What is Castleman Disease?
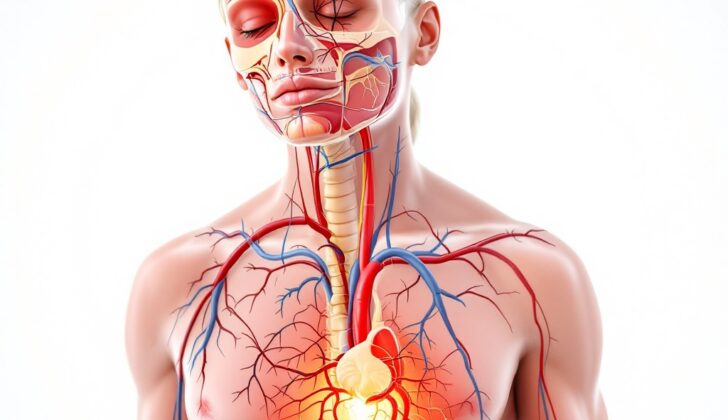
Castleman disease, also known as CD, is a rare disorder that causes abnormal growth of cells in the lymph nodes, which are small glands that produce and store cells that fight infection. The disease can affect lymph nodes anywhere in the body, like the neck, chest, abdomen, and pelvis, and can look like both harmless and harmful growths.
Depending on its cause, how it appears under a microscope, and its symptoms, Castleman disease is divided into several types. It can be classified as ‘hyaline vascular type’, ‘plasma cell type’, ‘mixed type’, and a type associated with human herpesvirus (HHV)-8.
When we look at how CD behaves clinically, it can manifest in two forms. The first is unicentric Castleman disease (UCD), which is more common and affects only one group of lymph nodes. The second is multicentric Castleman disease (MCD), which is less common and affects multiple groups of lymph nodes.
What Causes Castleman Disease?
We don’t know much about what causes this particular disorder, but some evidence suggests it could be due to a problem with the immune system. This problem can cause the immune cells called B lymphocytes and plasma cells to grow too much in places where immune cells are concentrated. Some potential triggers for these conditions could be ongoing, low-level inflammation, unusual growth in lymphoid organs, viral infections, changes in inflammation-controlling substances known as cytokines, and blood vessel formation.
There’s also a strong link between this disease and HIV, which weakens the immune system. In specific conditions like MCD – a type of this disorder, factors causing it can include the human herpesvirus (HHV)-8. This virus can disrupt the regulation of substances that help control inflammation, like CD20 and interleukin (IL)-6.
Almost all cases of the disease connected to HIV also test positive for HHV-8, compared to about 40 to 50% of cases that aren’t linked to HIV. For the remaining cases that don’t relate to HIV or HHV-8, often called idiopathic multicentric CD (iMCD), we don’t yet know what causes them.
Risk Factors and Frequency for Castleman Disease
Castleman disease was a difficult condition to study due to a lack of a formal definition and comprehensive knowledge. However, a study conducted in 2008 unveiled some key details about this disease:
- The occurrence rate (incidence) of unicentric Castleman disease (UCD) is 16 per million patient-years and it can affect people of all ages.
- The incidence of a variant of Castleman disease associated with human herpesvirus-8 (HHV-8) varies greatly. It is more likely to occur in men who are HIV-positive.
- Idiopathic multicentric Castleman disease (iMCD) occurs at a rate of 5 per million patient-years.
A different study conducted in the United States between 2000 and 2009 found some other important details:
- Out of 59 Castleman disease patients, 61% were males and the average age was 53 years.
- Most of the patients (68%) were white.
Between different types of Castleman disease, the hyaline-vascular variant is more common, making up 91% of total cases. Despite these findings, Castleman disease doesn’t show any notable preference for a particular sex or race. Although it often develops in people under the age of 30, it can occur in individuals of varied age groups.
Signs and Symptoms of Castleman Disease
Unicentric Castleman disease is typically a non-cancerous, slow-growing lump at one location in the body. Although it doesn’t initially cause any symptoms, as it grows in size, it can start to press on nearby structures and create discomfort. On the other hand, multicentric Castleman disease can be found at multiple sites in the body and is associated with general signs of inflammation, often referred to as “B symptoms.” These include:
- Fever
- Night sweats
- Feeling unwell
- Weight loss
Overproduction of a protein called IL-6 can lead to a variety of symptoms, such as swollen lymph nodes and an enlarged liver or spleen. It can also lead to excess proteins in the blood, blood clots, anemia, excessive growth of blood vessels, and increases in vascular leakiness. All these can cause swelling and fluid accumulation in the body, potentially even widespread swelling known as anasarca.
In severe cases of a subtype called idiopathic multicentric Castleman disease (iMCD), multiple organs can fail, including the kidneys, which can unfortunately be fatal.
Testing for Castleman Disease
Castleman disease is a challenging condition to diagnose because it doesn’t have specific signs that allow it to be easily differentiated from other illnesses that cause swollen lymph nodes. Thus, a diagnosis would be confirmed when the patient fulfills both major criteria, at least two minor criteria, and exhibits one laboratory abnormality.
First off, the major criteria include the examination of the lymph nodes under a microscope to check if a single node is affected (which could hint at Unicentric Castleman Disease or UCD) or if several nodes are affected (which suggests Multicentric Castleman Disease or MCD). It’s important that other conditions that could cause similar lymph node features like infections, cancer, and autoimmune disorders are ruled out first. Another major criterion is that the lymph node/s should be enlarged.
Meanwhile, the minor criteria can be divided into laboratory and clinical aspects:
Laboratory tests look for abnormalities such as high C-reactive protein or erythrocyte sedimentation rate (markers of inflammation), presence of anemia, issues with platelet count, low albumin levels, kidney issues or presence of proteins in urine, and an abnormal amount of gamma globulins in the blood.
The clinical aspects include symptoms such as fever, weight loss, night sweats, and fatigue, enlargement of the spleen or liver, and accumulation of fluid in various parts of the body.
Additionally, the presence of Interleukin-6 (IL-6) has been proven to be a specific marker for Castleman disease although other substances like soluble Interleukin-2 receptors (sIL2R), Vascular Endothelial Growth Factor (VEGF), certain antibodies, and other proteins may not specifically indicate this disease but are important in supporting its diagnosis.
It’s also essential to conduct tests to check for HIV and HHV-8, as these could be linked to Castleman disease.
To sketch out a treatment plan, a detailed assessment to detect other potentially affected sites should be conducted. This may include a special blood test called serum protein electrophoresis, an examination of the bone marrow, CT scans of the chest, abdomen, and pelvis, a skeletal survey using special X-rays, and a type of scan called a gallium scan. Such information is vital for detecting how widespread the disease might be and to set apart localized from multicentric Castleman disease.
Therefore, a diagnosis of Castleman disease requires close cooperation between the clinical and laboratory teams as it’s only confirmed when all other potential causes of swollen lymph nodes have been thoroughly examined and ruled out. This involves looking not just at the patient’s symptoms and medical history, but also at various laboratory and imaging results.
Treatment Options for Castleman Disease
Castleman disease is a rare condition with few treatment options. When only one lesion or abnormal area is present, known as unicentric Castleman disease, the best course of action is often to surgically remove the lesion.
For multicentric Castleman disease, where multiple lesions are present, there are many different treatment options. These include surgery, chemotherapy with or without steroids, and autologous stem cell transplantation where a patient’s own healthy cells are used to replace diseased or damaged cells. Treatments targeting CD20 and IL-6 pathways and HHV-8 replication have shown promising results.
Monoclonal antibodies, which are substances that can locate and bind to cancer cells wherever they are in the body, are often used to interrupt the IL-6 signaling cascade. This is a biological process that stimulates the growth and spread of cancer cells. Two effective monoclonal antibodies are Tocilizumab, an anti-IL6R antibody, and Siltuximab, an anti-IL-6 antibody. These are typically the first line of treatment, especially for patients who have serious symptoms but are not positive for HIV or HHV-8.
Antiviral medications like ganciclovir, foscarnet, and cidofovir have been shown to be effective against HHV-8 replication pathways, thus they can help in fighting the disease. Other promising treatments that have a limited amount of side effects include rituximab, thalidomide, bortezomib, IL-1 antagonist anakinra, and interferon-alpha. These are all considered immunomodulatory agents, meaning they modify the immune system’s response to help fight disease.
Chemotherapy and immunomodulatory drugs are often reserved for situations where the disease has come back or relapsed. However, it’s important to keep in mind that not all Castleman disease cases will respond to therapy and be fully cured.
What else can Castleman Disease be?
Castleman disease, also known as CD, can be mistaken for lymphoma or other solid tumors. For this reason, it’s crucial to correctly identify the type of Castleman disease someone has. This way, it can be distinguished from other diseases. Medical history, lab tests and imaging techniques play a key role in this diagnosis. While Castleman disease was originally considered a benign, or non-cancerous, disease of the lymph nodes, the systemic forms can be linked with related cancers and autoimmune disorders, such as Kaposi sarcoma and Follicular dendritic cell (FDC) tumours. Certain lymphomas, specifically Hodgkin and angioimmunoblastic T-cell lymphoma, are noteworthy for their ability to resemble Castleman disease.
The hyaline vascular form of Castleman disease shares a strong link with FDC tumors. This type of Castleman disease may result in the production of an immune protein called IL-6 that mimics other molecules. This can trigger an immune response, causing rashes and the generation of autoantibodies. It can also come with a life-threatening autoimmune blistering disease known as paraneoplastic pemphigus, especially in patients with treatment-resistant erosive mucosal lesions.
POEMS syndrome is a rare disease of the plasma cells resulting in multiple organ damage and is associated with neuropathy, organ enlargement, hormone disorders, the presence of a protein known as ‘M protein’, and skin changes. Approximately 30% of individuals with POEMS disease also have multicentric Castleman disease, specifically the HHV-8 positive variant. Many symptoms of systemic Castleman disease, like fluid in the abdomen, swollen lymph nodes, enlarged liver or spleen, and neuropathy also overlap with POEMS syndrome.
Both the HHV-8 associated form of Castleman disease and Kaposi sarcoma are vascular lesions caused by the same virus, HHV-8. This is why they often emerge together in individuals with HIV.
Some diseases that involve the body’s immune protein IgG4, like sclerosing cholangitis, Kuttner tumor, retroperitoneal fibrosis, Mikulicz disease, and autoimmune pancreatitis, are connected to enlarged lymph nodes similar to multicentric Castleman disease. However, these two diseases can be distinguished based on lab results, specifically increased levels of blood IgG4 and IgG4-positive plasma infiltrates in the IgG4-related diseases compared to IL-6 elevation in Castleman disease.
What to expect with Castleman Disease
Patients with UCD, a certain form of the disease, can often find relief with surgical options and usually have a good prognosis, meaning they can expect to live a long time after treatment. However, MCD, another form of the disease, often involves multiple other conditions in the body, and sometimes patients may also have diseases like HIV or HHV-8.
Because of these complexities, doctors have not settled on specific chemotherapy treatment plans for patients with MCD; they need to continue researching more effective treatment methods. Alongside the lack of established cures, the signs of this disease are often too subtle to notice and diagnostic tests do not always detect it, which leads to a delay in determining the illness. Hence, the prognosis—the likely course or outcome of the disease—for MCD is typically poor.
It’s also important to be aware that both UCD and MCD can sometimes worsen into a form of cancer called non-Hodgkin lymphoma.
Possible Complications When Diagnosed with Castleman Disease
Castleman disease can cause different complications depending on its type. This was shown in a study of 53 patients with Castleman disease, where it was found that only 32 of those patients had complications that affected their skin, blood cells, or internal organs.
Two of the most serious complications that can occur with one type of Castleman disease (UCD) are paraneoplastic pemphigus (PNP) and bronchiolitis obliterans (BO), which are both rare diseases.
Differences with another type of Castleman disease (MCD) include complications related to blood cells (such as clotting disorders and inflammatory reactions) and internal organs (such as kidney and liver damage).
Patients who don’t have these complications have a significantly higher survival rate. This emphasizes the importance of an early diagnosis to provide the best treatment options and improve patients’ outlook.
- Patients with UCD may face complications like PNP and BO.
- MCD patients may experience blood cell and internal organ complications.
- Patients without these complications have a better survival rate.
- Early diagnosis is crucial to provide appropriate treatment and improve prognosis.
Preventing Castleman Disease
If you notice any swelling in your lymph nodes that lasts for a long time, it’s important to have a doctor check it out immediately. This advice is especially crucial for those with a history of HIV or HHV-8, which are types of viruses that can weaken the immune system and affect the body in various ways. If you have MCD, which stands for Multicentric Castleman disease, a rare disorder that involves an overgrowth of cells in the body’s lymph nodes, regular doctor’s visits are needed to prevent any serious or life-threatening complications.