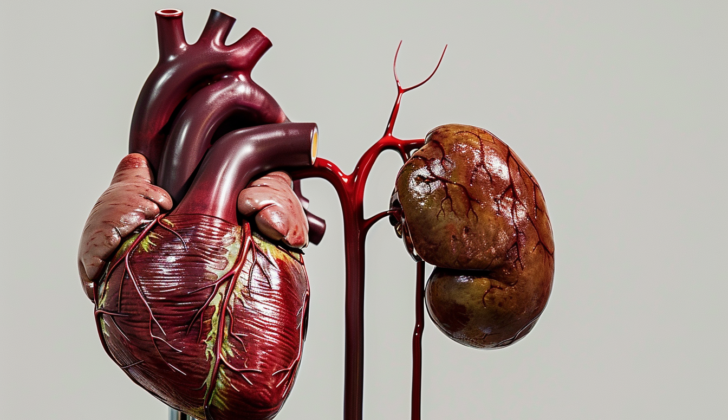
What is Cardiorenal Syndrome?
Cardiorenal syndrome refers to any sudden or long-term issue in either the heart or kidneys that can potentially cause a similar problem in the other organ. The phrase ‘cardiorenal syndrome’ includes various subtypes, which are grouped based on the root cause of the problem and how long the issue has been present.
What Causes Cardiorenal Syndrome?
Cardiorenal syndrome is a condition with five different subtypes:
* Type 1: This happens when heart function suddenly drops, leading to a quick decrease in kidney function.
* Type 2: This is a longer-term issue where problems with the heart over time lead to a steady decrease in kidney function.
* Type 3: This occurs when kidney function suddenly drops, leading to a quick decrease in heart function.
* Type 4: This is a longer-term condition where ongoing kidney problems lead to chronic heart issues.
* Type 5: This happens when diseases that affect the whole body cause both heart and kidney dysfunction.
Each of these types works differently and involve different strategies for management and treatment. The prognosis or expected outcome can also vary for these different types.
Cardiorenal syndrome type 1 is the most common and most studied type.
Risk Factors and Frequency for Cardiorenal Syndrome
In a 2007 study of over 118,000 patients admitted with seriously worsened heart failure, it was found that distinct levels of kidney function were observed. This function is measured by the Glomerular Filtration Rate (GFR), which tells how well the kidneys are working:
- 9.0% of patients had normal kidney function upon arrival.
- 27.4% had mildly impaired kidney function (GFR 60 to 89 mL-min-1.73 m).
- 43.5% had moderate kidney impairment (GFR 30 to 59 mL-min-1.73 m).
- 13.1% had severe kidney impairment (GFR 15 to 29 mL-min-1.73 m).
- 7.0% had a GFR under 15 mL-min-1.73 or were receiving long-term dialysis treatment.
Large databases also suggest a link between the existence of heart or kidney problems and an increased chance of the other occurring.
Signs and Symptoms of Cardiorenal Syndrome
Doctors can often tell the difference between acute and chronic heart or kidney health problems by looking at the patient’s medical history and symptoms. For example, if a patient has recently had a heart event, such as a heart attack, it could lead to serious heart malfunction, which can then harm the kidneys. Alternatively, if the patient has recently experienced severe diarrhea and vomiting, it could damage their kidneys first, which then negatively impacts heart function. Other useful information could include the patient’s medication history and previous test results. Even though it can be hard to identify the different types of heart-kidney conditions through a physical examination, many patients will show signs of fluid overload, such as:
- High jugular vein pressure
- Overall swelling and water accumulation, evident as fluid in the lungs, fluid in the abdomen, or swollen arms and legs
- Sounds of fluid in the lungs when checked with a stethoscope
- Low blood pressure, tiredness, weakened pulses, and abnormal heart rates, which all point to reduced heart function
Other signs that suggest kidney disease as the main cause of the heart-kidney condition could include:
- Pale skin due to anemia
- Reduced or no urine production before any heart difficulties start
Testing for Cardiorenal Syndrome
When a doctor starts looking into the cause of a patient’s symptoms, they usually begin with a general overview and an examination. This helps guide them towards what specific tests might be needed to identify the underlying issue. These tests often include blood tests – such as a complete blood count and a complete metabolic panel – along with tests on a urine sample. They will also likely check the levels of two specific substances, called brain natriuretic peptide (BNP) and troponin.
The doctor can calculate an ‘estimated glomerular filtration rate’ from the levels of a substance called creatinine found in blood test results, which can show how well the kidneys are working. Sometimes, a patient may be indicated to have a condition called “cardiorenal syndrome type 5”, and in these situations, they may also need blood and urine tests to check for possible infections, autoimmune diseases (like lupus), and another substance called ‘procalcitonin’. Further checks for this syndrome would typically include a heart scan and constant heart rate monitoring to find any rhythm problems that might be linked to the syndrome.
An imaging test known as a ‘transthoracic echocardiogram’ is extremely useful as it can spot problems in the walls of the heart, measure the percentage of blood being pumped out of the heart’s main pumping chamber (this is known as the ‘left ventricular ejection fraction’), and check for fluid around the heart. An ultrasound scan of the kidneys can give an idea of how large they are and how well they’re functioning. Certain patterns on a kidney ultrasound, such as smaller size and increased ‘echogenicity’ (or brightness), can suggest a diagnosis of chronic kidney disease.
Treatment Options for Cardiorenal Syndrome
While no treatments have been proven to improve the overall outcome for patients with cardiorenal syndrome, it’s common practice to focus on managing the root cause and complications of this condition. This often involves dealing with excess fluid in the body, which is a symptom typical in those with cardiorenal syndrome. Different methods can be used to remove this extra fluid, either with diuretic medicines or by employing a process called ultrafiltration.
Diuretics, also known as water pills, help your kidneys expel more salt and water into your urine, thus reducing fluid in your body. Powerful diuretics like furosemide, torsemide, and bumetanide are usually chosen. They can be used by themselves or combined with other diuretics. There are two ways to administer these diuretics: either a constant, steady dose or intermittent doses delivered via injection. The correct dosage can be determined using a measure of kidney function, known as creatinine clearance.
For instance, with a particular range of creatinine clearance, one could start treatment with a 40 mg injection of furosemide and then 10 mg per hour after that. Conversely, a larger starting dose of 80 to 160 mg of furosemide might be used, with the potential to repeat this dose various times a day until a favorable response is achieved. There is currently no definite supporting evidence to prefer one strategy over the other.
One benefit of a steady diuretic dose is that it allows medical professionals more opportunities to evaluate how well the treatment is working. If the patient’s body becomes resistant to diuretic therapy, adding a thiazide diuretic may help. Metolazone is often used in this case and is a popular combination with loop diuretics.
Ultrafiltration, a process that removes excess fluid from the body, can have benefits in stubborn cases. However, some recent studies have shown that initially, standard diuretic therapy may be more effective than ultrafiltration in reducing symptoms and lowering creatinine levels.
In the most severe cases, drugs that boost heart function and decrease blood vessel congestion, called inotropes, might be prescribed. However, there’s no definitive evidence supporting their use in the treatment of cardiorenal syndrome.
Lastly, the treatment of types 3, 4, and 5 cardiorenal syndrome would target treating the underlying kidney disease and avoiding things that could damage the kidneys. This includes staying away from certain medications and contrast dyes often used in some imaging tests. It’s also critical to manage any other health conditions that could be contributing to kidney damage or heart problems.
What else can Cardiorenal Syndrome be?
Determining the cause of ‘cardiorenal syndrome’ (a condition that affects the heart and kidneys concurrently) can be challenging. This is because patients often don’t show all the typical signs when they first come to the doctor. However, there are certain clues that can hint towards a ‘hypovolemic’ cause, which basically means the body is dehydrated or lacking sufficient fluids. These clues can include a recent increase in the use of water pills (diuretics), occurrences of diarrhea or vomiting, skin or throat infections, heatstroke, fever, intense physical activity, or the use of certain anti-inflammatory drugs (known as NSAIDs). These factors might indicate that the body is low on fluids, which could be contributing to the heart and kidney problems.
What to expect with Cardiorenal Syndrome
The chances of recovery are generally not good. Many calculators are available that predict patient’s prognosis, which means their likely outcome. These tools use various factors to predict the risk of someone dying in the hospital and the possibility of needing to be readmitted to the hospital.
Some of these factors include the level of blood urea nitrogen (BUN), which is a waste product in the blood; blood pressure when the heart is beating (systolic blood pressure); the amount of a waste product called creatinine in the blood, which can give an idea of kidney health; a substance called brain natriuretic peptide, which is often increased in heart disease; and how well diuretics, medications used to get rid of fluid in the body, are working.
Possible Complications When Diagnosed with Cardiorenal Syndrome
There are several serious health problems that can occur, such as:
- Liver failure
- Respiratory failure, which may require invasive and non-invasive ventilation
- Worsening kidney failure, which may necessitate temporary or permanent dialysis
Preventing Cardiorenal Syndrome
Taking prescribed medications like diuretics and sticking to a specific diet, along with monitoring body weight regularly, are key steps in preventing a recurrence of heart failure. Regular check-ins at a heart failure clinic for proper adjustments to diuretic doses, which help remove excess fluid from the body, are also highly important.