What is Hepatitis D?
The Hepatitis D virus (HDV) was first identified in 1977 in patients who also had chronic Hepatitis B virus (HBV) infection. At first, it was thought to just be a part of the HBV, but later research revealed that the HDV was actually a separate virus, initially referred to as the “delta agent”. An interesting feature of HDV is that it’s considered a hybrid virus: it uses a protein from the Hepatitis B virus for its protective outer layer, which means it can only infect people who also have HBV.
For reasons that are still not completely understood, the presence of the HDV seems to slow down the replication of HBV in the body. So, people infected with HDV usually have a less active HBV infection.
What Causes Hepatitis D?
HDV infection, or Hepatitis D, can cause both short-term and long-term inflammation, typically spread through blood-to-blood contact. The virus reproduces itself in liver cells, but for it to spread, it requires another type of Hepatitis virus, HBsAg. Liver cell death can happen as a result of the virus’ direct harmful effects, or due to the body’s own immune response.
It’s not common for the infection to be transmitted from a mother to her baby during childbirth. The main risk factors include blood transfusions and the use of intravenous drugs, where equipment like needles are shared.
Risk Factors and Frequency for Hepatitis D
Even though the spread of the Hepatitis D virus (HDV) relies on the Hepatitis B virus (HBV), its spread across the world is not the same as that of HBV. This difference is due, in part, to the way it spreads. HDV is mainly passed on through exposure to blood or blood products. It is not often spread through sex, even between men, and it is very rare for it to be passed from mother to child during birth. The data on how HDV spreads usually comes from people with HBV who are also infected with HDV. It’s estimated that 5% of people who carry HBV are also infected with HDV.
In recent years, there has been a significant decrease in the spread of HDV due to fewer cases of HBV infection. This decrease is mainly thanks to better living conditions, more awareness about how infectious diseases spread, and higher rates of HBV vaccination. HDV is most common in certain areas: the Mediterranean, East Africa, the Amazon basin, the Middle East, Central and Northern Asia, and some parts of the Pacific. In Western countries, HDV infection is not common and only occurs in people at high risk, such as intravenous drug users, people from areas where HDV is common, and people who have had multiple blood transfusions.
Signs and Symptoms of Hepatitis D
Hepatitis D is a type of liver infection caused by a virus. Many people don’t exhibit symptoms of this disease. However, if symptoms do occur, they might include fever, stomach pain, feeling sick, vomiting, yellowing skin or eyes (jaundice), confusion, easy bruising, or unexplained bleeding. The consequences of these symptoms largely depend on how severe the infection is.
- Fever
- Stomach pain
- Feeling sick
- Vomiting
- Yellowing skin or eyes (jaundice)
- Confusion
- Easy bruising
- Unexplained bleeding
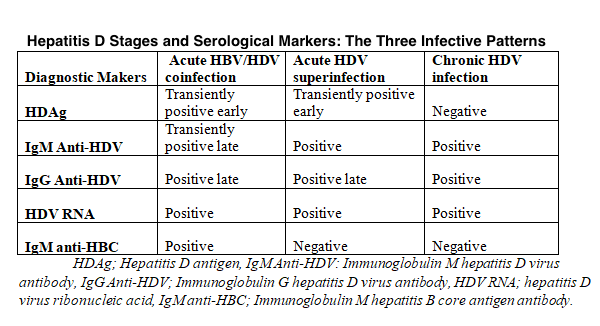
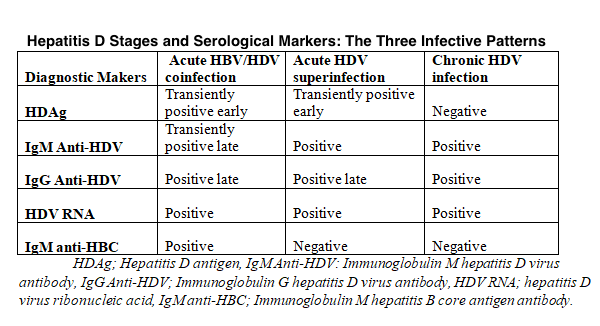
three infective patterns vary in appearance and levels of HDV RNA, HDAg, and
anti-HDV and HBV markers.
Testing for Hepatitis D
When the body encounters the hepatitis D virus (HDV), it produces two types of antibodies – Immunoglobulin M (IgM) and Immunoglobulin G (IgG). These antibodies combat the virus. How they appear and in what quantity depends on the type of HDV infection. Because HDV needs the hepatitis B virus (HBV) to multiply, doctors look for the presence of the HBV surface antigen (HBsAg) to confirm an HDV infection.
In an acute HDV infection, the virus will make its presence known early but briefly, meaning tests might need to be repeated for detection. Antibodies against the HDV typically appear late in the infection and might be the only way to confirm acute HDV if other markers of the infection aren’t present. The format of IgM anti-HDV can vary depending on the progression of the infection. If the infection is improving, anti-HDV IgM appears late and briefly, but if the infection becomes chronic, these antibodies will be around in large numbers and for a long time. However, they aren’t very specific as they’re also found in chronic HDV infection.
Doctors used to look for the infection marker HDAg for an active HBV infection. But the detection process was challenging and time-consuming as anti-HDV form immune complexes with HDAg. Now, the most sensitive and practical test is detecting HDV RNA via a scientific process called reverse transcriptase-polymerase chain reaction (RT-PCR).
High-risk groups, like intravenous drug users or those from HDV-endemic areas, who also have acute hepatitis B, should be suspected of having an HDV coinfection. Also, if someone with chronic hepatitis B has an undefined cause of the illness, they should be tested for HDV to rule out a combined infection with hepatitis B and D. If a person already has chronic hepatitis B, they should also be checked for concurrent chronic HDV infection if they are in a high-risk group. Usually, a test for the presence of total anti-HDV antibodies followed by confirming HDAg and/or serum HDV RNA level measurement can do this. As an added side note, if a person has chronic HDV infection, they typically have the hepatitis B e-antibodies (anti-HBe), which often show suppressed HBV replication.
Treatment Options for Hepatitis D
Finding the best treatment for HDV, or Hepatitis D, can be challenging because there is no known cure. There are no available treatments for a sudden, or acute, outbreak of HDV. However, promising results have emerged from clinical trials using a substance called interferon alpha (IFN alpha). This isn’t officially approved by the Food and Drug Administration (FDA) for chronic HDV yet, but it’s recommended by medical experts.
IFN alpha is given as a weekly injection for at least a year. The treatment aims to halt the spread of HDV within the body. We know it’s working if the virus and the Hepatitis D antigen (a substance produced by the virus) can no longer be detected in blood and liver tests. Successful treatment also results in normal levels of a liver enzyme called alanine aminotransferase (ALT) and reduced liver inflammation, assessed by a liver biopsy. If the disease advances to a stage called cirrhosis, where the liver is heavily scarred, a liver transplant is the only effective treatment.
What else can Hepatitis D be?
When trying to identify Hepatitis D (HDV), doctors also look at these potential health conditions due to their similar symptoms:
- Alcoholic hepatitis
- Autoimmune hepatitis
- Budd-Chiari syndrome (a rare liver condition)
- Cholangitis (inflammation of the bile ducts)
- Cholecystitis (inflammation of the gallbladder)
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Liver abscess
These potential diagnoses need to be ruled out through additional testing before a final diagnosis of HDV can be confirmed.