What is Hypoalbuminemia?
Albumin is a type of protein that is very common in the plasma, which is a part of your blood. Adults usually have between 35 to 50 grams of albumin in every litre of their blood. It’s a single chain of 585 components, known as amino acids, in a circular structure. Albumin is made entirely by your liver and takes about 21 days to get replaced. Your liver usually makes about 10 to 15 grams of albumin each day.
Its production is often stimulated by hormones, like insulin and growth hormone. Sometimes, substances that cause inflammation, like interleukin-6 and tumor necrosis factor, can slow down albumin production. In babies before they are born, the liver and yolk sac (an early source of blood cells) produce a protein quite similar to albumin called alpha-fetoprotein. This protein is thought to be the baby’s version of albumin and they are both controlled by genes that are found close by on a particular chromosome (a structure that carries your genes).
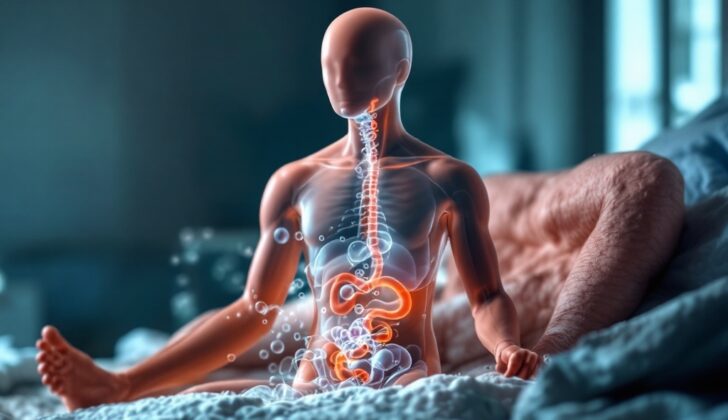
Albumin plays many key roles in your body. It helps to maintain the pressure inside your blood vessels and prevent fluid from leaking out of them. It also carries many different substances throughout your body, in turn reducing their harmful effects, like certain drugs and bilirubin (a substance made from the breakdown of red blood cells) in newborn babies. On top of that, albumin carries around 40% of the calcium in your blood and helps in transporting hormones like thyroxine, cortisol, and testosterone. Albumin also delivers fatty acids and shields your body from damage by harmful molecules known as oxidants. It helps to keep the pH (acidity) of your blood steady too.
Albumin also provides a way to check on a person’s nutrition and the severity of their disease, especially in people who are critically ill or suffering from chronic diseases. About 6% and 10% of albumin can go out of your body through your kidneys and intestines each day. When the level of albumin in your blood falls lower than what’s usually expected, it’s called hypoalbuminemia. This article will tell you about the causes and how to diagnose hypoalbuminemia.
What Causes Hypoalbuminemia?
Hypoalbuminaemia, or low albumin levels in the blood, is a common problem among patients in the hospital or those who are critically ill. This condition can come about for a few different reasons. It could be due to the body not making enough albumin, which is rare, or it could be because the body is losing too much albumin.
Albumin is a protein that our bodies generally make enough of. But in some cases, we might lose more than we should. This can occur through the kidneys, the gastrointestinal (GI) tract, which is long tube running from the mouth to the anus where digestion takes place, the skin, or spaces outside the blood vessels (extravascular space). It’s also possible that albumin is being broken down (or ‘catabolized’) faster than normal in the body.
Sometimes, hypoalbuminaemia could be due to a mix of two or more of these causes. In other words, it’s not always easy to pinpoint one single reason for low albumin levels.
Risk Factors and Frequency for Hypoalbuminemia
Low albumin levels in the blood, also known as hypoalbuminemia, is more common in certain groups of patients. Particularly, those who are hospitalized, seriously ill, or elderly are more likely to have this condition. In fact, one report found that over 70% of elderly patients who are hospitalized have this condition.
Signs and Symptoms of Hypoalbuminemia
Hypoalbuminemia is a condition often discovered during routine medical tests conducted for other primary health issues. It’s marked by lower albumin protein levels in the blood.
Those with hypoalbuminemia may experience certain symptoms such as:
- Swelling in the extremities (peripheral edema)
- Accumulation of fluid in the abdomen (ascites) and other cavities in the body (effusions)
- General swelling of the body (anasarca)
- Fatigue and excessive weakness
- Symptoms relating to nutritional deficiencies, such as iron deficiency anemia, often seen in people with Celiac disease
Signs of the underlying disease that causes hypoalbuminemia may also be present. For instance, a person with liver disease may show indications like jaundice, while someone with protein-losing enteropathy (PLE) might have symptoms like diarrhea. When a urine test strip is used, high protein levels in the urine (proteinuria) may be detected.
Testing for Hypoalbuminemia
A quick and accessible way to identify if you have low albumin levels in your body involves measuring serum albumin using automated chemistry analyzers. These machines monitor the change in color when albumin binds to a specific dye; the color alterations are measured with a technique called spectrophotometry. Alternatively, other techniques, known as immunonephelometry or immunoturbidometry, can also be used.
Your doctor might also find low albumin levels while undertaking protein electrophoresis, a test that provides an approximate albumin value. This test can be useful if you have low albumin levels as it helps determine the reason behind it. During an acute inflammatory response, if you have lower albumin levels, there will also be an increase in types of proteins called alpha-1 and 2 globulins, while the gamma globulins remain standard. In chronic inflammation, the test pattern will show low albumin levels along with an increase in gamma globulins.
If you’re suffering from nephrotic syndrome, a kidney disorder, the test will reveal low albumin levels with an increase in alpha-2 globulins due to the presence of large proteins, and a decrease in gamma globulins.
With chronic liver disease, tests will typically show low albumin levels with an increase in gamma globulins and something called beta-gamma bridging.
To understand the cause of low albumin levels and to monitor the condition, some other tests might be conducted. These include liver function tests to check for liver disease, measurements of albumin in urine to analyze protein loss, and tests for a heart-related protein called brain natriuretic peptide. Imaging scans might also be conducted.
A particular test you may undergo as part of the evaluation involves measuring alpha-1 antitrypsin clearance to evaluate protein loss in the area of your gut beyond the stomach. This test necessitates collecting a stool sample over a defined period and a blood sample. A protein called alpha-1-antitrypsin, which can’t be broken down by digestive enzymes, serves as a marker for blood proteins in the gut. If this protein is excreted in excess, it suggests an abnormal protein loss from your gastrointestinal system.
Treatment Options for Hypoalbuminemia
The treatment for hypoalbuminemia, which is a low level of albumin protein in the blood, depends on what’s causing it. This is because hypoalbuminemia is usually a result of another health condition. For example, albumin infusions, which are treatments that put albumin directly into your bloodstream, may be given to people who have been severely burned or are very ill.
Whether albumin infusions help other groups of critically ill patients is a topic of debate among healthcare professionals. These infusions can also be useful for people with cirrhosis, a type of liver disease, who are experiencing certain complications.
What else can Hypoalbuminemia be?
When it comes to determining the causes of low levels of albumin in the blood, or hypoalbuminemia, the possibilities are numerous. These include:
- Diseases impacting the production of albumin, such as cirrhosis,
- Issues affecting the absorption of albumin and protein, as seen in certain conditions like Protein Losing Enteropathy (PLE),
- Conditions that result in the loss of albumin through the kidneys, like nephrotic syndrome,
- And situations where the body breaks down substances quickly, a process known as increased catabolism. This is typically seen in severely ill patients.
What to expect with Hypoalbuminemia
Low levels of albumin, a protein in your blood, can often serve as an early warning sign for health complications, especially in patients admitted to the hospital or those in critical care. Doctors often use this condition, called hypoalbuminemia, to predict the likelihood of serious health outcomes for these patients.
Possible Complications When Diagnosed with Hypoalbuminemia
Serious complications can occur with severe hypoalbuminemia, a condition where there’s a low level of albumin in your blood. These complications can include circulatory collapse (when your blood ceases to circulate around your body properly) due to its impact on the pressure required to keep fluid in the blood vessels (what’s known as oncotic pressure). Other potential complications are swelling (edema) and extreme, generalized body swelling (anasarca). All of these complications can also increase the risk of other problems in individuals who are critically ill.
Complications:
- Circulatory collapse due to impact on oncotic pressure
- Presence of edema (swelling)
- Anasarca (extreme, generalized body swelling)
- Increased risk for additional complications in critically ill patients