What is Mediastinitis?
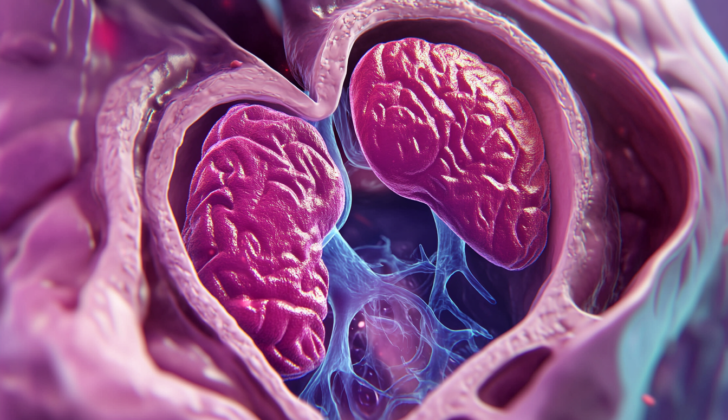
Mediastinitis is a serious and potentially dangerous condition where there’s inflammation or an infection in the mediastinum. The mediastinum is the area inside your chest that’s enclosed by your lungs and contains important parts of your body like your heart, major blood vessels, windpipe, main airways, food pipe, and several nerves. This condition is rare but it should be taken into account because any infection in these critical organs is life-threatening and needs immediate medical attention.
Mediastinitis can occur due to various reasons and is mainly divided into three types—postoperative mediastinitis, descending necrotizing mediastinitis, and fibrosing mediastinitis. Postoperative mediastinitis is the most common type and happens after a surgery. Descending necrotizing mediastinitis is the next common type and these two usually happen suddenly and progress rapidly. Fibrosing mediastinitis, the rarest subtype, develops slowly over time.
What Causes Mediastinitis?
Mediastinitis is a condition caused by damage to structures located in the space between your lungs, known as the mediastinum. This damage can be caused by medical procedures, traumatic events, or infections. For example, complications from medical procedures like heart surgery, esophageal dilation, or endoscopic interventions may cause accidental injury to tissues in this area, leading to infection, which we call “iatrogenic” causes. Trauma-mediated causes could be chest injuries from accidents or wounds that harm the windpipe (trachea) or esophagus, causing contamination in the mediastinum. Infections can spread to the mediastinum from nearby areas, as seen in conditions like descending necrotizing mediastinitis, where infections from the mouth or throat extend into the mediastinum. Infections can even sometimes spread from elsewhere, such as lung infections or complications from pancreatitis.
In cases where there’s a tear in the esophagus, mediastinitis can occur. This happens because the rupture allows stomach fluid, containing digestive bacteria, to leak into the mediastinum. These tears can be due to medical procedures, although they can also occur spontaneously or due to injury. Some common causes are from endoscopic procedures, Boerhaave syndrome (a rare condition where there’s a spontaneous tear in the esophagus), and foreign body aspiration (inhaling a foreign object). Other, less common causes include, direct injury, spread of lung infection, and pancreatitis.
Poststernotomy mediastinitis is a rare condition that can occur after chest surgery. Even with advancements in surgical techniques and antibiotics, along with guidelines to prevent infections, there has been no significant decrease in the occurrence of this condition. The infection generally occurs at the time of surgery or afterwards, from the surgical wound.
A specific type of mediastinitis, known as descending necrotizing mediastinitis, arises from mouth or throat infections that spread downward from the neck to the mediastinum. This condition occurs in about 2% to 5% of cases where a deep abscess (pocket of pus) forms in the neck, as seen in conditions like Ludwig’s Angina, and other dental infections.
An uncommon type of mediastinitis, known as fibrosing mediastinitis, doesn’t have an identified cause but is believed to be associated with a number of infectious and noninfectious processes. Potential infectious causes include histoplasmosis and tuberculosis, which are linked to an immune-system reaction. Noninfectious causes might include diseases such as sarcoidosis (an inflammatory disease that can affect any organ), retroperitoneal fibrosis (inflammation in the abdominal region), and Riedel thyroiditis (a rare inflammatory disease affecting the thyroid).
Risk Factors and Frequency for Mediastinitis
The exact number of people who suffer from mediastinitis is not well known. Most clinics and hospitals see mediastinitis in about 0.3% to 5% of their patients after surgery, with an average of 1% to 2%. The rate is higher in patients who have had heart transplant surgeries, surgeries to bypass blocked arteries in the heart along with thoracic aortic surgery, and surgeries to bypass blocked arteries in the heart along with heart valve surgeries. However, the rate is lower in patients who have had only artery bypass surgeries, heart valve repairs, and thoracic repairs.
- Mediastinitis is seen in about 0.3% to 5% of patients after surgery. The average is 1% to 2%.
- Heart transplant, coronary artery bypass with thoracic aortic surgery, and coronary artery bypass with valve surgery patients have higher rates of mediastinitis.
- Isolated coronary artery bypass, valve repairs, and thoracic repairs patients have lower rates.
In the past, most mediastinitis cases were of the descending necrotizing mediastinitis type. But with advancements in medical imaging and antibiotics, this rate has significantly decreased. For fibrosing mediastinitis, it is often associated with a subtype known as granulomatous, which is more commonly found in North America due to a higher rate of Histoplasma capsulatum, a type of fungus.
- Descending necrotizing mediastinitis cases have significantly decreased thanks to medical advancements.
- Fibrosing mediastinitis is often linked to a subtype called granulomatous, common in North America.
Signs and Symptoms of Mediastinitis
Acute mediastinitis is a serious condition that can make patients look and feel unwell. Common symptoms include difficulty swallowing, chest pain, fever, and shortness of breath. For doctors, understanding a patient’s overall health, recent surgeries or infections, travel history, and lifestyle is key to diagnosing this condition.
After surgery, if mediastinitis develops, risk factors such as diabetes, obesity, smoking, kidney failure, and a weak immune system are important to note. The details of any past surgeries, including how long they took, if they happened repeatedly, or if they used a lot of cautery, are also significant. Physical signs of mediastinitis can include an unstable breastbone, discharge from the wound, and tenderness and pain. Slow recovery after surgery without any clear reason is another sign to watch out for. Most times, mediastinitis appears within a month of the surgery.
If a specific type of mediastinitis, called descending necrotizing mediastinitis, is suspected, it’s usually because a head or neck infection hasn’t been treated well and has spread. Patients with this condition may also have shortness of breath. Physical signs can include neck or chest pain, along with crepitus (a crackling feeling under the skin) and redness.
An insidious type of mediastinitis known as fibrosing mediastinitis often starts out with no symptoms. When symptoms do show up, they can include cough, shortness of breath, chest pain similar to pleurisy, coughing up blood, fever, or weight loss. Patients with this type of mediastinitis may also have a history of repeated lung infections. As the disease worsens, it can start to affect other organs nearby, leading to symptoms like superior vena cava syndrome. The patient’s travel history is also important because fibrosing mediastinitis is linked to diseases like histoplasmosis and tuberculosis.
Testing for Mediastinitis
If your doctor suspects that you have mediastinitis, which is inflammation of the area in the chest between the lungs, they’ll first check important basic body functions like your airway, breathing, and circulation. If needed, they might start emergency treatments even before doing any lab tests or imaging scans. Once your condition is stable, getting the right imaging scan becomes very important for diagnosing your situation.
A chest X-Ray could show signs like a wider mediastinum (the area between the lungs) or air in the mediastinum, but it often doesn’t give a detailed view of the whole condition. CT (Computed Tomography) scans and MRI (Magnetic Resonance Imaging) scans are better at helping the doctor assess mediastinitis because they provide a more detailed view.
If mediastinitis occurs after surgery, it can be hard to assess with imaging due to the natural changes after the surgery. The CT scan’s ability to accurately diagnose will notably improve after 14 days following the surgery. Additionally, your doctor may also perform a mediastinal aspiration – a procedure where a needle is used to extract fluid from the mediastinum – to aid in the diagnosis.
In a serious form of mediastinitis called descending necrotizing mediastinitis, imaging might show a wider mediastinum, fatter density in the mediastinum, fluid levels indicating an abscess (infected area with pus), or fluid around the lungs which is often associated with mediastinitis. If the pericardium (the sac-like covering around the heart) is affected, imaging may show thickening, fluid around the heart, or air around the heart. Moreover, a CT scan of your neck might be done to find the primary source of the infection.
Around that time, you’ll also likely have some lab studies done. These could show higher white blood cell count, high C-reactive protein, and increased procalcitonin levels – all signs of inflammation or infection. Blood cultures might also be done, especially if mediastinitis is suspected after surgery, as this condition is often associated with bacteria in the bloodstream.
If you have fibrosis mediastinitis, a chronic type of mediastinitis, the CT scan might show a mass that distorts the mediastinal fat planes and extends into surrounding structures. This could be spread through the mediastinum, or it could be localised to a specific area. It might also show calcifications (hardened areas caused by calcium build-ups), especially if you have an associated condition called histoplasmosis (a fungal infection). Narrowing in the airway, the bronchi (the tubes leading into the lungs), the main artery to the lungs or the superior vena cava (large vein) or the esophagus (tube leading to the stomach), as well as conditions causing lung damage can be common symptoms. Chest X-rays usually show abnormalities in these patients, although findings may be not very clear. A wider mediastinum with distortion of the mediastinum interfaces is frequently seen. In cases where the blood vessels to the lungs are involved leading to high pressure in these blood vessels, bronchial cuffing (swelling around the bronchi) and thickening of the septum (wall dividing left and right sides of the heart) may be present. Fluid around the lungs is seen less often.
Treatment Options for Mediastinitis
The treatment for acute mediastinitis, a serious infection in the area between the lungs, often involves immediately starting powerful antibiotics and undergoing surgery if needed. The antibiotics used at first are broad-spectrum, which means they can kill a wide variety of bacteria. After lab tests figure out exactly what bacteria is causing the infection, the doctors can switch to a more specific antibiotic.
When it comes to surgery, there are lots of different methods the doctors can use. The choice will depend on how severe and widespread the infection is. After the surgical intervention, the doctors will frequently check your progress through CT scans, lab tests, and physical evaluations. This helps them determine whether you might need more surgery. Patients with mediastinitis are usually taken care of in an intensive care unit because they need close monitoring and treatment.
Fibrosing mediastinitis, another form of the disease that leads to scar tissue in the chest, has an unclear cause, which makes it difficult to decide on a standard treatment. Medications for this condition are somewhat limited, but doctors often use treatments that suppress the immune system, steroids, or antifungal drugs due to the limited options available. If you have symptoms from fibrosing mediastinitis, you might need to undergo surgical procedures, such as placement of a stent (a small tube) to open up blocked areas, or bypass surgeries to route around blocked areas.
What else can Mediastinitis be?
When a patient might have mediastinitis, it’s really important for the doctor to look at all possible illnesses it could be. This is because the symptoms of mediastinitis can also be caused by other problems in the chest area or even elsewhere in the body. The doctor needs to promptly and accurately figure out what the problem is to ensure that the patient gets the right treatment as quickly as possible.
The conditions that mediastinitis can often be mistaken for include:
- Coronary artery disease
- Acute coronary syndrome
- Pulmonary embolism (a blood clot in the lungs)
- Pneumothorax (a collapsed lung)
- Aortic dissection (a serious condition where there’s a tear in the wall of your main artery)
- Cellulitis (a bacterial skin infection)
- An infection in the head or neck
- A type of growth like a tumor or mass
What to expect with Mediastinitis
Postsurgical and descending necrotizing mediastinitis are severe conditions that can result in serious harm or death if not treated promptly. Descending necrotizing mediastinitis, a severe infection of the area between the lungs, can lead to a death rate of 20% to 40% despite available treatment methods.
Fortunately, developments in surgery and better treatment methods have resulted in lower death rates for those experiencing postsurgical mediastinitis, a severe infection following chest surgery. Today, death rates vary from 1% to 14%, a significant decrease from previous rates which varied from 12% to 50%.
In comparison, fibrosing mediastinitis, a condition where fibrous tissue builds up in the area between the lungs, generally has a better outlook when it affects one side (unilateral) versus both sides (bilateral). However, despite the typically slow progression of this condition, patients frequently experience recurring pneumonia or pulmonary heart disease, a strain on the heart caused by a lung disease.
Possible Complications When Diagnosed with Mediastinitis
Mediastinitis is a serious condition that demands swift diagnosis and treatment. If not managed effectively, it can result in several severe complications, even putting the patient’s life in danger. Quick medical intervention can help control these risks and improve the patient’s health prognosis.
Here’s a list of possible complications from mediastinitis:
- Inflammation of the pericardium (Pericarditis)
- Inflammation of the heart muscle (Myocarditis)
- Repeated instances of pneumonia
- Formation of pus-filled cavities in the lung (Lung abscess)
- Build-up of fluid between the lungs and chest wall (Pleural effusion)
- An extreme response of the body to an infection leading to organ failure (Sepsis)
- Blocked airway
- Heavy bleeding or coughing blood (Hemoptysis)
- A condition in which the right side of the heart fails (Cor pulmonale)
- Failure of multiple organs in the body (Multiorgan failure)
- Scarring and fibrosis
- Long-lasting pain
- Complications arising from surgical treatment or removing dead tissue (debridement)
Preventing Mediastinitis
Preventing a condition called mediastinitis, especially for those who have had chest surgeries or invasive procedures, depends a lot on prevention and learning. It’s crucial that patients understand and follow care instructions before and after surgery to lower the chance of getting an infection. This includes taking care of any wounds properly, watching out for early signs of infection like redness, swelling, or fever, and getting medical help quickly if any symptoms appear. Doctors and nurses should point out how important it is to keep hands clean and keep everything in their surroundings clean to lower the risk of infections. Informing patients about possible complications and the need for follow-up visits makes sure problems are noticed and dealt with early on. Educating patients completely and having them follow prevention steps can reduce the chance of getting mediastinitis a lot.
Steps that can be taken during and after surgery to lower the chance of mediastinitis include using completely clean and sterile methods throughout surgery, making sure that any bleeding is controlled and the breastbone is closed properly. Using a preventative antibiotic gel in the nose for those who carry a common type of bacteria called S. aureus after surgery can lower the risk of an infection at the site of the surgery. Also, using an antibiotic ointment on the site of the surgery after heart surgery can reduce the chance of getting mediastinitis.