What is Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)?
Hypothyroid myopathy is a condition that’s seen in between 30% and 80% of people with hypothyroidism. This condition can appear in both congenital (from birth) and acquired (developed later in life) cases. It shows up as generalized muscle aches, weakness, and pain or stiffness. The thyroid hormone is fundamental for metabolism, growth, and the function of organs, impacting the musculoskeletal system, which involves our muscles and skeleton. Severe or untreated hypothyroidism can lead to serious muscle disease, causing major functional limitations.
The symptoms of hypothyroid myopathy can come on slowly and be nonspecific, meaning it’s hard for medical professionals to tell it apart from fatigue and other similar muscle disorders. It’s important for every patient diagnosed with hypothyroidism to be asked about any muscle or skeleton-related symptoms. The muscles most affected are usually the proximal ones found in the thighs, hips, shoulders, and neck. This can affect daily activities such as climbing stairs, getting up from a seated position, and lifting items. In rare cases, severe hypothyroid myopathy can result in muscle tissue death, a condition known as acute compartment syndrome, or even respiratory failure.
What Causes Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)?
Hypothyroid myopathy happens when the thyroid gland doesn’t produce enough hormones. These hormones are vital for our body’s metabolism, which includes how our muscles function. When these hormone levels are low, it can lead to symptoms like muscle weakness and fatigue. Here are some common reasons behind this hormone deficiency:
* Autoimmune disorders: The most common cause in developed countries is Hashimoto thyroiditis, an autoimmune disorder where the body’s immune system attacks the thyroid gland, leading to hypothyroidism.
* Iodine deficiency: Iodine is a nutrient necessary for making thyroid hormones. If there isn’t enough iodine in a person’s diet, it can result in a deficiency of thyroid hormones and eventually hypothyroid myopathy. This is the most common cause worldwide.
* Thyroid surgery or radiation therapy: If a person has to undergo surgery or radiation on their thyroid gland, it can harm the gland or lessen its function, causing hypothyroidism and hypothyroid myopathy.
* Medications: Some prescribed drugs, like lithium, can affect the production of thyroid hormones.
* Congenital hypothyroidism: Some people are born with an underactive thyroid gland, which can lead to noticeable developmental delays and physical deficiencies.
* Aging: As we get older, our thyroid function may naturally decline.
In nutshell, hypothyroid myopathy happens when there’s not enough thyroid hormones in the body, and this can be caused by numerous factors, including autoimmune disorders, iodine deficiency, surgery, certain medications, congenital hypothyroidism, and aging.
Risk Factors and Frequency for Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
Hypothyroidism is a common medical condition, with as many as 12% of Americans likely to experience it at some point in their lives. It can occur at any age, though it typically shows up most often between the ages of 40 and 70. While it affects both genders, women tend to have it more often than men. No specific ethnic or racial group is more prone to it than others. Lastly, it appears to affect older adults more frequently than younger folks.
- Hypothyroidism is a typical health issue.
- About 12% of Americans may experience it at some point.
- Though it can happen at any age, it’s most common between 40 and 70 years.
- Women are more likely to have this condition than men.
- It doesn’t affect any race or ethnic group more than others.
- Older adults have a higher chance of getting it versus younger individuals.
Signs and Symptoms of Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
Hypothyroidism, an underactive thyroid condition, can sometimes lead to changes in the muscles and nerves, along with common symptoms like fatigue, weight gain, intolerance to cold, and dry skin. You might even notice a decrease or absence of deep tendon reflexes. In rare cases, muscle and nerve issues could be the first sign of hypothyroidism, so if you experience new muscle or nerve problems, it’s important to consider the possibility of thyroid dysfunction.
When hypothyroidism impacts the muscles (a condition called hypothyroid myopathy), you might experience different symptoms. These can include muscle pains, cramping, fatigue, and weakness, especially after exertion. You might notice muscle stiffness or general body pain which increases after exercise. These symptoms could happen together with higher levels of muscle enzymes in the blood.
- Myalgia: This presents as muscle stiffness or widespread pain, often worse after exercise.
- Proximal Myopathy: This is recognized by slow and symmetrical muscle weakness, fundamentally in the shoulders and hip areas. Sometimes, this condition could be severe, involving high levels of muscle enzymes in the blood.
- Muscle Pseudohypertrophy: This can lead to muscle enlargement and different degrees of weakness. It can give the skin and underlying tissue a thick and doughy appearance. The signs of hypothyroidism are typically obvious in these circumstances.
There are also two syndromes connected to muscle pseudohypertrophy:
- Kocher-Debre-Semelaigne Syndrome: It usually affects children and is associated with muscle enlargement, skin swelling, short height, and developmental delays.
- Hoffmann Syndrome: Generally seen in adults, this is characterized by pseudohypertrophy, painful spasms, muscle weakness, and stiffness. Usually, it is seen in primary hypothyroidism but very rarely in secondary hypothyroidism. It’s thought to be caused by the deposit of certain molecules and the increase in muscle fiber size.
Rhabdomyolysis is a possible complication of hypothyroidism that can cause exceedingly high levels of an enzyme called creatine kinase. It can be triggered by intense exercise, trauma, electrolyte imbalance, alcohol consumption, or concurrent statin therapy, and may lead to kidney failure.
Myoedema refers to a small bump that appears on the muscle surface after light pressure, such as that from a percussion hammer. This bump lingers for a while due to sustained muscle contraction and the slow return of calcium to muscle cells.
Acute compartment syndrome, a condition where increased pressure within a muscle hampers blood supply, is a rare complication of hypothyroidism. It can be caused by heavy exercise, statin or alcohol use, although the specific mechanisms are unclear.
Testing for Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
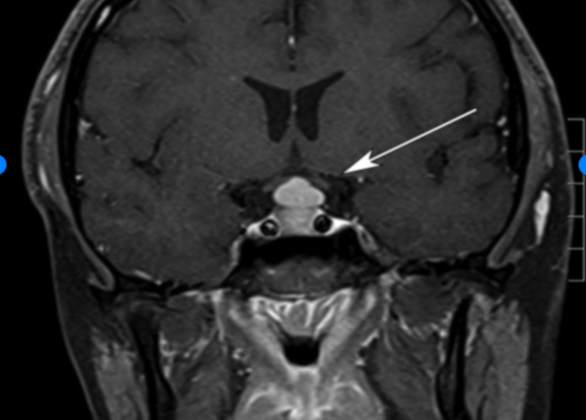
If you’re being tested for hypothyroid myopathy, a condition which involves muscle weakness due to underactive thyroid, doctors will check your levels of two things in your blood: thyroid-stimulating hormone (TSH) and T4. It’s common to find higher than normal levels of an enzyme called creatine kinase in people with this condition. However, this isn’t unique to hypothyroid myopathy, and you might have high creatine kinase levels for many years before you start noticing muscle issues.
To figure out how weak your muscles might be, you may be asked to do some physical tests. These could include walking for six minutes, measuring your hand grip strength, or seeing how quickly you can stand up from a chair. These tests help doctors understand more about the strength in your proximal muscles, which are the ones closest to the center of your body.
Another test that may be done is an electromyography (EMG), which measures the electrical activity in your muscles. In some people with hypothyroid myopathy, this test may show lower than normal activity. However, half of the people with this condition have a normal EMG, so having normal results doesn’t necessarily mean you don’t have hypothyroid myopathy. If you have another condition called Hoffman syndrome, the EMG could also show unusual wave patterns.
Doctors don’t always need to do a muscle biopsy to diagnose hypothyroid myopathy, but if they do, they might find certain features in the muscle tissue. These might include swelling and paleness in the tissue, loss of the usual muscle pattern, and wider gaps between muscle fibers. Other characteristics can include changes in muscle fiber sizes, areas of muscle cell death or damage, and unusual features like more internal nuclei, unusual inclusions within the mitochondria, glycogen build-up, vacuoles that look like they are involved in autophagy, and disorganized myofibrils.
Treatment Options for Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
Levothyroxine, a synthetic version of the thyroid hormone thyroxine (T4), is the main medicine used to treat hypothyroidism, including muscle problems caused by this condition. The body absorbs levothyroxine slowly and circulates rapidly. However, it may take around 6 weeks to fully see its effects. Dosage adjustments are guided by monitoring the levels of thyroxine and thyroid-stimulating hormone (TSH) in the blood. The goal is to normalize these levels in about two months. Improvement in muscle problems often begins within 2 to 3 weeks, but it may take several months for complete resolution.
The starting dose of levothyroxine is usually 1.6 micrograms per kilogram of body weight every day. However, this might be lower for older patients or those with heart disease. Levothyroxine should be taken on an empty stomach with water, ideally 30 to 60 minutes before eating. If there are still symptoms after 2 to 3 weeks, the patient’s condition should be reassessed, and their blood levels of thyroxine and TSH rechecked after 3 weeks. The maintenance dose may differ depending on the cause of hypothyroidism. Doctors usually check TSH levels every year or more often if the results are abnormal or the patient’s status changes.
One study suggested that the amount of T4 needed relates more to lean body mass than total body weight. It also found that the full replacement dose after thyroid removal varied based on the patient’s body mass index (BMI)—with varying doses according to different BMI categories.
Before starting hormone replacement therapy, it’s important to rule out adrenal insufficiency to prevent a potentially life-threatening condition called adrenal crisis. After thyroid hormone replacement and restoring normal thyroid function, most patients gradually see their neuromuscular symptoms resolve. Creatine kinase levels, a marker for muscle damage, typically drop quickly within a few weeks of starting thyroxine replacement, often before TSH levels normalize. This could be used as an early indicator of treatment response, as it may take up to 6 months for the muscle symptoms to completely resolve. Most symptoms resolve within a year of adequate hormone replacement.
What else can Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid) be?
When doctors are trying to diagnose muscle weakness caused by an underactive thyroid, also known as hypothyroid myopathy, they need to also consider that it could be due to other conditions, such as:
- A disorder called acid maltase deficiency, which affects muscle cells
- Acute poliomyelitis, a viral disease that can cause paralysis
- Amyotrophic lateral sclerosis, also known as ALS or Lou Gehrig’s disease, which is a neurodegenerative disease that affects nerve cells in the brain and spinal cord
- Becker muscular dystrophy, a genetic disorder that causes progressive muscle weakness
- Inclusion body myositis, a type of inflammation of the muscles
- Polymyositis, an inflammatory disease that causes muscle weakness
- Post-polio syndrome, which can cause a variety of symptoms in people who have had polio earlier in life
- Peripheral neuropathy, a result of damage to your peripheral nerves, often causes weakness, numbness and pain, usually in your hands and feet
It’s important to rule out these possibilities in order to make an accurate diagnosis and provide the best possible treatment.
What to expect with Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
In general, people with hypothyroid myopathy – a muscle disease caused by an underactive thyroid – can expect a good outcome if the condition is recognized and treated promptly. In many cases, muscle strength and function can improve significantly with thyroid hormone replacement therapy. But, please remember it’s not a quick fix; recovery might take a while, and ongoing treatment over a long period might be necessary.
On the other hand, more severe cases could have a less favorable prognosis, especially when the diagnosis comes late or the patient has other health problems. In these situations, there might be permanent muscle damage, resulting in the loss of muscle strength and function. So, quick identification and treatment are important to prevent this.
Possible Complications When Diagnosed with Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
Hypothyroid myopathy is a condition that can progress and lead to several symptoms and issues. Below are some possible complications:
- Muscle cramps: This condition can cause your muscles to experience prolonged contractions, leading to cramps. This generally happens in muscles that are already weak.
- Reduced mobility: The muscle weakness and fatigue linked with hypothyroid myopathy can make it more difficult to move. Regular tasks like walking, climbing stairs, or standing up from a chair might become challenging.
- Increased risk of falls: The decreased mobility may also lead to a higher chance of falling. This risk is especially serious for older adults, as falls can result in injuries like fractures, further limiting mobility and lowering quality of life.
- Respiratory complications: Severe cases of hypothyroid myopathy can cause the muscles used for breathing to weaken. This can result in respiratory issues like shortness of breath and difficulty breathing.
- Cardiovascular complications: This condition might also affect the heart muscles, increasing the risk of heart failure and irregular heart rhythms (arrhythmias).
- Psychological impact: Living with ongoing muscle weakness and fatigue from hypothyroid myopathy can lead to psychological effects. These can include depression, anxiety, and lower self-esteem.
- Long-term disability: When hypothyroid myopathy is severe, persistent muscle weakness and functional impairment may lead to long-term disability. This could mean needing ongoing help with daily activities.
Recovery from Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
Rehabilitation for hypothyroid myopathy, a condition that weakens the muscles, aims to build up muscle strength, stamina, and overall functionality. Although there isn’t a designated rehab program for this condition, general rehab methods can be used to deal with muscle weakness and related symptoms. The key parts of rehabilitation for hypothyroid myopathy include:
A physical therapy assessment: A physical therapist will evaluate things like the patient’s muscle strength, range of motion, balance, and daily functional abilities. By identifying weak spots or problems, the therapist can design a personalized treatment plan to address these issues.
Exercise therapy: Exercise is crucial for rehabilitation and a properly structured program can enhance muscle strength, endurance, and movement. This could include strength-building exercises, aerobics, flexibility and balance training. The workout regimen would be tailored over time to fit the patient’s needs.
Conserving energy: Tiredness is a usual symptom of hypothyroidism, so learning how to conserve energy and manage daily activities more efficiently can be beneficial. Some energy-saving techniques include pacing one’s activities, task prioritization, and using special equipment or support devices to lessen physical strain.
Walking training: People with hypothyroid myopathy often have difficulty walking. Gait training exercises help to improve walk patterns, balance, and coordination. These exercises can include specific tasks, such as heal-to-toe walking, side-stepping, and climbing stairs.
Functional training: The patient’s ability to perform daily life tasks like grooming, dressing, household chores should be the focus of rehabilitation. Exercises mirroring real-life activities can help patients regain confidence and independence in their daily routines.
Education and self-management: Educating patients about hypothyroidism and its effect on muscle function, the significance of sticking to their medication and lifestyle changes is crucial. Empowering patients to take charge of their condition and maintain their rehabilitation progress is important.
Collaboration with others: The rehab care for hypothyroid myopathy may require working together with other health practitioners such as endocrinologists, neurologists, and occupational therapists. This team approach ensures that we cater to all the patient’s needs.
In a nutshell, rehab care for hypothyroid myopathy should be personally customized to match the patient’s needs and goals, aiming to improve muscle function, boost functionality, and enhance their overall quality of life. A comprehensive and multidisciplinary approach is key to achieving the best results for patients with hypothyroid myopathy.
Preventing Hypothyroid Myopathy (Muscle Weakness due to Hypothyroid)
Patients should be told to quickly let their healthcare provider know if they start to experience or have worsening muscle weakness, cramping, or muscle pains. These might be signs of a condition called hypothyroid myopathy. Regular check-ups are extremely important for assessing changes in thyroid function and making necessary adjustments to the medication dosage as required.