What is Lymphocytic Hypophysitis?
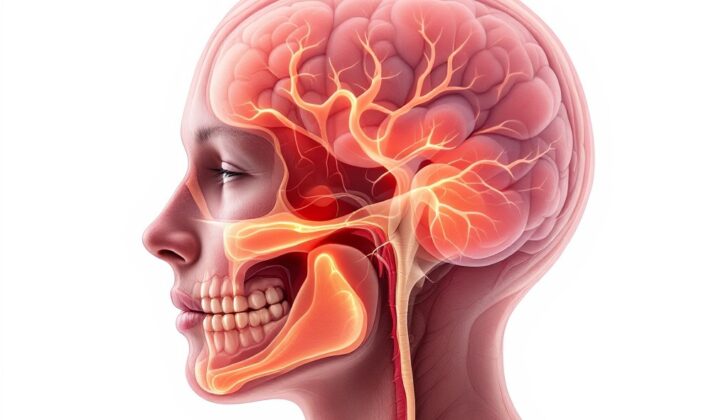
Lymphocytic hypophysitis is a rare condition affecting the pituitary gland, a small, pea-sized organ situated at the base of your brain. This condition results from inflammation and/or a growth within the gland, leading to decreased functionality, a situation we refer to as hypopituitarism. This happens because the gland gets invaded by T and B lymphocytes, types of cells from your immune system.
This issue is an autoimmune condition, meaning your own immune system mistakenly attacks your body’s own cells and tissues. Out of all types of primary hypophysitis, where the inflammation starts in the pituitary itself, lymphocytic hypophysitis is encountered most frequently when examining tissue under a microscope.
Symptoms of this condition are caused by the pituitary gland not functioning properly. These may include central diabetes insipidus, a condition characterized by extreme thirst and excessive urination; A deficiency in hormones produced by the front part of the pituitary gland; and high levels of a hormone called prolactin, which we call hyperprolactinemia.
Because this condition is relatively rare, correctly identifying and treating it can be tricky. Nevertheless, understanding its symptoms and causes is an important step towards improved patient care.
What Causes Lymphocytic Hypophysitis?
Hypophysitis is a condition caused by inflammation in the pituitary gland.
It can be grouped into two categories based on its origin: primary or secondary.
- Primary hypophysitis happens inside the pituitary gland directly. Primary hypophysitis can be further divided based on the type of cells affected and area of the pituitary gland involved. The types of primary hypophysitis include lymphocytic, granulomatous, xanthomatous, IgG4 related, or mixed. Primary hypophysitis can also be categorized based on which part of the gland is affected.
- Secondary hypophysitis arises from other conditions or medications that cause inflammation in the pituitary gland. Conditions that can cause secondary hypophysitis include sarcoidosis, hemochromatosis, amyloidosis, granulomatosis with polyangiitis, tuberculosis, syphilis, and certain immune system modulating medicines. Lymphocytic hypophysitis is a type of primary hypophysitis and is the most common form. Lymphocytic hypophysitis is sometimes referred to as autoimmune hypophysitis.
Risk Factors and Frequency for Lymphocytic Hypophysitis
Hypophysitis, which refers to inflammation of the pituitary gland, is pretty rare. Each year, it only affects about 1 in 9 million people. That said, these numbers could be an underestimation, since certain treatments for cancer that can impact the pituitary gland have become more widely used recently. Additionally, there’s a type of hypophysitis linked to the immune system (known as IgG4 related disease) that’s only recently been recognized.
One specific type of hypophysitis, lymphocytic hypophysitis, was initially thought to only affect pregnant women in their last trimester or during the first six months after giving birth. However, we now know that it can also occur in women who aren’t pregnant and in men. This condition is still rare though, and it affects women eight times more frequently than men.
The average age of diagnosis is around 44.7 for men and 34 for women. In 20% to 50% of cases, it’s associated with other conditions that involve the body’s immune system attacking its own cells.
Signs and Symptoms of Lymphocytic Hypophysitis
Lymphocytic hypophysitis, which originally was believed to only impact the front portion of the pituitary gland, can also affect the rear part of the gland and the connecting stalk. This leads to inflammation, and the infiltration of certain immune cells into the gland. The disease can result in deficiencies in one or more pituitary hormones. If it affects the posterior part, it can cause central diabetes insipidus, and if the anterior part is affected, it can lead to conditions like central adrenal insufficiency and hypothyroidism.
Moreover, conditions like hypogonadotropic hypogonadism and growth hormone deficiency can also occur due to the inflammation of the pituitary gland. If the pituitary gland increases in size, it can press against the optic apparatus/chiasm, resulting in decreased vision and color perception.
Most people with this disease initially experience headaches, which then may lead to visual field defects, double vision, and a condition called ophthalmoplegia. Sequentially, destruction of the pituitary can occur, leading to hypopituitarism, which affects almost all pituitary hormones. Common symptoms of this include:
- Nausea
- Vomiting
- Fatigue
- Loss of sexual desire
- Failure of menstruation (amenorrhea)
- Dizziness
Testing for Lymphocytic Hypophysitis
People with lymphocytic hypophysitis, a condition marked by inflammation of the pituitary gland, often present with symptoms related to impaired pituitary gland function. The only surefire way to diagnose this condition is by examining tissue samples under a microscope. However, with a combination of clinical evaluation, lab testing, and imaging studies, doctors can often make an accurate diagnosis without needing to resort to a tissue biopsy.
To diagnose on the basis of symptoms alone, doctors will often assess your pituitary hormone function. They will measure levels of several hormones, including prolactin, adrenocorticotropic hormone, cortisol, IGF-1, growth hormone, thyroid-stimulating hormone, free thyroxine, testosterone, luteinizing hormone, and follicle-stimulating hormone. They will also check whether you have developed diabetes insipidus, a condition that causes excessive thirst and urination, among other symptoms. This involves testing for electrolyte levels, anti-diuretic hormone, serum and urine osmolality, and may require a water deprivation test if needed.
In addition, up to 50% of people with lymphocytic hypophysitis will also have other autoimmune conditions. Doctors will often check for antibodies associated with your pituitary gland (antipituitary antibodies) and hypothalamus (antihypothalamus antibodies), and may run tests to check for other autoimmune and inflammatory diseases. These can include a complete blood count, a complete metabolic panel, c-reactive protein, erythrocyte sedimentation rate, antinuclear antibody, and lupus antibodies at the very least.
Imaging studies, such as MRI scans of your pituitary gland, also play an important role in diagnosing lymphocytic hypophysitis. It’s important to differentiate this condition from a pituitary adenoma, a noncancerous tumor. In lymphocytic hypophysitis, the pituitary gland and the pituitary stalk is symmetrically enlarged, but there is no stalk deviation. The MRI scan may also show a homogeneously intense pituitary with dura enhancement (dural tail), along with arachnoid (a membrane covering the brain and spinal cord) enhancement. These features are not present in a pituitary adenoma.
However, it can still be difficult to distinguish between lymphocytic hypophysitis and a pituitary adenoma based on imaging alone. This can lead to misdiagnoses, and even unnecessary surgeries. To help with this issue, a scoring system known as the Gutenberg scoring was developed to identify lymphocytic hypophysitis more accurately.
The exact scores for this system are rather complex and specific, but they take into account factors such as a patient’s age, current or recent pregnancy, MRI findings such as increased stalk size and specific patterns of pituitary gland enhancement, and other signs and symptoms. A total score above 1 suggests a pituitary adenoma, while a score of 0 or below suggests lymphocytic hypophysitis. This scoring system has been proven to have a high degree of success in correctly diagnosing lymphocytic hypophysitis.
Treatment Options for Lymphocytic Hypophysitis
The treatment of a condition called lymphocytic hypophysitis revolves around managing hormone deficiencies caused by the pituitary gland (a tiny organ at the base of your brain that controls hormone production) and treating any enlargement of the pituitary gland which may cause other issues. Treatment usually includes careful monitoring and the use of anti-inflammatory medicine, with surgery or radiation therapy being rarely needed.
Firstly, doctors need to assess the function of the pituitary gland and manage any deficiencies in the hormones it produces. Patients should also be checked for a condition called diabetes insipidus, (a rare form of diabetes that causes excessive thirst and urination), which may require treatment. While lymphocytic hypophysitis can sometimes get better on its own, steroid therapy is typically the main treatment if this condition is suspected. Steroids are medicines that reduce swelling and inflammation, and can lessen the effect of the gland’s enlargement.
But if a person’s sight is impaired or other important structures are being compressed due to the enlarging gland, surgery might be necessary. Surgery can also be required if a biopsy (a small sample of tissue) is needed to confirm the diagnosis. Some patients may need long-term therapy with hormone replacements. However, steroidal therapy can help patients recover their pituitary function and reduce the need for lifelong hormone replacements if the condition doesn’t reoccur after treatment.
The dosage and duration of steroid therapy can vary, as there is no consensus on what is best. One study in Germany treated patients with varying doses of steroid medications over durations ranging from four days to a year. Steroids need to be reduced gradually depending on the patient’s response, as long term use has been shown to increase the risk of side effects like weight gain, a condition known as Cushing’s Syndrome (which causes weight gain, especially in the face and upper body), swelling, glaucoma (a group of eye conditions that damage the optic nerve), psychiatric symptoms, and diabetes.
While initial response to steroid therapy can be good, there is a high chance, about 38%, that the condition might reoccur. If steroids don’t help or the condition reoccurs after steroid treatment, other medications to suppress the immune system, such as methotrexate, azathioprine, and cyclosporine can be used. Some cases have also successfully been treated with dopamine agonists, a type of drug that affects the levels of a chemical in the brain which promotes the production of a hormone called prolactin, due to inflammation of the pituitary gland.
Surgery is only considered for those who suffer from vision problems, have a mass effect from gland enlargement that is causing compression on nearby structures, or for those needing a biopsy for diagnosis. Surgery may be appealing because it provides a tissue sample to confirm lymphocytic hypophysitis and eliminate the possibility of a pituitary tumor. However, surgery, which can involve partial removal of the pituitary lesion or decompression of the mass, has a chance of the lesion and symptoms coming back in 11% to 25% of patients. No relationship has been found between the extent of resection and the recurrence rate. Surgical complications can include postoperative meningitis (inflammation of membranes that cover the brain and spinal cord) and rhinorrhea (continuous discharge of fluid from the nose). There have been cases where steroid therapy and surgery were both used.
If all mentioned approaches, including immunosuppressive therapy, fail to work, a type of radiation therapy called fractionated radiotherapy can be used.
What else can Lymphocytic Hypophysitis be?
When physicians try to diagnose lymphocytic hypophysitis, which involves inflammation of the pituitary gland, they start with a detailed history and physical examination of the patient. However, without a sample of tissue obtained through a biopsy and seeing evidence of a mass in the pituitary gland alongside symptoms of hypopituitarism (a condition where the pituitary gland does not produce enough hormones), it can be difficult to narrow down the diagnosis.
The potential causes for these symptoms are broad. Primarily, the doctor might consider the possibility of a pituitary adenoma, which is a benign tumor of the gland. However, other conditions may also cause these symptoms, including:
- A craniopharyngioma, which is a rare type of brain tumor.
- A Rathke cleft cyst, a benign cyst in the brain.
- Germinomas, a type of germ cell tumor.
- Pituitary apoplexy, a medical emergency caused by bleeding into or impaired blood supply of the pituitary gland.
- Pituitary metastasis, a condition where cancer elsewhere in the body has spread to the pituitary gland.
Additionally, some infectious and inflammatory conditions may result in the same symptoms. These include:
- IgG4 hypophysitis, an autoimmune disease affecting the pituitary gland.
- Granulomatous hypophysitis, which could be due to tuberculosis, syphilis, or sarcoidosis.
- Wegner’s granulomatosis, a rare disease causing inflammation of blood vessels.
- Langerhans cell histiocytosis, a rare type of cancer affecting the brain.
With these potential diagnoses in mind, the next step is to carry out a thorough lab work and imaging for further investigation.
What to expect with Lymphocytic Hypophysitis
Lymphocytic hypophysitis, a disease of the pituitary gland, often gets misdiagnosed as it can share similar symptoms with another condition called pituitary adenoma. In the past, this disease could only be diagnosed after a patient’s death, but with modern imaging technology, we’re able to detect it sooner and have seen an increase in reported cases.
The pituitary gland is affected by an excessive number of lymphocytes (a type of white blood cell), which causes inflammation. This inflammation can lead to a condition called hypopituitarism, where the pituitary gland doesn’t produce necessary hormones.
Treatment depends on the severity of the patient’s symptoms. Some cases might resolve on their own over time and only require regular check-ups. Other treatment options include glucocorticoid therapy, immunosuppressive agents, or even partial removal of the pituitary gland by surgery. If there’s a risk to vital structures nearby, surgical decompression might be necessary.
Diagnosing lymphocytic hypophysitis can be challenging because many patients don’t show any symptoms. However, most patients will experience headaches, vision problems, or other hormone-related symptoms. Diagnosis can often occur long after the initial symptoms appear.
In many cases, despite medical and surgical treatment, a recurrence of the disease may occur, requiring lifelong hormone replacement therapy. Diagnosing and managing such conditions, especially adrenal insufficiency (a condition where the adrenal glands don’t produce enough essential hormones), is vital as it can result in serious health complications and even be life threatening.
However, even though diagnosing lymphocytic hypophysitis can be difficult, once it’s detected, it can be effectively managed with steroids, surgery, immunosuppressive agents, and regular monitoring. Most patients will have a good prognosis with appropriate treatment.
Possible Complications When Diagnosed with Lymphocytic Hypophysitis
It’s crucial to quickly diagnose and properly treat a condition called lymphocytic hypophysitis as it can lead to complications. Often patients with this condition experience issues with their pituitary gland hormones, leading to conditions like diabetes insipidus and overall hormone deficiency – known as panhypopituitarism. It also impacts levels of prolactin, a hormone that can be either too low, normal or too high. Key hormones to check for abnormal levels are cortisol and adrenocorticotropic hormone, as these are indicators of a condition called adrenal insufficiency that can come from lymphocytic hypophysitis.
Detection of secondary adrenal insufficiency can be a bit tricky due to its rapid development. One common test may not show abnormal results in time because the adrenal glands haven’t had time to weaken. To early detect adrenal insufficiency, another test involving insulin-induced low blood sugar might be necessary.
Other hormone imbalances may potentially occur, and they can be tested for. This includes hormones and factors like prolactin, IGF-1, growth hormone, thyroid-stimulating hormone, free thyroxine, testosterone, luteinizing hormone, follicle-stimulating hormone, electrolytes, anti-diuretic hormone, and serum and urine osmolality.
Additionally, if the pituitary gland enlarges, it can cause neurological issues, like visual field defects due to its growing size pressing on surrounding structures. This could result in pressure on the optic nerve, optic chiasm and cranial nerves located in the cavernous sinus. Symptoms could include poor color vision, eye muscle paralysis, and double vision.
Possible Health Checks:
- Adrenocorticotropic hormone and cortisol level tests.
- Insulin-induced hypoglycemia test for adrenal insufficiency.
- Hormonal tests for: prolactin, IGF-1, growth hormone, thyroid-stimulating hormone, free thyroxine, testosterone, luteinizing hormone, follicle-stimulating hormone.
- Tests to check the levels of: electrolytes, anti-diuretic hormone, serum and urine osmolality.
- Check for neurological symptoms related to pituitary gland enlargement.
Preventing Lymphocytic Hypophysitis
Lymphocytic hypophysitis is a rare health problem where your body’s immune system mistakenly attacks your pituitary gland (a small organ at the base of the brain that controls many important functions in your body). Due to this, the gland becomes inflamed. This condition is seen more in women than in men. On average, men are diagnosed around 45 years old, while women are around 34.
Typical symptoms include headaches, issues with vision, feeling sick, throwing up, feeling dizzy, extreme tiredness, a reduced sex drive, and women might stop menstruating. If you experience any of these symptoms, it is essential to let your doctor know. In most cases, the doctor might suggest getting blood tests and an MRI scan of your brain to diagnose the condition. The treatment can vary from person to person. Some may require supportive care, the use of steroids, medicines that reduce the body’s immune response, and sometimes even surgery. If you’re having serious vision problems, surgery might be necessary.
It’s very important to have regular check-ups with all your doctors, especially for the long-term monitoring of your condition. This is particularly important for keeping an eye on any hormone deficiencies and giving you hormone therapy if required. If detected early and managed appropriately, people diagnosed with lymphocytic hypophysitis generally have a good recovery.