What is Adenopathy?
Lymphadenopathy, or swollen lymph nodes, is something many doctors come across during regular medical appointments. Both doctors and patients can become anxious when they discover swollen lymph nodes because, in rare cases, this might be a sign of serious conditions like cancer or infections such as HIV or tuberculosis. However, it’s worth noting that most of the time, lymphadenopathy is harmless and resolves on its own. It’s crucial to understand how lymph nodes function and when their enlargement needs closer examination.
Lymph nodes are part of the body’s defense system. They contain different types of cells that can identify and react to harmful substances, hence increasing in size. The benchmark for a lymph node being considered “enlarged” is usually when it’s larger than 1 cm. However, this is not a strict rule as it can vary based on the patient’s age and the location of the lymph node. For example, children under ten years typically have bigger lymph nodes, and something as large as 2 cm could be normal, depending on the circumstance.
The characteristics of lymphadenopathy such as the pattern of the swelling, whether the nodes are tender or not, and the patient’s relevant symptoms and personal history provide vital information in diagnosing the condition. It might show up in a scattered way (generalized lymphadenopathy) or in a single group of lymph nodes (localized lymphadenopathy). The nature and location of the swelling can give a clue about what might be causing it. A thorough medical history including factors like exposure to diseases, medications, lifestyle habits, and demographic factors could also provide valuable hints.
An assessment of lymphadenopathy often starts with an in-depth patient history and a focused physical exam. The degree of assessment required largely depends on the patient’s symptoms. For instance, a person with neck lymphadenopathy and symptoms of a sore throat and fatigue might not require more than a basic history, examination, and a mono test. In contrast, someone with generalized lymphadenopathy might need a more comprehensive investigation.
Doctors categorize lymphadenopathy into three categories after a history and physical exam. It could be diagnostic, suggestive, or unexplained. In cases where the enlargement is unexplained, the patient’s risk for serious disease or cancer guides the next steps. For patients with a lower risk, the doctor might opt to watch the condition for a few weeks to see if the lymph node’s size reduces. If not, a biopsy might be necessary. For patients with a high risk, a biopsy is usually done immediately. More information like travel history, animal exposure, dietary habits, and history of smoking or drug use, among other factors, are considered.
While there are no set rules for laboratory evaluations of unexplained generalized lymphadenopathy, doctors typically start with complete blood count and checks for Epstein-Barr virus. If these tests don’t show anything, other tests like chest x-rays, tests for syphilis and HIV, among others, may be performed. If all these are negative, a sample of the lymph node might be taken for further examination.
Statistics on lymphadenopathy are not always accurate because most cases are caused by temporary illnesses that are not reported. That said, less than 1% of people with lymphadenopathy have cancer, and that number could go up to 50% or more for individuals with existing risk factors. So, it’s crucial to check any unexplained lymph node swelling properly to rule out any serious illness.

swollen, ruptured inguinal lymph node or buboe. After the incubation period of
2 to 6 days, symptoms of the plague appear, including severe malaise, headache,
shaking chills, fever, pain, and swelling, or adenopathy, in the affected
regional lymph nodes, also known as buboes.
What Causes Adenopathy?
Lymphadenopathy, or swelling of the lymph nodes, can be caused by various factors including:
* diseases caused by infections
* tumors
* disease related to inflammation
* autoimmune diseases
* inherited disorders related to metabolism
* exposure to toxins or certain types of medication
Infectious diseases that lead to swollen lymph nodes can be caused by different microorganisms:
* Viruses such as HIV, mononucleosis, roseola, herpes, chickenpox and adenovirus.
* Bacteria including Staphylococcus, Streptococcus, Salmonella, Syphilis, and Yersinia.
* Mycobacteria such as those causing tuberculosis and Mycobacterium avium intracellulare (MAI).
* Fungi leading to conditions like coccidioidomycosis, histoplasmosis, and Candida.
* Parasites behind toxoplasmosis, Chagas disease, and others.
Tumors can also cause swollen lymph nodes, which can be primary cancers or cancers that have spread from other parts of the body. These include acute lymphoblastic leukemia, Hodgkin lymphoma, non-Hodgkin lymphoma, neuroblastoma, leukemia in children, rhabdomyosarcoma, lung cancer that has spread, cancers that have spread from the digestive organs, metastatic breast cancer, thyroid cancer, and kidney cancer.
Other diseases, including autoimmune ones like sarcoidosis, juvenile rheumatoid arthritis, serum sickness, and systemic lupus erythematosus can also cause the condition.
Certain medications and toxins including allopurinol, atenolol, captopril, carbamazepine, many of the cephalosporins, gold, hydralazine, penicillin, phenytoin, primidone, paramethylamine, quinidine, the sulfonamides, and sulindac, can result in swollen lymph nodes. Certain lifestyle exposuress, like alcohol, UV radiation, and tobacco, can cause cancers that in turn result in lymphadenopathy.
Finally, certain inherited metabolic disorders like Niemann-Pick disease and Gaucher disease can also cause swelling of the lymph nodes.
Risk Factors and Frequency for Adenopathy
Lymphadenopathy, a condition where the lymph nodes become enlarged, affects both men and women relatively equally. It’s more common among children because they often have more viral infections. The condition is usually not serious in children, again due to the high prevalence of viral and bacterial infections in this age group. Approximately 75% of all lymphadenopathy cases are localized, with half of those cases mainly occurring in the head and neck area. They can also occur in the groin area, and in the armpit, above the collarbone.
Where the patient lives and their circumstances can indicate causes of lymphadenopathy. For instance, people living in developing regions like sub-Saharan Africa, Southeast Asia and the Indian subcontinent may experience it due to exposure to parasites, HIV, and tuberculosis. In contrast, in the United States and Europe, the Epstein-Barr virus, Streptococcus (the bacteria that cause strep throat), and some cancerous processes are common causes. Also, a patient’s exposure history can play a significant role in causing lymphadenopathy.
- Whether they had exposure to blood and products from blood through things like blood transfusion, unsafe sexual practices, intravenous drug use, or through their job.
- If they were exposed to an infectious disease, either at home, at work, or when traveling.
- Their use of medications, either prescription, non-prescription, or supplements.
- Exposure to diseases carried by animals, either from pets or at their job.
- Exposure to bites from arthropods, or insects.
Signs and Symptoms of Adenopathy
When diagnosing adenopathy, which is an abnormal enlargement of the lymph nodes, doctors rely heavily on a patient’s history and physical examinations. The complexity of these exams depends on the cause of the adenopathy. For example, diagnosing swollen cervical lymph nodes due to a strep throat infection is typically easier than diagnosing swollen lymph nodes as a result of more complex conditions like Gaucher disease or sarcoidosis.
The evaluation includes five key factors: how long the condition has been present, where the swellings are in the body, accompanying symptoms, the patient’s background and lifestyle, and any exposure to medications.
- Chronicity: Doctors consider swollen lymph nodes as “chronic” when they’re present for more than three weeks. Swollen lymph nodes that last less than two weeks or more than a year are usually linked to non-serious causes.
- Localization: Lymph nodes can be localized or generalized, meaning present in more than two unlinked areas. Generalized lymph nodes often require extensive tests and are usually a sign of systemic illness. Swollen localized lymph nodes usually indicate localized disease or infection.
- Concomitant symptoms: Additional symptoms provide crucial clues in diagnosing adenopathy. Morbid symptoms such as fever, weight loss, and night sweats in conjunction with generalized adenopathy can be concerning. However, similar symptoms can be normal in cases of localized adenopathy with concurrent Flu or Strep.
- Epidemiology: Details about the patient’s exposure to risky dietary practices, pets, insect bites, recent blood exposure, unprotected sex, drugs injection, occupational exposure to animals, and travel insights, specifically to underdeveloped regions or the Southwest in the United States, are critical.
- Pharmacological exposure: A comprehensive medical history, including prescribed medications, over-the-counter drugs, supplements, and herbal remedies is crucial.
Physical examination may reveal the location of the swollen lymph nodes and their areas of drainage in the body. The examination allows the determination if lymph nodes are localized or generalized, allowing focus on the affected area. For example:
- The nodes in the submandibular area generally drain the tongue, lips, mouth, and conjunctiva.
- Submental nodes typically drain the lower lip, oropharynx, and cheek.
- Jugular lymphadenopathy typically drains the tongue, tonsils, pinna, and parotid gland.
- Posterior cervical adenopathy can be related to the scalp, neck, and skin of the arms and legs.
- The suboccipital nodes and preauricular nodes drain the scalp, head, eyelids, temporal region, and pinna.
- Postauricular nodes drain the scalp and external auditory meatus.
- The right supraclavicular node drains the mediastinum, lungs, and esophagus.
- Axillary nodes chiefly drain the arm, thoracic wall, and breast.
- The epitrochlear nerve roots typically drain the ulnar side of the forearm and hand.
- Inguinal nodes drain the penis, scrotum, vulva, vagina, perineum, gluteal region, lower abdominal wall, and parts of the lower anal canal.
The characterization of the swollen lymph node is also crucial. These can include:
- Tenderness or pain, suggesting an inflammatory process or possible malignant node with hemorrhage.
- Firm rubbery nodes may suggest lymphoma, soft nodes normally signify infection or inflammatory condition, and hard ‘stone-like’ nodes suggest cancer, generally metastatic.
- “Shotty” nodes are small, scattered, and feel like shotgun pellets under the skin. This is common with viral illnesses in children.
- A “matting” configuration is when the lymph nodes appear gathered and linked together. While this can be indicative of malignancy, it is not conclusive.
Testing for Adenopathy
When experiencing symptoms associated with lymphadenopathy (swollen or abnormal lymph nodes), several laboratory tests can be conducted for diagnosis. One fundamental test is the Complete Blood Count (CBC) which examines the number and types of white blood cells in your body. These can often indicate if there’s a bacterial, viral, or fungal infection.
Other tests can check for specific diseases. For example, the Epstein-Barr virus and Cytomegalovirus tests check for mononucleosis, a common cause of lymphadenopathy. HIV serology tests can determine if lymphadenopathy is due to acute HIV syndrome or related issues. Other tests, like the FTA and RPR tests, can check for syphilis.
Various serological tests (which examine your blood serum) can be used to diagnose or rule out specific conditions. For instance, Toxoplasmosis serology can indicate if you have acute toxoplasmosis, a cause of lymphadenopathy. Hepatitis B serology tests can establish if hepatitis B is a factor in your lymphadenopathy, whereas an ANA (Antinuclear Antibody) serology can check for Systemic Lupus Erythematosus (SLE), another potential cause.
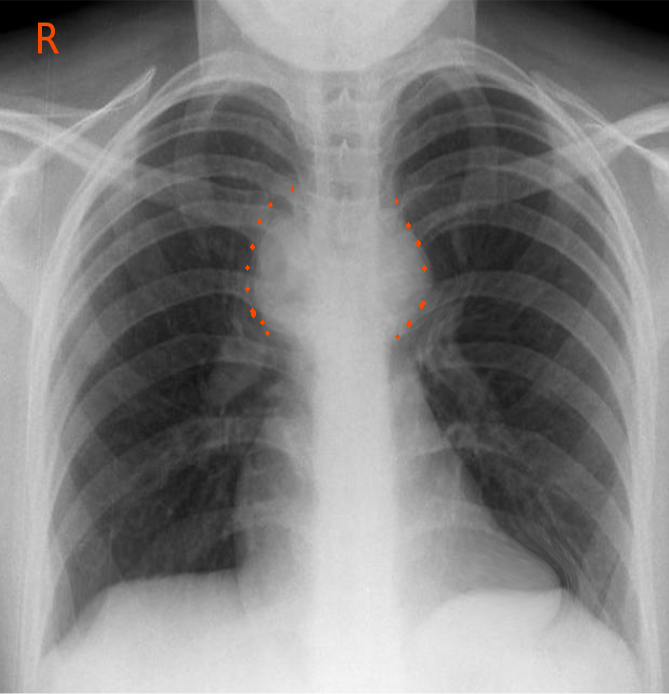
After completing laboratory tests, your doctor might request radiological testing. A chest X-ray can show if diseases like tuberculosis, sarcoidosis, or cancers are present and causing lymphadenopathy. CAT scans of the chest, abdomen, and pelvis can provide more detailed images to help with diagnosis.
Ultrasounds can also be very helpful by assessing the number, size, shape, and internal structure of the affected lymph nodes. Color Doppler ultrasonography is used to differentiate between older and newly active lymphadenopathy. Lastly, an MRI scan can be very useful in evaluating any thoracic, abdominal, and pelvic masses, contributing to an overall understanding of the situation.
It’s important to note that tuberculosis, which can be detected using a PPD (Purified Protein Derivative) test, is a common cause of lymphadenopathy, especially in developing countries.
Treatment Options for Adenopathy
The treatment for lymphadenopathy, which is the term for swollen lymph nodes, depends on what’s causing the swelling. Here’s a look at how treatments might vary:
1. If the swelling is due to a cancer that started in the lymph nodes, the treatment is directed at the cancer itself.
2. If the swelling is due to cancer that has spread to the lymph nodes from somewhere else, doctors will treat both the cancer in the lymph nodes and the primary source of cancer.
3. If a bacterial infection is causing the lymph node swelling, treatment might involve supportive care, antibiotics, and addressing the source of infection (if possible).
4. If a viral infection is to blame, the approach is often to watch and wait, offer supportive care, or treat the virus directly if there are antiviral medications available.
5. If certain medications or exposure to a toxic substance are causing the swelling, the best approach may be to stop taking the offending medication or to avoid the toxic substance.
What else can Adenopathy be?
When it comes to figuring out the cause of swollen lymph nodes, doctors may use several steps to reach an accurate diagnosis. After taking a thorough history and physically examining the patient, they can classify the lymph node swelling into different categories:
- It may be clear what is causing the swollen lymph nodes. For example, if the patient has strep throat or a skin infection, then the lymph nodes may be swollen as a response to that.
- The swollen lymph nodes might suggest a specific condition like mononucleosis, and the doctor can run a test to confirm it.
- Sometimes, the cause of the swollen lymph nodes is not immediately clear.
If the cause isn’t clear, the doctors will need to decide whether the swelling is localized (in one specific area) or generalized (all over the body). If the swelling is localized and the doctor thinks the patient is not at risk of cancer or serious illness, they may decide to monitor the patient for a few weeks to see if the swelling reduces. If there’s a risk of cancer or severe illness, a biopsy might be needed.
If it’s generalized swelling, and the cause is still unknown, the doctor may perform several tests, including a complete blood count, checks for mononucleosis, testing for tuberculosis and sexually transmitted infections, and scans like a chest X-ray. If these tests don’t provide a clear answer, a biopsy might be needed.
One efficient approach to diagnosing swollen lymph nodes is categorizing it by node pattern and location, getting detailed patient history, and carefully evaluating each individual’s case.
Generalized lymph node swelling can be caused by infections like mononucleosis, HIV, tuberculosis, typhoid fever, syphilis, or the plague. It can also be a result of cancers like leukemia or lymphoma, certain metabolic disorders, reactions to medications, or autoimmune diseases like Sjogren syndrome, sarcoidosis, rheumatoid arthritis, or lupus.
When the swelling is localized, its cause can vary depending on the region of the body it’s in. For example, in the head and neck region, it could be due to a viral or bacterial infection, or certain types of cancer. In the groin area, common causes are sexually transmitted diseases, skin infections, or cancers. In the armpit area, causes might include infection, cancer, or even a reaction to a breast implant. Lastly, swelling in the area above the collarbone could be due to certain types of infections.
What to expect with Adenopathy
The outlook for lymphadenopathy, which means swollen lymph nodes, greatly depends on what’s causing the swelling. Most swollen lymph nodes that are seen in regular medical check-ups are due to bacterial or viral illnesses that can be treated. However, conditions like HIV, active tuberculosis and tumors generally have a more uncertain outlook.
Generally speaking, localized lymphadenopathy, where the swelling is confined to a certain area, tends to have a better outlook than generalized lymphadenopathy, where the swelling is widespread. The reason for this is related to the causes of the swelling. Additionally, the sooner the cause is identified in a medical setting, the better the outlook tends to be.
Possible Complications When Diagnosed with Adenopathy
Diagnosing and treating lymphadenopathy (swollen lymph nodes) can be tricky, but here are some important points to bear in mind:
- A thorough history and careful physical examination are crucial in diagnosing lymphadenopathy.
- Most cases of both localized and generalized lymphadenopathy have a treatable cause that isn’t serious.
- Generalized lymphadenopathy always requires careful evaluation and investigation.
- An incisional biopsy, which is a test that takes a small sample of the lymph node, is the most reliable diagnostic tool for lymphadenopathy.
- Taking a detailed note of the patient’s lifestyle and personal medical history can provide clues about whether the lymphadenopathy needs immediate treatment, or can be monitored over a period of 2 to 4 weeks.
- If the lymph nodes above the collarbone (supraclavicular lymphadenopathy) are swollen, this is almost always a sign of a serious illness in the chest or abdomen.
Preventing Adenopathy
Educating patients is key in preventing conditions that can lead to abnormal swelling of the lymph nodes. This instruction can take several forms:
1. Quitting smoking, drinking alcohol in moderation, practicing safe sex, and avoiding drug use can greatly lower the occurrence of diseases like cancer, HIV, hepatitis B and C, and sexually transmitted infections.
2. Getting vaccinated properly, maintaining good hygiene, having good public sanitation, and strictly following infection control practices can greatly reduce recurrence, and the spread of infections that cause lymph node swelling.












