What is Cardiogenic Pulmonary Edema?
Edema is a condition where there’s too much fluid collecting under the skin or inside body cavities. This can be caused by a disturbance among the “Starling forces” or due to a problem or blockage in the body’s lymphatic system, which is responsible for draining fluids.
If edema happens underneath the skin, it can usually be seen as swelling in a part of the body. If it’s in a body cavity, it can result in noticeable symptoms related to that cavity.
Edema can take different forms, including peripheral edema, pulmonary edema, cerebral edema, macular edema, and lymphedema. There are also less common forms, like idiopathic edema and hereditary angioneurotic edema.
Pulmonary edema, in particular, is when too much fluid gathers in the walls and spaces of the lungs. This can be a dangerous condition for some people. It can occur because of cardiogenic reasons which involves disturbances of the forces in the lungs’ blood vessels and tissues, or it can be non-cardiogenic, due to direct injury or damage to lung tissue or blood vessels.
What Causes Cardiogenic Pulmonary Edema?
Cardiogenic pulmonary edema, which is a build-up of fluid in the lungs due to heart-related problems, can be caused by several factors. All these factors contribute to increased pressure and collection of blood on the left side of the heart.
Some conditions that lead to raised pressure on the left side of the heart include coronary artery disease that results in left ventricular failure, congestive heart failure, cardiomyopathy, and heart valve diseases on the left side of the heart. These conditions can increase the pressure in the veins carrying blood to the lungs, which in turn increases the pressure in the lung’s blood vessels, causing fluid to build-up.
Cardiac arrhythmias, irregular heart rhythms, and right to left shunts, which are abnormal pathways between the right and left sides of the heart, can also lead to this condition. These factors all contribute to an escalation in pressure on this side of the heart, leading to pulmonary edema or fluid in the lungs.
Risk Factors and Frequency for Cardiogenic Pulmonary Edema
Pulmonary edema is a serious condition that is primarily associated with heart failure. It affects a large number of people, and it is particularly common in males and the elderly. It is important to understand that this condition can be very severe, with many people being readmitted to hospital and a high mortality rate.
- Pulmonary edema affects 75,000 to 83,000 people out of every 100,000 with heart failure and low ejection fraction.
- About 80% of heart failure patients also have pulmonary edema.
- Approximately 74% of patients with this condition are discharged from the hospital.
- The survival rate one year after diagnosis is about 50%.
- At a follow-up six years after diagnosis, the mortality rate is around 85% among patients with congestive heart failure.
- It is more common in males than females.
- Elderly people are at higher risk of developing pulmonary edema.
Signs and Symptoms of Cardiogenic Pulmonary Edema
Pulmonary edema is a condition where fluid fills your lungs, making it hard to breathe. It can come on suddenly (acute) or slowly over time (chronic). Each type has a different set of symptoms.
If you have acute pulmonary edema, you might experience:
- Severe shortness of breath that gets worse when you exert yourself or lay down
- Feelings of dread or anxiety, especially when lying down
- Gasping for air
- Dizziness and excessive sweating
- A cough, which could mean your edema is getting worse
- Sputum (mucus) that is pink and frothy – a sign of severe disease
- Chest pain, because of a heart attack or ruptured aorta
- Cold, moist skin
On the other hand, chronic pulmonary edema might cause:
- Shortness of breath when you exert yourself
- Breathing difficulty when lying down
- Waking up breathless in the night
- Swelling of your body or legs
- Weight gain
- Fatigue
Ortner syndrome is a condition that can occur alongside pulmonary edema for some. This occurs when an enlarged left atrium in the heart presses down on the recurrent laryngeal nerve, leading to hoarseness.
Doctors can use physical examinations to confirm pulmonary edema. Common findings include:
- A general state of confusion, agitation, irritability
- Excessive sweating and cold extremities
- A posture indicating difficulty in breathing
- Blue lips (cyanosis)
- Elevated blood pressure, which if low, can indicate severe left ventricular systolic dysfunction or cardiogenic shock
- Rapid breathing (tachypnea)
- Increased heart rate (tachycardia)
- Swelling of the lower body (pedal edema), which is generally associated with chronic heart failure
- Shortness of breath and use of additional muscles to breathe
- Short, rapid sounds on inhaling (crackles) in the lungs
- Fast breathing (tachypnea) and signs of a pulse
- Breathing sounds like rhonchi and wheezing
- Abnormal heart sounds including an increased S3, accentuated pulmonic S2, and different types of murmurs based on the valve affected
- An enlarged liver (hepatomegaly) which may be tender, indicative of right-sided heart failure
Chronic congestion may also lead to liver problems and sometimes causes fluid build-up in the belly (ascites).
Testing for Cardiogenic Pulmonary Edema
Pulmonary edema, or fluid buildup in the lungs, can be tricky to diagnose as there’s no single definitive test. Doctors usually start with simpler tests and if needed, progress to more complicated ones to determine the cause.
Blood tests are often a starting point; these can check for conditions like anemia or sepsis, monitor electrolyte levels (which could be disrupted in patients taking diuretics), measure levels of oxygen and brain natriuretic peptide — a substance that’s low in those with heart-related edema.
An ECG is another basic test that checks for heart problems like irregular rhythms or signs of damage.
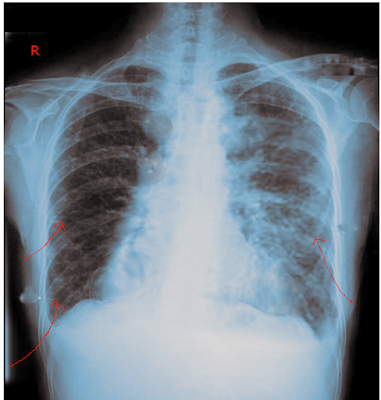
A chest X-ray is crucial in assessing for pulmonary edema. At the early stage, the test can show an enlarged heart, widened blood vessels, and a shift in blood towards the upper part of the lungs. At the intermediate stage, there might be fluid in the lung tissue, “Kerley B lines” (short, horizontal lines near the base of the lungs), fluid around the bronchi, or thickening of lung partitions. If it’s in the late stage, the test might show fluid filled alveoli (air sacs where oxygen and carbon dioxide are exchanged), a “batwing” appearance around the heart, and fluid in the pleural space (between the lungs and chest wall).
Ultrasound can be a good follow-up option to help confirm the diagnosis. For instance, it can differentiate between chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF) as the reason for a sudden worsening of long-term difficulty in breathing.
An echocardiogram is crucial in identifying heart-related causes of pulmonary edema. It can help distinguish between problems with heart muscle contractions or relaxations, and issues with the heart valves.
Invasive techniques like inserting a Swan-Ganz catheter, a thin tube that measures pressures in the heart, may be used. This tube is threaded from a peripheral vein into a branch of the pulmonary artery to measure the pressure in the blood vessels supplying the lungs.
Treatment Options for Cardiogenic Pulmonary Edema
When a patient arrives, there are several important steps that must be addressed for their immediate care:
1. Ensure the patient’s airway is clear for proper breathing and ventilation.
2. Monitor the patient’s breathing patterns and oxygen levels.
3. Check the patient’s vital signs and administer any necessary cardiac care.
4. Deliver oxygen and breathing support if necessary through a nasal cannula, face mask, non-rebreather mask, noninvasive pressure support ventilation or mechanical ventilation.
5. Position the patient upright.
6. Start an intravenous line.
7. Monitor the patient’s urine output.
Once the airway is clear and the patient’s oxygen levels are satisfactory, further care largely depends on the individual’s particular condition. Supplemental oxygen should be provided if the patient has low oxygen in the blood (SpO2 less than 90%). But too much oxygen can cause narrowed blood vessels and a reduction in cardiac output, so it may not be beneficial to give a patient more oxygen than necessary.
If the patient continues to have breathing problems and low oxygen levels, even when receiving extra oxygen, it may be beneficial to try non-invasive ventilation. This method may reduce the need for invasive methods such as intubation and it often improves the patient’s respiratory condition. If the patient doesn’t respond to non-invasive ventilation or cannot have it for medical reasons, moving to invasive intubation and mechanical ventilation may be necessary.
In terms of specific treatment plans, this will depend on managing the root cause of the patient’s condition. Non-invasive management can be achieved by decreasing the amount of blood the heart has to pump through medicines which include nitroglycerin, sodium nitroprusside, isosorbide dinitrate, loop diuretics, morphine and nesiritide.
For patients in acute settings, medical treatment typically involves medications to promote urination to remove excess fluid, possibly combined with medicines that help widen blood vessels. This is particularly true in patients admitted to hospital with acute heart failure.
Patients in the hospital dealing with lung congestion due to fluid buildup are generally managed with medications that promote urination, with a focus on monitoring weight, fluid intake and output, heartbeat, kidney function and electrolytes.
Alongside these, vasodilator therapy may also be necessary. It can help to lower high blood pressure and can improve the effectiveness of diuretics. However, it should be used carefully to avoid low blood pressure and requires careful monitoring.
Invasive management involves treatments such as intra-aortic balloon pumps, ultrafiltration, ventricular assist devices, ECMO, heart transplants, valve replacements, and intubation.
For patients with severe heart failure and cardiogenic shock, mechanical cardiac support can be useful in stabilizing the patient before making a more permanent decision about their care. In these critical circumstances, the choices made by healthcare professionals can mean the difference between life and death. Therefore, all available resources and techniques should be explored before deciding on the most suitable course of action for each individual patient.
What else can Cardiogenic Pulmonary Edema be?
When a doctor is trying to determine the cause of your health issues, there are several other conditions they might consider before making an exact diagnosis. Here are the other conditions they might be thinking of:
- Problems with your lungs causing difficulty in breathing (respiratory failure)
- A heart condition caused by reduced blood flow (myocardial ischemia/infarct)
- A blockage in one of your lung’s main arteries (pulmonary embolism)
- Fluid in the lungs caused by a severe injury to the spinal cord (neurogenic pulmonary edema)
- Fluid in the lungs caused by climbing to high altitudes too quickly (high-altitude pulmonary edema)
- A serious lung condition causing inflammation and fluid build-up (acute respiratory distress syndrome)
It is necessary for the doctor to rule out these possibilities to accurately diagnose your condition.
What to expect with Cardiogenic Pulmonary Edema
The outlook for patients mainly relies on the initial cause, and often it’s not that great. Cardiogenic pulmonary edema, a serious condition, has a discharge rate of 74% and only a 50% survival rate a year after diagnosis. When it comes to congestive heart failure, the statistics are even grimmer, with an 85% mortality rate observed in a 6-year follow-up study.
Possible Complications When Diagnosed with Cardiogenic Pulmonary Edema
Most of the complications linked to pulmonary edema, which is fluid accumulation in the lungs, stem from the problems of its root cause. When the cause is related to heart conditions, the complications can include:
- Increased risk of irregular heart rhythms like atrial fibrillation, ventricular fibrillation, and fast ventricular heartbeats
- Blood clots resulting in pulmonary embolism, deep vein thrombosis, and stroke
- Inflammation of the heart lining, known as pericarditis
- Rupture of heart structures
- Heart valve disease
- Shock due to poor heart function
- Pressure buildup in the heart caused by fluid (tamponade)
- A post-heart attack syndrome called Dressler syndrome
- Death
Pulmonary edema can lead to severe shortages of oxygen in the body (hypoxia and hypoxemia), resulting in damage to organs and even failure of multiple organs. Another frequent issue resulting from pulmonary edema triggered by heart problems is respiratory failure.
Preventing Cardiogenic Pulmonary Edema
Heart problems are the main cause of a condition called pulmonary edema. This is why doctors advise patients to take steps to prevent heart disease from getting worse. Here’s how patients can do this:
* Live a healthy lifestyle and get regular exercise
* Stop smoking
* Stop drinking alcohol
* Keep their weight under control and watch what they eat
* Follow a proper diet
* Eat less cholesterol
* Limit salt intake
* Monitor and control blood pressure
* Maintain a good control of blood sugar levels.