What is Villous Adenoma?
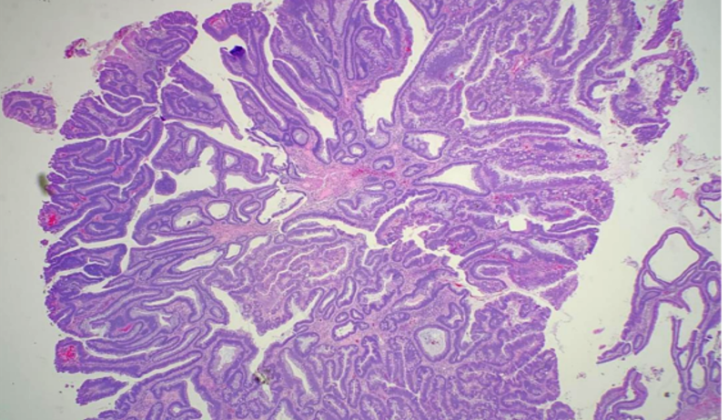
Adenoma is a term generally used to describe any non-cancerous tumor that arises from glandular tissue. This article specifically talks about adenomas in the colon, which commonly appear in growths called polyps. As people get older, the chances of developing colon polyps become higher. Adenomatous polyps are the most commonly found type of polyp in the colon, making up around 60 to 70% of all polyps in the colon. These adenomas can be categorized into three types: tubular, villous, or tubulovillous. Villous adenomas, identified by their resemblance to finger-like or leaf-like projections (see Image. Villous Adenoma), are classified as such if they have more than 75% villous features. Tubulovillous adenomas consist of between 25 and 75% villous features. If an adenoma has less than 25% villous features, it indicates a tubular adenoma. Adenomas are typically symptom-free and are usually discovered during routine screenings for colorectal cancer. However, it’s important to note that adenomas with villous features may slightly increase the risk of developing more advanced growths or abnormal cells (dysplasia) compared to other types of adenomas. Villous adenomas are more likely to appear in the rectosigmoid area, which is the part of the colon closest to the rectum, but they can show up in other parts of the colon as well.
What Causes Villous Adenoma?
Both your environment and your genes can affect your chances of getting colorectal polyps. Most of the time, these polyps appear randomly, even though a person’s genetics can have a serious influence on whether the polyps form in the first place. If you’ve had adenomas, a specific type of colon polyp, in the past, you’re at a higher risk for colon cancer.
This cancer typically forms from adenomatous colon polyps. Most of the time, these polyps occur randomly because of changes in the adenomatous coli pathway or DNA repair mechanism.
Familial adenomatous polyposis (FAP) is a genetic condition that greatly increases the chances of patients getting multiple adenomatous polyps. A mutation (or change) causes FAP in a gene that normally suppresses tumors, which means it usually helps control cell growth. This mutation can be inherited, or in about a third of patients, it can occur as a new mutation. FAP is quite rare, affecting between 1 in 8,000 and 1 in 14,000 people, but it leads to large numbers of polyps starting in late childhood. Even though these seem like big numbers, FAP represents only about 1% of colon cancers.
Adenomas are polyps with features of low-grade dysplasia, which means they have abnormal cells that aren’t quite cancerous yet. Some of these adenomas may slowly transform into more serious conditions, like invasive adenocarcinoma, a type of cancer. Even though doctors don’t completely agree, some studies show that adenomas with villous features might increase the risk of developing colorectal cancer. The size of adenomas at baseline can also influence future disease.
Risk factors for villous adenoma, a specific type of polyp, include:
– Your lifestyle and diet. Eating lots of fruits and vegetables can lower your risk, while consuming fats and alcohol can increase your risk.
– There’s a strong link between smoking and developing adenomas.
– Patients with acromegaly, a rare condition where the body makes too much growth hormone, are at high risk for adenomas and colon cancer.
– Some studies show a link between a bacteria called Streptococcus bovis and the formation of rectal villous adenomas.
– If you’ve had surgery to change the way your urine flows, you’re at higher risk for developing adenomas.
– Patients with Inflammatory bowel disease, a condition that causes long-lasting inflammation and sores in the gastrointestinal tract, are at high risk for adenomas and colorectal cancer.
Risk Factors and Frequency for Villous Adenoma
Colon polyps become more common as people get older. By the time people reach 50, around 25% to 30% have colon polyps, according to screenings for colorectal cancer. This number increases to 50% by the age of 70, especially in high-risk Western countries, such as the United States. However, colon polyps are rare in younger people, with only 1% to 4% of those aged between 20 to 30 having them. Also, not all colon polyps are the same. For example, villous adenomas, one type of colon polyp, make up between 5% to 15% of all adenomas.
Signs and Symptoms of Villous Adenoma
Most people with colorectal polyps don’t experience symptoms. Often, these polyps are discovered during routine health screenings or surveillance colonoscopy. Some people, though, might notice symptoms like rectal bleeding.
Polyps larger than 1 cm are more likely to cause symptoms. These symptoms may include:
- Abdominal cramps
- Changes in bowel habits
- Rectal bleeding
In rare cases, a type of polyp known as a villous adenoma can lead to severe diarrhea, which can cause dehydration and an imbalance of electrolytes in the body.
Testing for Villous Adenoma
The US Preventive Services Task Force recommends that adults at average risk start regular colon cancer screening from the age of 50. There are several ways to check for colon cancer. These include a fecal occult blood test, which checks your stool for tiny amounts of blood; a fecal immunochemical test, which also checks for blood in the stool; and direct visualization methods, which involves a detailed look at the colon.
In some cases, a colonoscopy or biopsy may be necessary. These procedures involve a detailed examination and testing of any unusual spots or growths in the colon to confirm the presence of polyps or cancer. On occasion, blood work may be required. Low hemoglobin and mean cell volume, along with low iron and ferritin levels in your blood, could indicate anemia caused by iron deficiency.
It’s noteworthy to mention that the fecal occult blood test doesn’t always confirm the presence of villous adenoma, a type of colon polyp. Only 40% of patients with this condition will test positive. Of these, roughly 2-10% may have colon cancer.
There are also imaging techniques like a double-contrast barium enema, which shows the colon more clearly than a single contrast barium study. However, the barium enema method can miss small polyps that are less than 6 mm, and improper bowel preparation can lead to false results. Also, if you have a condition like diverticular disease, it could lead to false negatives.
A fairly new method of screening is CT colonography, which uses a CT scanner to produce detailed images of your colon. But this technique also requires a thorough bowel preparation and may miss tiny polyps.
The most accurate method to check for polyps is endoscopy which does not only identify polyps but also helps in treatment. However, the process heavily depends on the operator, and it’s not entirely without risks and discomforts. One form of endoscopy, sigmoidoscopy, only allows the doctor to view up to 60 cm of the bowel and usually doesn’t require a full bowel preparation.
Treatment Options for Villous Adenoma
Surgeons should completely remove adenomatous polyps, which are growths that can develop in the lining of the bowel, ensuring there is no remaining affected tissue. Depending on how the polyp looks and how many are removed, follow-up screenings are recommended in line with American Cancer Society guidelines. Here’s a breakdown of what that means:
– If you’re of average risk (meaning you don’t have a close family member with colon cancer), you should have a colonoscopy starting at age 50. If there are no concerning growths or signs of cancer, you should have another one in 10 years.
– If the doctors find one or two small growths (less than 1 cm in size) with low-grade changes in the cells, they’ll likely recommend another colonoscopy in 5 to 10 years.
– If there are three to ten growths removed, or a big growth (at least 1 cm) or any growths with severe changes to the cells or villous features (which means they’re more likely to be cancerous), you should have another colonoscopy in three years.
– If more than ten growths were removed at once, you should have another colonoscopy within three years.
If you’re at increased risk (meaning a close relative developed colon cancer before turning 60, or if two or more of your close relatives had colon cancer at any age), you should start having colonoscopies at age 40 or ten years before the youngest person in your close family was diagnosed – whichever is earlier. You then follow the same guidelines as above, but you should never go more than five years between screenings.
If you’re at high risk due to genetic disorders that dramatically increase your risk of colon cancer (such as Familial Adenomatous Polyposis or FAP), doctors recommend yearly sigmoidoscopy, which is a less invasive screening test. If you’re known to have FAP, a surgery to remove the colon might be recommended.
If the growth is more than 2-3 cm, is flat against the wall of the bowel, and the edges are not clear after the removal procedure, then surgery might be necessary.
What else can Villous Adenoma be?
These are some conditions that can affect the mucosal lining of your body:
- Juvenile polyps
- Cowden disease
- Mucosal prolapse
- Pseudopolyposis
- Lymphoid polyps
What to expect with Villous Adenoma
Most villous adenomas, a type of abnormal growth in the colon or rectum, do not show any symptoms. However, they can lead to blockages, bleeding, or intussusception, a condition where one part of the intestine slides into an adjacent part. The main worry with villous adenomas is that they could turn into a type of cancer or a malignancy. Specifically, growths larger than 1 cm carry a high risk of becoming malignant.