of a systemic inflammatory response syndrome, this could also indicate the need for urgent surgery.
Testing for Spigelian Hernia
If you have a noticeable bulge along the curved line at the Spigelian fascia (a particular area in your abdomen), it’s usually fairly easy for your doctor to diagnose the problem. However, If the doctor is still not sure after examining you and taking your medical history, they might suggest taking a more detailed look with a radiological evaluation. This is usually an ultrasound, which has been shown to be a helpful first approach to diagnosing this issue. During this test, you might be asked to stand, as this can increase the pressure within the abdomen and make any problems easier to see. You might also be asked to perform a Valsalva maneuver, which is essentially taking a deep breath and trying to exhale while keeping your mouth and nose closed, as this can also help make issues more visible.
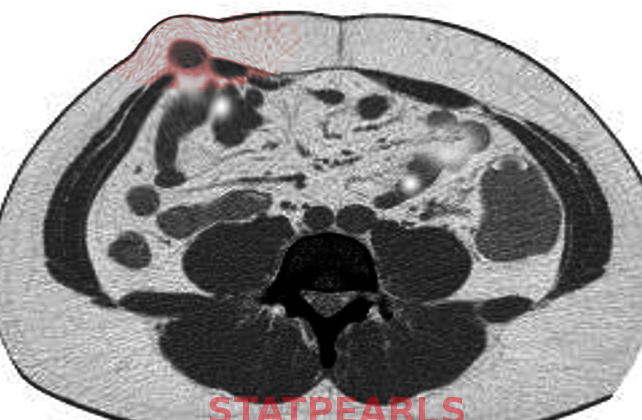
If the ultrasound doesn’t provide a clear enough picture, your doctor might order a computed tomography (CT) scan. CT scans are the best method to diagnose a Spigelian hernia, which is a type of hernia that happens along the semilunar line at the Spigelian fascia. This test should be performed with oral contrast, which means you’ll drink a special liquid before the test that helps to highlight the bowel and any hernia during the scan.
Treatment Options for Spigelian Hernia
While Spigelian hernias may not respond to conservative treatments or regular monitoring, they can still be managed through several surgical methods. Given the high risk of intestines getting trapped and cutting off their blood supply, surgery is often advised and has become the standard treatment. The surgery may be executed through an open, laparoscopic, or robotic approach.
Open surgery is a common technique to repair Spigelian hernias. Here, the operation may involve either closing the muscle tear or applying a mesh to support the area. Typically, a horizontal or a left side cut near the midline is made. In some cases, the classical approach is via a cut made at a right angle to an imaginary line joining the hip bone’s top front part to the belly button, centering on a significant point called McBurney’s. As the surgery progresses, the hernia sac (a protruding sac-like organ) is located and separated. As per the contents of the sac and the presence of a strangulated bowel (blocked intestines), the hernia may be either pushed back into place with a surgical tool, or parts of abdominal fat or bowel may need removal. Some surgeons may elect to use non-dissolvable sutures when closing the muscle tear, while others may use synthetic mesh or a biological mesh for support.
Laparoscopic surgery, another method, is associated with less discomfort and a shorter stay in the hospital when compared to open techniques. Several procedure methods have been used to repair Spigelian hernias, all involving the use of synthetic mesh. Other approaches include preparing and placing peritoneal flaps (folded layers of tissue lining the abdomen), wherein a mesh will be placed.
Robotic surgical techniques are relatively new, and are performed similarly to some laparoscopic approaches. However, there are not enough studies yet to compare the effectiveness and safety of robotic versus laparoscopic repairs.
If there’s a risk of infection inside the abdomen or if the contents of the hernia have their blood supply cut off, requiring a part of the bowel to be removed, a synthetic mesh should not be utilised to repair the hernia. Although no consensus exists on how to repair a Spigelian hernia in the case of contamination, options such as laparoscopic suturing, applying biological mesh, placing synthetic mesh in the space before the peritoneal lining, or multi-staged mesh repair are considered viable by the medical community.
What else can Spigelian Hernia be?
When a doctor is trying to diagnose a Spigelian hernia, they also need to consider other serious conditions that could cause similar symptoms. These conditions might include:
- Rectus sheath hematoma (bleeding into the muscles of the abdomen)
- Incisional hernia (a hernia caused by an incision from surgery)
- Ventral hernia (a hernia on the front of the abdominal wall)
- Soft tissue or abdominal wall cancer
- Abscess (a pocket of infection)
- Lymphadenopathy (enlarged lymph nodes)
What to expect with Spigelian Hernia
Overall, people with simple Spigelian hernias (a type of hernia that occurs along the outer edge of the rectus abdominis muscle) can expect a great outcome after surgical repair. However, if there are signs of bowel ischemia (a condition where blood flow is reduced or blocked to the intestines) or systemic inflammatory response syndrome (a severe body-wide response to infection or significant injury) due to the hernia being strangled, the risk of complications and even death increases.
Possible Complications When Diagnosed with Spigelian Hernia
Before surgery, patients may face risks such as:
- Confinement or Incarceration
- Strangulation
- Bowel obstruction
After surgery, possible complications include:
- Infection in the mesh used during the procedure
- Injury to the bowel or the organs in the abdomen
- Formation of a pocket of serous fluid (Seroma)
- Formation of a large bruise or blood-filled swelling (Hematoma)
- Infection at the surgical site
- Recurrence of the hernia