What is Dural Arteriovenous Fistula?
Dural arteriovenous fistulas (dAVF) are abnormal blood vessels where arteries, usually from the carotid or vertebral arteries, drain directly into areas of the veins in the dural leaflets, which are part of the brain’s coverings. These conditions might also be called dural arteriovenous malformations. They often occur above the tentorium (the partition between the brain and cerebellum), rather than below it. The most common place they appear is at the junction between the transverse and sigmoid sinuses, with a slight bias toward the left side. They can also occur in various other areas, including the tentorial, petrosal, ethmoidal, Sylvian, cavernous sinus, spinal dura, and superior sagittal sinus regions. If they happen in the cavernous sinus, they are called carotid-cavernous fistulas.
The dAVF can behave in different ways clinically, and their impact, including the risk of increased pressure within the skull and bleeding, mainly depends on the patterns of the venous drainage. If there is cortical venous drainage, this could lead to a very serious disease progression. The most aggressive dAVFs are often in the tentorial region, followed by the Sylvian/middle fossa and ethmoidal/anterior fossa regions. The Borden and Cognard classifying systems are widely used to predict how aggressive a dAVF is likely to be.
What Causes Dural Arteriovenous Fistula?
Most dural arteriovenous fistulas, or dAVFs, often don’t have a known cause. However, evidence suggests that many are likely formed after conditions such as a clot in the dural sinus (part of the brain), trauma, infection, or previous brain surgery.
Those dAVFs that involve the larger veins in the brain typically result from a gradual narrowing or blockage in one of the brain’s venous sinuses. These sinuses are important paths that bring used blood from the brain back to the heart.
Risk Factors and Frequency for Dural Arteriovenous Fistula
Dural arteriovenous fistulas, or dAVFs, are medical conditions that can occur at any age, but they are most commonly diagnosed in people between 40 and 60 years old. But it’s important to note that younger people, including children, can also develop dAVFs. Each year, there are about 0.15 to 0.29 cases per 100,000 people. dAVFs make up 10 to 15% of all brain blood vessel malformations.
- dAVFs can happen at any age but typically occur in people aged 40 to 60.
- However, they can also develop in younger age groups, including children.
- Each year, there are about 0.15 to 0.29 cases of dAVFs per 100,000 people.
- dAVFs are responsible for 10 to 15% of all brain blood vessel malformations.
Signs and Symptoms of Dural Arteriovenous Fistula
When doctors check a patient who may have a dAVF (dural arteriovenous fistula), they perform a thorough examination of the nervous system. This is a part of the larger medical examination done to identify the surgical risks the patient might have.
Interestingly, some individuals with a dAVF may not show any symptoms. Often, these cases are found during brain scans that are being conducted for unrelated medical conditions. Some dAVFs show no symptoms for prolonged periods, while others may even naturally disappear.
However, for those who do experience symptoms, they may be categorized as either mild or severe. These symptoms can include one or more of the following:
- Headache
- Nausea/vomiting
- Seizures
- Cranial neuropathies (nerve malfunctions)
- Pulsatile tinnitus (hearing your heartbeat in your ear)
- Intracranial hypertension (increased pressure around the brain)
- Papilledema (swelling of the optic disc)
- Glaucoma
- Hydrocephalus (build-up of fluid in the brain)
- Intracerebral hemorrhage (bleeding in the brain)
- Speech or language issues
- Coordination issues
- Altered sensations
- Weakness
- Face pain
- Dementia
- Parkinsonism (conditions that cause movement problems like those seen in Parkinson’s disease)
- Apathy
- Vision problems
- Proptosis (bulging eyes)
Testing for Dural Arteriovenous Fistula
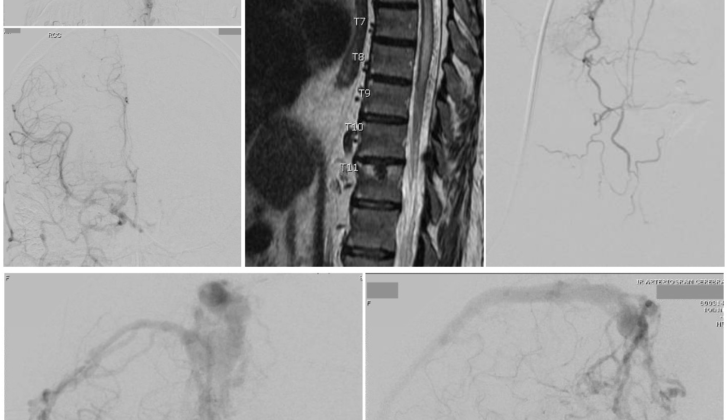
When doctors suspect dural arteriovenous fistulas (dAVFs), they typically use imaging studies such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA). These tests can highlight abnormal blood vessels, blockages or growths in the blood-filled spaces in your head (sinuses), and swelling or fluid build-up from high blood pressure in veins. The MRA can also show if there is early filling of the sinuses, dilated vessels on the surface of the brain, and swelling from venous hypertension. Sometimes, up to half of patients may show this kind of swelling in the membranes covering the brain and spinal cord, even without ‘back-filling’ into the surface veins of the brain (cortical retrograde filling). If there is high pressure in the venous sinuses, they might also identify hydrocephalus, a build-up of brain fluid.
To make a final diagnosis and plan treatment, a six-vessel digital subtraction angiogram (DSA) needs to be done. This technique can show the doctors clear details about the fistula, especially in the face and neck arteries, the condition of the sinuses, and which veins are affected.
Doctors often use the Borden Classification system to categorize the dAVFs based on how the blood flows and whether there is cortical venous drainage. There are three types:
+ Type I: The blood flows forward into a dural venous sinus or membrane vein. They usually don’t cause problems in the long term.
+ Type II: There is forward flow into a dural venous sinus and backward flow into the cortical veins. The likelihood that they will behave aggressively or dangerously is about 39%.
+ Type III: The blood only flows backward from the fistula into cortical veins, causing high pressure in the veins. They behave aggressively in around 79% of cases.
Another way doctors categorize dAVFs is using the Cognard classification. According to it, dAVFs fall into seven categories, based on whether the blood flows backward or forward, the location of the fistula, whether there is drainage into the cortical veins, and whether there are enlarged veins.
The categories are as follows:
+ Type I: They are inside a sinus, have forward blood flow, and no cortical drainage. They usually follow a harmless course.
+ Type IIa and IIb: They cause backward flow into the sinus or forward flow with reflux into cortical veins, respectively. They have a 20% and 10% risk of increased pressure inside the skull and bleeding due to venous reflux.
+ Type IIa+b: They cause backward flow with reflux into cortical veins. They present a 66% risk of bleeding and potentially, higher pressure in the skull.
+ Type III and IV: They drain directly into a cortical vein, with or without venous enlargement, carrying a 40% and 65% risk of bleeding respectively.
+ Type V: They drain directly into spinal cord veins. Half of these patients may present with a progressively worsening condition affecting the spinal cord.
Treatment Options for Dural Arteriovenous Fistula
Deciding whether to treat dural arteriovenous fistulas (dAVFs), abnormal connections between arteries and veins in the brain’s protective covering, depends on the patient’s symptoms, pre-existing health conditions, and the risk of severe brain pressure or bleeding. If the lesions have no symptoms and are low-grade, they generally don’t cause significant problems and are usually monitored regularly rather than treated. But when lesions are high-grade, cause symptoms, or draining into veins in the brain’s outer layer, treatment is considered. There are three main treatment measures, namely open surgery, endovascular embolisation, and stereotactic radiosurgery.
The goal of any treatment is to entirely disconnect the abnormal connection between the artery and vein. If this isn’t done correctly, other arteries may be drawn to the fistula, potentially continuing to cause symptoms or risk of bleeding.
During surgical treatment, the surgeon disconnects the artery from the vein. Sometimes, they’ll need to remove a piece of the protective layer of the brain or use packing techniques to stop blood flow. Surgery is typically recommended if endovascular approaches have not succeeded, or aren’t viable.
Endovascular surgery involves using materials or coil-like devices to seal off the abnormal connection between the artery and vein in the brain. The goal is to entirely eliminate this abnormal bridge. Depending on the specifics of the case, the treatment can be done through the artery (transarterial) or vein (transvenous).
Stereotactic radiosurgery is another option. It’s very effective in treating low-grade dAVFs, and especially useful for patients who have persistent symptoms like a strong pulsating sound in the ears. This method might also be chosen for dAVFs where the anatomy makes other interventions challenging, for patients with significant health conditions, or as a backup option when surgery or endovascular treatment hasn’t fully worked. Here, the area is subjected to radiation, leading to blood clot formation and closing down the abnormal connection. However, this treatment might take several months to years to show results, and there’s a risk of bleeding until the final recovery.
What else can Dural Arteriovenous Fistula be?
These are some medical conditions that might affect the brain or its blood vessels:
- Cerebral arteriovenous malformations (a disorder that causes irregular connections between arteries and veins in the brain)
- Cavernous malformations (a condition where blood vessels in the brain form abnormally, creating a ‘cavern’ that can bleed or leak)
- Highly vascular tumors (abnormal growth that has a large number of blood vessels)
What to expect with Dural Arteriovenous Fistula
The outcome of a neurological issue largely depends on the severity of the symptoms and deficits experienced. For many patients, pulsatile tinnitus—a condition that involves hearing a rhythmic, sometimes heartbeat-like sound in the ears—can be resolved by sealing off the fistula (an abnormal connection, in this case between blood vessels). Both seizures and visual issues typically see major improvements after treatment. While strokes cannot be cured, steps can be taken to prevent any new neurological issues from developing.
Once the fistula is efficiently sealed off and blood can no longer flow backwards into the brain’s cortex, any swollen areas and high blood pressure will generally improve and return to normal. However, both surgical approaches and non-surgical interventions using a catheter, known as the endovascular approach, do come with potential complications which could worsen the patient’s condition. There are also potential complications linked with radiosurgery—a type of radiation therapy—including radiation necrosis, a serious issue where tissue dies due to radiation.
Disease grading scales such as Borden and Cognard differentiate among more severe cases (grades II and III for Borden and grades IIb-V for Cognard), which carry an annual death rate of about 10% and an 8% yearly risk of bleeding within the brain. These severe cases also carry an approximately 7% annual risk of experiencing non-bleeding related neurological problems.
Possible Complications When Diagnosed with Dural Arteriovenous Fistula
These are some of the conditions that could occur in the brain:
- Bleeding within the brain tissue (Intracerebral hemorrhage)
- Blood clots underneath the protective covering of the brain (Subdural hematomas)
- Bleeding in the space between the brain and the tissue covering the brain (Subarachnoid hemorrhage)
- Increase in the pressure inside the skull (Increased intracranial pressure)
- Uncontrollable shaking caused by electrical disturbances in the brain (Seizures)
Preventing Dural Arteriovenous Fistula
Having a dural arteriovenous fistula, which is a type of blood vessel abnormality, can lead to significant physical and mental health issues. This condition can dramatically lower the quality and length of a person’s life. Symptoms often include bleeding within the brain, which can affect speaking and moving abilities, depending on where and how big the bleed is.
Patients must have a solid understanding of their diagnostic results and how their condition is likely to progress, including the risk of more bleeding. This knowledge helps them make informed decisions. Patients should also be aware that any damage caused by lack of blood supply (ischemic injuries) is permanent, but with proper treatment, no further harm should occur.
The patients with permanent damage will need physical, occupational, and speech therapy to cope. If a decision is made not to treat the blood vessel abnormality immediately, it’s crucial to closely monitor the patient’s symptoms, looking out for any new symptoms or worsening of existing ones.