What is Raynaud Disease?
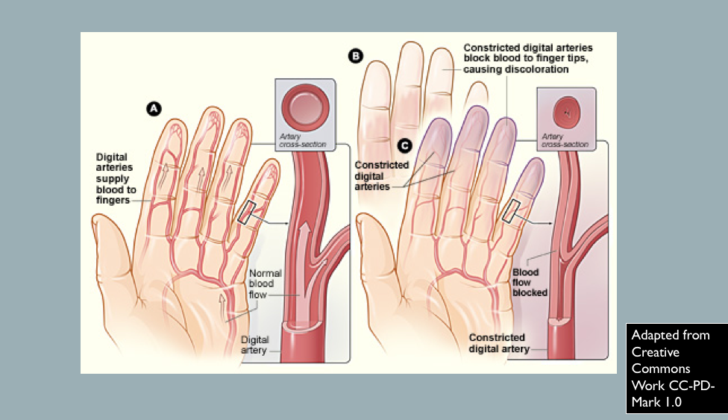
When it gets cold, your body protects itself by limiting the blood flow to your skin. This helps keep your body warm and maintain a steady internal body temperature. However, in a condition called Raynaud’s phenomenon, your body restricts blood flow to your fingers and toes not just when it’s cold, but also in situations of emotional stress.
These blood vessels constrict, limiting blood flow to the digital arteries— the blood vessels in your fingers and toes— and the skin’s small arteries. This response was initially documented by Maurice Raynaud in 1862 and studied further by Sir Thomas Lewis in 1930.
In general, Raynaud’s phenomenon is a temporary narrowing of blood vessels that happens in response to cold temperatures or emotional stress. This situation can be either ‘primary’ (happening on its own) or ‘secondary’ (occurring as a result of another condition).
What Causes Raynaud Disease?
Raynaud’s phenomenon, a condition that affects the blood flow to certain parts of the body like your fingers and toes, can be caused (secondary Raynaud’s phenomenon) by several things.
It is often linked with disorders affecting your connective tissues, which are the tissues that help support and give structure to other tissues and organs. These can include conditions like scleroderma (which causes skin to harden), systemic lupus erythematosus (a long-term condition leading to inflammation to many body parts), Sjogren syndrome (disease affecting the areas of the body that produce fluids like tears and saliva), and antiphospholipid syndrome (a disorder that causes blood clots).
Certain medications might cause this type of Raynaud’s phenomenon. These can include drugs for migraines, drugs that modulate the body’s immune response (interferon alpha and beta), medicines that help prevent organ rejection in transplant patients (cyclosporine), and particular medications used for heart conditions known as non-selective beta blockers.
Raynaud’s phenomenon can also be triggered by jobs involving repeated exposure to vibrating machinery (mostly affecting men). This is referred to as hand-arm vibration syndrome. Other vocational causes include exposure to a type of plastic called polyvinyl chloride, injuries due to cold temperatures at work, or work related to ammunition.
In people over the age of 60, diseases that block blood vessels (obstructive vascular diseases) are a common cause of Raynaud’s phenomenon. This includes conditions like thromboangiitis obliterans (a rare disease that inflames small- and medium-sized blood vessels), microemboli (tiny blood clots), diabetic angiopathy (blood vessel damage due to diabetes), or atherosclerosis (build-up of fats, cholesterol and other substances in and on the artery walls).
Infections, including parvovirus B19, cytomegalovirus, hepatitis B, and hepatitis C have also been linked to Raynaud’s phenomenon.
Other conditions such as fibromyalgia (causes pain all over the body), polycythemia (body makes too many red blood cells), arteriovenous fistula (abnormal connection between arteries and veins), myalgic encephalitis (long-term illness causing fatigue), or malignancy (presence of cancer in the body) can also cause secondary Raynaud’s phenomenon.
Risk Factors and Frequency for Raynaud Disease
Raynaud’s phenomena, a condition that affects your blood vessels, is more common in women, especially in those between their teens and 20s. In fact, for every 9 women who have the condition, there is only 1 man with the same issue. So, the condition is nine times more likely in women than in men.
Signs and Symptoms of Raynaud Disease
Raynaud’s phenomenon is a condition where cold temperatures or emotional stress can cause the skin on a person’s fingers and toes to become cold, numb, and change color. Here are some key points we need to check when diagnosing it:
- Age when symptoms first appeared
- Which areas of the body are affected
- Whether it affects both sides of the body equally
- Possibility of skin ulcers
- Severity of the symptoms
- Presence of other systemic symptoms
- Identifying if cold temperatures or emotional stress provoke it
- If there’s increased risk due to stress, patient’s gender, cold temperature or a concurrent connective tissue disease
- If symptoms started later in life (age 30s and 40s), as this could increase the risk of a connective tissue disorder developing along with it
An attack of Raynaud’s often begins suddenly. It generally starts in one finger, then spreads to others on both hands symmetrically. The thumb usually isn’t involved. The fingers become cold, and they look pale or even blue. This “white or blue attack,” as it’s called, can last for about 20 minutes. Then, blood flow returns, causing affected areas to turn red as they warm up – a process known as reactive hyperemia.
If other areas, like the face, ears, knees, or nipples are affected, it may be a sign of secondary Raynaud’s. The condition may also cause numbness, a pins and needles sensation, or even aches and pains in fingers. In serious cases, it can lead to ulcers on the tips of fingers and toes, or even gangrene which could cause the loss of fingers or toes. These severe symptoms typically accompany secondary Raynaud’s in comparison to primary forms of the disease.
Another notable skin change during a Raynaud’s attack can be the presence of a purplish, mottled pattern on the skin – a condition called livedo reticularis. This results from tiny blood clots in the skin. It’s reversible with re-warming, but can become permanent with secondary disorders like antiphospholipid syndrome, vasculitis, cold agglutinin disease, or peripheral vascular disease.
Testing for Raynaud Disease
Nailfold capillary microscopy is a diagnostic test used to distinguish between primary and secondary Raynaud’s phenomenon. This condition causes some areas of your body, like your fingers and toes, to feel cold and numb in response to cold temperatures or stress. “Primary” means it occurs on its own, while “secondary” means it is caused by another health condition, often a connective tissue disorder (CTD).
This test looks for changes in tiny blood vessels and the structure of certain peripheral blood vessels associated with connective tissue disorders. It checks for variations in the shape, size, and number of capillaries (tiny blood vessels), the presence of bleeding, and areas without capillaries loops. The test is performed using tools like a dermatoscope or ophthalmoscope, which magnify the area for detailed examination. Another method is called videocapillaroscopy that involves recording the images.
If the test shows abnormalities—like enlarged capillary loops or a loss of them—it correlates with a higher likelihood of developing a connective tissue disorder. If ‘mega-capillaries’ (extremely large capillaries) are seen with a decreased number of capillaries overall, these changes might suggest a disease called scleroderma, which causes hardening and tightening of the skin and connective tissues.
Treatment Options for Raynaud Disease
The goal of treating Raynaud’s phenomenon, a condition where certain parts of the body like fingers and toes feel numb and cold in certain conditions, is to lessen the number and intensity of attacks, and to stop tissue from getting insufficient blood supply (ischemia). Treatment success is checked by the Raynaud Condition Score (RCS). This scoring system checks the quality of life, frequency and severity of attacks, and the effect of Raynaud’s phenomenon on an individual’s life.
The first step in managing Raynaud’s phenomenon is to make lifestyle changes such as avoiding cold, staying warm, avoiding things that excite your nervous system, avoiding anxiety or emotional stress, and not smoking.
If these changes don’t improve the patient’s symptoms, medication that helps widen the blood vessels (vasodilating mechanism of action) is used. A type of medication called dihydropyridine calcium channel blockers (DHP CCBs), including amlodipine and nifedipine, are usually the first choice of treatment for Raynaud’s phenomenon. When starting these types of medication, the dosage begins low and is gradually increased every 4 weeks depending on how the patient responds to it. It is important to keep an eye on blood pressure response, especially if patients have naturally low blood pressures.
Side effects of DHP CCB include swelling in the lower extremities (peripheral edema), a rapid heart rate (palpitations, reflex tachycardia), dizziness, and headaches. These medicines are not suitable for people with low blood pressure (hypotension), peripheral edema, chest pain (angina), heart attack (myocardial infarction), and certain heart conditions. The use of these drugs during pregnancy is generally avoided.
If the symptoms don’t get better after using DHP CCB therapy, another type of drug called a phosphodiesterase (PDE) inhibitor will be used. If the CCB treatment has caused some improvements, the PDE inhibitor can be added to the current therapy. If there’s no improvement with the CCB, then the PDE inhibitor can be used on its own. Sildenafil is one of the commonly used PDE inhibitors.
If these treatments don’t help, other options include using topical nitrates, such as nitroglycerin, which is a potent blood vessel widener that’s applied directly to the affected areas. Although this medication gets into the bloodstream and can cause side effects like low blood pressure, dizziness, and headache.
In case all the above medications don’t work, other options like losartan, fluoxetine, and prazosin can be used. If blood supply to the fingers or toes (tissues) are compromised and symptoms are severe, then prostaglandin, a potent blood vessel widener, is given through IV. This also prevents blood cells from sticking together (platelet cell aggregation).
For cases of Raynaud’s phenomenon that don’t respond to treatment and have recurring skin sores (ulcers) in the fingers or toes, another option is Bosentan, which prevents blood vessels from constricting. In extreme cases, surgery to remove certain nerves causing blood vessels to constrict (sympathectomy) may be considered. In cases of secondary Raynaud’s phenomenon where there has been a history of insufficient blood supply causing sores, low dose aspirin should be taken daily. If aspirin can’t be taken, other options include clopidogrel or dipyridamole.
What else can Raynaud Disease be?
Raynaud phenomenon is a condition that can be confused with several other diseases or conditions due to apparent similarities. These include:
- External blood vessel compression
- Complex regional pain syndrome
- Erythromelalgia
- Acute idiopathic blue finger or paroxysmal finger hematoma
- Acrocyanosis
- Occlusive peripheral vascular disease
- Peripheral neuropathy
- Excessive cold sensitivity
What to expect with Raynaud Disease
In the case of what’s known as primary Raynaud’s phenomenon, where a person’s fingers or toes temporarily turn blue or white due to low temperature or stress, it’s possible for the condition to naturally disappear without treatment, an event known as spontaneous remission. Unfortunately, this sort of spontaneous remission doesn’t happen with what’s known as secondary Raynaud’s phenomenon, which is typically a more severe form and is often caused by another underlying health condition.
Interesting enough, pregnancy has been noted to improve the condition of Raynaud’s phenomenon. This is possibly due to the increase in red blood cell count and amount of plasma (liquid part of the blood), which happens during pregnancy. These changes tend to enhance the flow and oxygen supply to the different parts of the body.
Possible Complications When Diagnosed with Raynaud Disease
Severe Raynaud’s phenomenon can cause a lack of blood supply to tissues, leading to tissue death. This could potentially result in amputation of the affected area.