What is Pituitary Apoplexy?
Pituitary apoplexy is a condition where the pituitary gland located at the base of the brain suffers from a stroke or bleeding. This usually happens in a pre-existing tumor in the pituitary gland known as a pituitary adenoma. This stroke or bleeding leads to what is called “sudden death” of the pituitary gland, either due to the blood supply being cut off or severe bleeding. The first case of a stroke due to a pituitary tumor was reported in 1898 while the term ‘pituitary apoplexy’ started being used in 1950, to refer to the death of tissue and bleeding into pituitary tumors.
This situation is often a medical and surgical emergency. Quick recognition and evaluation of the condition are very important to help improve the patient’s outcome and prevent further complications.
What Causes Pituitary Apoplexy?
Pituitary apoplexy is often found in cases where a patient has an existing pituitary tumor, but in most of these cases, the patient doesn’t know they have a tumor. There are many factors that can contribute to pituitary apoplexy. These include certain endocrine tests, treatments with bromocriptine or cabergoline, gonadotropin-releasing hormone treatments, procedures like lumbar fusion, pregnancy, radiation directed at the pituitary, anticoagulation medication, a low count of platelets called thrombocytopenia, and even erectile dysfunction medications.
Sheehan syndrome is another condition that affects the pituitary gland. It typically happens to women after childbirth. The pituitary gland is damaged and dies off because of lack of blood flow, usually due to significant bleeding during childbirth. This syndrome results in inadequate functioning of the adrenal glands, thyroid gland, and other parts of the body controlled by the pituitary gland, but it rarely involves changes to vision. This condition usually isn’t grouped with pituitary apoplexy because it doesn’t not involve a pre-existing tumor, and rarely does it ever cause visual symptoms.
Risk Factors and Frequency for Pituitary Apoplexy
Pituitary apoplexy, a type of rare event that affects pituitary adenomas, or tumors in the pituitary gland, ranges from 1.5-27.7% in cases according to various reports. Some of these reports do not distinguish between those who show symptoms and those who do not. If we consider only the instances where patients showed symptoms, the incidence is about 10%. However, when including cases where there was a silent or non-symptomatic bleeding within the tumor, which was detected by brain imaging, the rate goes up to 26%.
Pituitary apoplexy is quite rare in adenomas, with an estimate of 0.2% per year. The risk increases with larger tumors (more than 10 cm) and in those which have shown quick growth.
Most people who experience this condition are aged between 37 and 58. In terms of gender, it is seen twice as often in males as compared to females.
Signs and Symptoms of Pituitary Apoplexy
Pituitary apoplexy is a medical condition that typically starts with a sudden headache behind the eyes. Other symptoms may include blurry vision, loss of side vision, double vision, droopy eyelids, nausea, vomiting, change in mental status, hormonal problems, and one eye pointing outwards. Patients may also experience pupil enlargement in the affected eye. Some individuals may complain about seeing double due to pressure on one or more nerves controlling eye movements, with the oculomotor nerve often affected. This can result in droopy eyelids and lateral eye deviation.
- Sudden headache behind the eyes
- Blurry vision
- Loss of side vision (hemianopia)
- Double vision (diplopia)
- Droopy eyelids (ptosis)
- Nausea and vomiting
- Change in mental status
- Hormonal problems
- One eye pointing outwards (lateral eye deviation)
- Pupil enlargement in the affected eye
In more than two-thirds of pituitary apoplexy cases, the pituitary gland stops secreting a hormone called adrenocorticotropic hormone (ACTH). As ACTH controls the secretion of cortisol from the adrenal gland, its absence can result in a set of symptoms known as an “adrenal crisis”. During an adrenal crisis, patients may experience nausea, vomiting, abdominal pain, slow heart rate, low blood pressure, low body temperature, fatigue, and in severe cases, even coma.
- Nausea and vomiting
- Abdominal pain
- Slow heart rate (bradycardia)
- Low blood pressure (hypotension)
- Low body temperature (hypothermia)
- Fatigue (lethargy)
- Coma (in severe cases)
Testing for Pituitary Apoplexy
A non-contrast head CT scan (Computed Tomography), which is a type of imaging that uses special X-ray equipment to take pictures of your brain, is usually the first step for doctors when trying to diagnose a certain type of brain tumor. This is done because these scans are relatively quick and easy to obtain. The CT scan shows a tumor in and above the sella of the brain (area where the pituitary gland sits) that is accompanied by bleeding within the tumor. However, it can’t specifically show if there is any tissue death due to low blood supply within the tumor or gland.
After the non-contrast scan, a contrast examination is performed. This involves using a special dye to highlight the areas of the body being examined. It helps to clearly outline the size of the tumor because regions with bleeding or dye enhancement appear brighter than the brain.
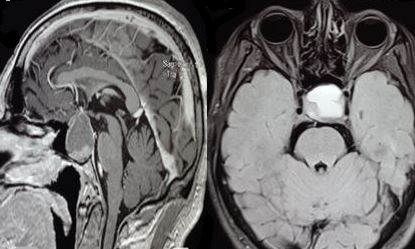
A Brain MRI (Magnetic Resonance Imaging), is done to give a more detailed picture of the brain tumor. MRI is the preferred imaging choice because it can clearly identify areas of bleeding and tissue death within the tumor. For an ischemic pituitary tumor, which means the tumor has not received enough blood, the MRI will show an enlarged sella/suprasellar mass with a brighter outer layer surrounding a darker center. The MRI can also identify the physical state of the tumor and spot tissue death due to a possible blockage in the blood vessels. If the tumor is hemorrhagic, meaning it has some bleeding, the MRI will show a brighter signal within the areas of the tumor indicating the presence of blood. The MRI T2 star gradient echo sequence is a special sequence which is extremely sensitive in picking up the presence of a certain form of iron present in red blood cells called hemosiderin.
In addition to imaging, a hormonal evaluation of the pituitary gland is needed as well because almost 80% of patients with this condition have at least one deficiency in the hormones produced by this gland. The most commonly deficient hormones are the growth hormone, lacking in 90% of patients, and ACTH (Adrenocorticotropic hormone), which is absent in 70% of patients.
Doctors also use a 5-grade classification system, based on the symptoms and signs that the patient presents with, to determine treatment decisions and predict the outcome.
Treatment Options for Pituitary Apoplexy
When a patient experiences a pituitary apoplexy, a condition where there is sudden bleeding or swelling in the pituitary gland at the base of the brain, immediate medical care involves keeping the body’s fluids and electrolytes balanced and stable. Corticosteroid medications, which help to reduce inflammation, are also typically given to all patients, even if they aren’t showing signs of severe adrenal gland dysfunction. However, the exact dosage will depend on the individual patient’s needs and response to treatment.
The treatment plan for the pituitary tumor causing the apoplexy can vary. Some doctors recommend early surgery to reduce the size of the tumor in all patients, while others suggest a less aggressive approach for patients who aren’t showing severe symptoms such as vision loss or impaired consciousness. Patients with rapidly worsening symptoms, such as a decline in consciousness, involvement of the area of the brain that controls body temperature and thirst (the hypothalamus), and deteriorating vision, may need emergency surgery.
Surgery has been found to significantly improve symptoms postoperatively, especially when performed as soon as possible. In some cases, doctors may delay surgery for about a week if the patient’s vision impairment appears to be stable. If the patient’s eye muscle function issues are improving or stable, doctors may consider a wait-and-see approach.
Common surgical methods include microscopic endonasal or sublabial transsphenoidal surgeries, which involve removing the tumor through the nose or under the upper lip respectively. For larger tumors, or tumors that have spread to other parts of the brain, a craniotomy, a surgical procedure where part of the skull is removed, may be necessary to adequately remove the tumor.
Endoscopic endonasal approaches, where a thin tube with a camera on the end (an endoscope) is used to view and remove the tumor through the nose, are effective for pituitary apoplexy. However, the procedure may be challenging to perform if needed during late hours, as it requires the collaboration of an ear, nose, and throat specialist with a neurosurgeon.
In children, pituitary tumor apoplexy can be more aggressive than in adults, and early surgery may lessen its frequency and improve outcomes.
What else can Pituitary Apoplexy be?
There are several medical conditions that can mimic the visual and headache symptoms associated with pituitary apoplexy. Some of these conditions can be managed with medicine, while others may need a different type of surgery. These conditions include:
- Rathke’s cleft cyst
- Temporal arteritis
- Aneurysm
- Craniopharyngioma
- Subarachnoid hemorrhage
- Meningitis or encephalitis
- Cavernous sinus thrombosis
- Basilar artery infarct
- Hypertensive encephalopathy
- Ophthalmoplegic migraine
- Retrobulbar neuritis
What to expect with Pituitary Apoplexy
Pituitary apoplexy is a serious condition that could be life-threatening if not caught and treated. On average, the death rates due to this condition are between 1.6% and 1.9%.
Most patients with this condition experience improved vision, less visual field defects, and better eye muscle function after both medical and surgical treatment. Eye function improvement is typically seen right after surgery and continues for several weeks post-surgery. However, vision tends to recover less in patients who already have partial or total blindness in one or both eyes.
While early intervention may lead to better visual outcomes, research shows that changes in visual deficits, resolution of eye muscle paralysis, recovery from hormone deficiency caused by pituitary damage, or other signs and symptoms like headaches and confusion, don’t necessarily depend on when the surgery is carried out. Regaining normal eye muscle function usually takes about 3 months, while recovering from abducens nerve palsy typically takes around 6 months.
Overall, visual improvements are seen in 75 to 85% of patients, normal vision is regained in 38% of patients, and preoperative eye muscle paralysis is rectified in 81% of patients.
Complete removal of the tumor and a shorter duration of preoperative headaches significantly increase the chances of post-surgery headache improvement. Also, it’s important to note that 80% of the patients will likely need hormone replacement therapy. In some cases, the tumor may naturally shrink over time, and surgery isn’t needed. This is typically caused by a cut-off of the blood supply to the tumor tissue, resulting in its death.
Possible Complications When Diagnosed with Pituitary Apoplexy
The list of medical conditions includes:
- Visual loss
- Adrenal crisis
- Ophthalmoplegia
- Increased pressure within the skull
- Ptosis
- Diabetes insipidus
- Brain damage affecting both sides of the brain
Preventing Pituitary Apoplexy
If you have experienced a medical condition called pituitary apoplexy, where there’s sudden bleeding or insufficient blood supply in the pituitary gland located at the base of the brain, you may have ongoing hormone imbalances. Therefore, doctors will schedule a checkup for you between 4 to 8 weeks after the incident to see how your pituitary gland is functioning.
It’s crucial for your doctors to monitor your vision and the movement of your eyes, and to check the field of your vision, in these check-ups. This is because pituitary apoplexy can affect these capabilities.
Additionally, doctors generally suggest you to get an MRI scan, a type of imaging test, about 3 to 6 months after the bleed to monitor any remaining tumor tissue. Then, they might suggest you to keep doing this scan every year for the following 5 years, just to keep a tab on things.
If you already know about a tumor in your pituitary gland, it’s important to be aware that this tumor could bleed. In order to manage this risk, it’s vital to regularly see both your hormone specialist (endocrinologist) and brain specialist (neurosurgeon) as per their suggested schedule. You should also quickly seek medical professional help if you notice a sudden change in your vision or if you have a major headache.