What is Granulomatous Uveitis?
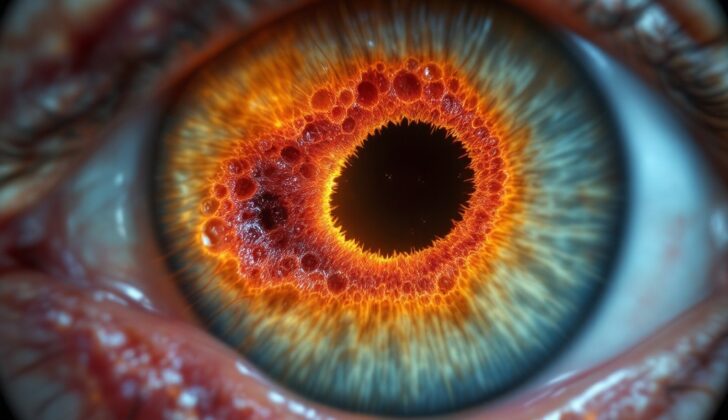
The uvea, or the middle layer of the eye, is made up of three parts – the iris, the ciliary body, and the choroid. The term ‘uvea’ is derived from the Greek word ‘uva’, meaning “grape”. Uveitis refers to the inflammation of this middle layer of the eye and can involve any combination of the three parts of the uvea.
There are several ways to categorize uveitis. Based on the location of inflammation in the eye, it can be termed as anterior, intermediate, posterior, or panuveitis. Depending on the cause of uveitis, it can be classified as infectious or non-infectious. Additionally, based on how the body reacts to the cause, it can be characterized as granulomatous or non-granulomatous uveitis.
Several different conditions, related to either the eye or the entire body, can result in uveitis. Therefore, these classifications are helpful because they can potentially narrow down what might be causing the uveitis, as each condition typically has its unique symptoms. In this discussion, I will go through the different ways to identify and manage granulomatous uveitis.
What Causes Granulomatous Uveitis?
There are many medical conditions that can cause granulomatous inflammation of the uveal tract, which is the layer in your eye that contains the iris, ciliary body, and choroid. These conditions can be either infectious or non-infectious.
Infectious causes are conditions triggered by a harmful microorganism in the body. These conditions include Tuberculosis, Syphilis, Herpes viruses, Cytomegalovirus, Lyme disease, Toxoplasmosis, Toxocariasis, Trematodes, Propionibacterium acnes, Post-streptococcal infections, and some types of fungal infections, including Candida, Histoplasmosis, and Cryptococcosis. Some of these can follow coronavirus disease-2019 as well.
On the other hand, non-infectious causes are conditions not triggered by harmful microorganisms, and can be due to various other reasons. They include Sarcoidosis, Multiple sclerosis, Vogt-Koyanagi-Harada disease, Sympathetic ophthalmia, Lymphoma, Blau syndrome, Histiocytosis, Granuloma annulare, and a
reaction to the presence of lenses or drugs such as brimonidine and pembrolizumab.
Incriminating causes could also be unknown as in the case of multifocal choroiditis, common variable immune deficiency, juvenile idiopathic arthritis, high-density silicone oil tamponade, intraocular foreign bodies including caterpillar hair, and tattoo-associated granulomatous uveitis.
Risk Factors and Frequency for Granulomatous Uveitis
Granulomatous uveitis, an inflammatory eye condition, is influenced by several factors including cause, location, and ethnicity. Its occurrence varies worldwide, with certain patterns linked to specific populations and locations. For instance, tuberculosis is prevalent in places like India and Egypt where it’s a common cause of this condition. In contrast, it’s rarely the cause in developed countries like the United States, although there has been a recent increase due to the HIV epidemic.
The disease also varies with ethnicity and location. Sarcoidosis, another condition causing granulomatous uveitis, is more common in Black populations than White, but less frequent in Asians. On the other hand, Vogt-Koyanagi-Harada disease commonly triggers non-infectious uveitis among Asians. In regions such as Asia, South America, Central America, and parts of Africa, Toxoplasmosis is a frequent reason for uveitis. Additionally, Trematode-induced granulomatous uveitis is especially prevalent in Egypt and India, while Lyme disease is typically found in North America and Europe. Meanwhile, Blau syndrome is primarily seen in White populations.
Signs and Symptoms of Granulomatous Uveitis
A patient’s medical history is a key component in evaluating uveitis, a disease that causes inflammation inside the eye. This history allows for more accurate examinations and guides further tests. For example, symptoms like coughing or difficulty breathing could hint at diseases such as tuberculosis or sarcoidosis. Certain details from a person’s sexual history could suggest syphilis or herpes. History of a tick bite followed by a unique “bulls-eye” rash might suggest Lyme disease, especially if the client lives in an area where this disease is common. Nevertheless, exposure to cats can be a hint of toxoplasmosis. If a patient has traveled to an area where tuberculosis is common or had an injury in the other eye, these particular conditions might be the only clue to the diagnosis. Adjusted examinations by the specialist according to the main complaints and symptoms of the patient are necessary.
Patients with uveitis typically show symptoms like blurred vision, eye pain, redness, and sensitivity to light. These symptoms depend on where exactly the inflammation is located inside the eye. For instance, a detailed examination of the front part of the eye in patients with granulomatous uveitis may show an inflamed eye, a change in eye pressure, large deposits on the back of the cornea, flare-ups and cells in the front part of the eye, granulomas, cataracts, especially in the rear part of the lens, surgery history in particular uveitis cases, and cells in the front part of the vitreous humor.
Examinations of the back of the eye might show inflammation of the jelly-like substance in the eye, cloudy vitreous humor, perivascular exudates, retinal bleeding in cases of retinal vasculitis, cystoid macular swelling, and optic disc swelling. Some of the symptoms could be related to the back of the eye and associated complications such as choroidal neovascularization, retinal neovascularization, and epiretinal membranes. Certain signs can be related to specific conditions.
When possible, diagnostic criteria can aid in determining specific causes of granulomatous uveitis. These criteria generally comprise both clinical findings and investigative discoveries.
Testing for Granulomatous Uveitis
Laboratory tests are often the starting point to identify what’s causing a condition known as uveitis, which is an inflammation inside your eye. These tests look for signs of what might be causing the inflammation, and the tests your doctor orders will depend on your symptoms and medical history. It’s important to know accurately how likely a test is to give true results because false results might lead to a wrong diagnosis and incorrect treatment. General tests that most patients will get include a complete blood count, and tests for inflammation known generally as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
Lab tests will also look for possible infectious causes of uveitis, which could range from tuberculosis, syphilis, herpes, cytomegalovirus, borrelia, and toxoplasma, to others. This is done by checking for antibodies (which are defense elements your body makes against things like pathogens) against these infectious agents in your blood.
Additionally, laboratory examinations might be used to find out if non-infectious diseases might be causing your uveitis, like sarcoidosis (an inflammatory disease that could affect any organ in your body) and multiple sclerosis (the disease that damages the protective covering of nerve cells in the brain and spinal cord). Sometimes, these tests are required before starting certain treatments.
In addition to lab tests, imaging scans like X-rays, computed tomography (CT), and magnetic resonance imaging (MRI) scans help doctors detect or rule out certain infective and non-infective conditions that could cause your eye inflammation. A biopsy, which is taking a small portion of tissue for further examination, is another useful diagnostic tool.
Doctors can examine parts of your eye by taking small samples of fluids from the eye chamber, this fluid gives information about the specific cause of the inflammation. Doctors can examine this fluid in detail to identify if there are antibodies against any specific organisms, or even look for DNA or RNA of various infectious agents.
Imaging techniques like B-scan ultrasonography, confocal microscopy, fluorescein angiography, optical coherence tomography, and indocyanine green angiography help doctors to evaluate your condition further.
Sometimes, a biopsy may also be taken from sections of eye tissues. This is helpful in diagnosing the cause of your condition, particularly those that are not easily identified by standard tests. But the use of this method will depend on the expected cause of your uveitis.
Treatment Options for Granulomatous Uveitis
Granulomatous uveitis, a type of inflammation of the eye, is treated with varied approaches, including addressing the eye directly, treating the body as a whole, and managing any complications that may arise.
In terms of direct treatment of the eye, your healthcare provider may use topical treatments like eye drops that contain steroids or other medicines to reduce inflammation. If the inflammation is stubborn, they might consider injections into or around the eye to deliver medication straight to the inflamed area. When infection is causing the inflammation, specific antibiotics or antifungals may be injected into the eye. For persistent inflammation, substances that can decrease the immune response, called immunosuppressants, might be used. In some cases, surgical procedures might be necessary, such as removing a part of the eye lens that is causing inflammation.
While treating the eye directly, it’s also essential to deal with any underlying conditions that may be causing the inflammation. This overall body treatment often involves medications like steroids or immune system-modulating drugs. For instance, if the inflammation is resulting from non-infectious conditions, physicians might use medications like cyclosporine or methotrexate. On the other hand, if the cause is an infection, they might take a different approach, using anti-microbial medications such as penicillin for syphilis or acyclovir for herpes-induced uveitis. There are also drugs called biologics, which can be helpful in some non-infectious uveitis. If a certain medication is causing the uveitis, it should be stopped.
Lastly, complications from granulomatous uveitis must be managed. For instance, cataracts, a clouding of the eye’s lens that can be a complication of this condition, might need to be surgically removed. Glaucoma, a condition of increased pressure in the eye, might be managed with eye drops or even surgery in some instances. Additionally, eye injections are available for complications like macular edema (swelling in a specific part of the retina in the back of the eye) or abnormal vessel growth. When retinal issues occur, such as non-healing bleeding in the eye or blockage of vision from internal eye structures, a type of surgery called vitrectomy might be needed to clear the vitreous, a jelly-like substance in the middle of our eyes.
What else can Granulomatous Uveitis be?
When looking at eye conditions, particularly those involving the uvea (the middle layer of the eye), doctors may consider multiple potential diagnoses, such as:
- Non-granulomatous uveitis: an inflammation of the uvea which doesn’t involve granulomas (small areas of inflammation)
- Pigment dispersion syndrome: a condition where pigment granules from your iris (the colored part of your eye) circulate around the eye
- Uveal melanoma: a type of cancer that develops in the cells that produce pigment in the eyes
- Uveal metastasis: cancer that has spread to the uvea from another part of the body
- Retinoblastoma: a rare type of eye cancer that usually develops in early childhood
- Intraocular lymphoma: a type of cancer in the lymphatic system, which can affect the eyes
- Bilateral acute depigmentation of the iris: a condition where both irises abruptly lose their pigment or color
What to expect with Granulomatous Uveitis
The outcome for granulomatous uveitis, an eye inflammation condition, can vary greatly depending on what’s causing it and how severe it is. Identifying the problem early on and treating it can significantly improve the condition, and could even prevent serious complications that might threaten your vision or your life.
Possible Complications When Diagnosed with Granulomatous Uveitis
Common complications that can result from eye diseases and surgical procedures include:
- Cataract, particularly posterior subcapsular cataract
- Posterior synechia (these are adhesions that can develop behind the iris, potentially closing off the pupil)
- Peripheral anterior synechia (these are adhesions that can affect the perimeter of the iris)
- Cyclitic membrane (a layer of tissue developing as a result of inflammation in the eye)
- Ocular hypotony (a condition where the eye pressure is too low)
- Secondary open-angle glaucoma (an optic disc damage resulting from fluid build-up in the front part of the eye)
- Secondary closed-angle glaucoma (a condition where the iris blocks fluid from draining out of the eye)
- Steroid-induced glaucoma (a kind of glaucoma that became worse due to steroid medications)
- Cystoid macular edema (a condition where fluid accumulates in the retina, affecting vision)
- Epiretinal membrane (a thin film that develops over the macula, the center of the retina)
- Choroidal neovascularization (the growth of new blood vessels that can lead to bleeding or scarring retina)
- Retinal vasculitis (inflammation of the blood vessels in the retina)
- Retinal neovascularization (the growth of new abnormal blood vessels in the retina)
- Vitreous hemorrhage (bleeding into the clear gel that fills the space between the lens and the retina)
- Retinal detachment (a condition where the retina pulls away from the back wall of the eye)
- Macular hole (a small break in the macula, affecting central vision)
- Band keratopathy (a specific type of corneal degeneration)
- Amblyopia (a loss of vision in one eye due to the eye and brain not working together effectively)
- Systemic complications related to the underlying diseases such as arrhythmias in heart conditions like cardiac sarcoidosis.
Preventing Granulomatous Uveitis
People diagnosed with granulomatous uveitis should learn about their condition. Granulomatous uveitis is an eye inflammation that can affect one’s overall health. It’s essential to understand its effects, its likely outcomes, and the complications that can arise from this condition. It’s also important to understand the treatment process along with its associated side-effects.
Staying on track with treatment plans and regular check-ups is extremely crucial in managing granulomatous uveitis. Frequent medical consultations allow early detection and cure of any eye complications, as well as monitoring for any other health issues that may occur as a result of the condition or its treatment.
For those who are on systemic medications (drugs that work throughout the body), routine lab tests may be necessary. These tests help doctors track and manage any negative side effects caused by these medications, ensuring their patients’ safety.