What is Rhinophyma?
Rhinophyma is a condition that alters the shape of the nose due to unusual growth of oil-producing glands and the supporting tissue beneath. The term ‘Rhinophyma’ comes from two Greek words: ‘rhis’, which means nose, and ‘phyma’, which means skin tumor. Rhinophyma is the most common form of these abnormal swellings, but the condition can also appear on different parts of the body, including the chin (Mentophyma), forehead (Metophyma), chin (Gnatophyma), ears (Otophyma), and eyelids (Bleharophyma).
Rhinophyma usually develops as a severe form of a skin condition known as rosacea. The connection between rosacea and rhinophyma was first established in 1846 by Ferdinando Hebra Von. The condition is not new and has been depicted in artwork, such as in a 15th-century painting by Domenico Ghirlandaio showing a man with a large rhinophyma.
It’s essential to treat this condition because it can cause significant emotional distress and breathing problems, especially when it thickens parts of the nose, blocking air passage. Another challenge with this condition is the incorrect but widespread belief that it’s caused by heavy drinking, leading to negative stereotypes. This has resulted in nicknames like “whiskey nose”, “gin blossom”, and “potato nose”. This misconception has not been proven scientifically, but it continues to create social stigma. Movies also contribute to this stigma, as they often give characters with rhinophyma villainous roles, like the evil queen in “Snow White and the Seven Dwarfs”.
What Causes Rhinophyma?
Rosacea was once thought to progress in stages, starting with red and flushed skin (erythematotelangiectatic rosacea), then progressing to bumps and pimples (papulopustular rosacea), and finally resulting in thickened skin (phymatous rosacea). However, since many people show symptoms of these different types at the same time, doctors now classify and diagnose rosacea based on the person’s specific symptoms (phenotypes).
Rosacea often begins when a person is between 20 and 30 years old and includes symptoms like facial redness, flushing, and tiny, visible blood vessels. These symptoms can be made worse by things like caffeine, alcohol, and sunlight.
The root cause of these changes is complicated and isn’t fully understood, but it involves an overactive immune system. This can lead to inflammation, swelling, and redness on the skin. Mast cells – a type of immune cell – also play a role by expanding blood vessels and promoting the formation of new ones.
Another factor is the production of angiotensin II – a substance that causes blood vessels to contract and dilate. The shifting of these blood vessels can lead to persistent inflammation and ultimately the enlargement of the sebaceous glands (glands that produce an oily substance known as sebum) and hardening of skin tissue.
When this happens around the nose, it can cause the skin to swell and thicken, particularly around the nose tip and sides. It’s important to note that the underlying bone structure does not change; only the skin around it expands.
There’s also a mite named Demodex folliculorum that lives in our sebaceous glands. The role this mite plays in rosacea is not fully understood, as it’s not yet certain whether its presence causes rosacea, or if it’s simply more common in people who already have the condition.
Risk Factors and Frequency for Rhinophyma
Rosacea is a skin condition that is generally seen more in women. However, a specific type of rosacea called rhinophyma is usually found in white men over the age of 50. The number of affected men to women ranges from 5 to 1 or even up to 30 to 1. It’s not common, but there have been reports of Asian or African American men having rhinophyma. There’s a theory that male hormones might make men more prone to developing rhinophyma.
Signs and Symptoms of Rhinophyma
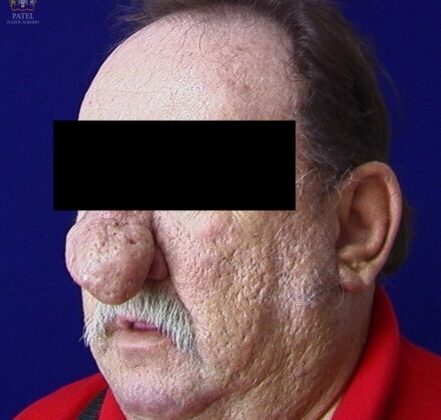
Rhinophyma is a condition that can be identified by redness, visible blood vessels, and thickened skin around the nose. Typically, the bottom two-thirds of the nose shows these symptoms more than the top third. While there isn’t a specific test to diagnose rhinophyma, a tissue sample can help to confirm the diagnosis.
Rhinophyma is considered a late stage of rosacea, a skin condition that was divided into four stages by Wilkin in 1994. These stages include pre-rosacea, vascular rosacea, inflammatory rosacea, and late rosacea. In 2002, the National Rosacea Society further refined these classifications, creating a set of primary and secondary features for diagnosing rosacea.
In order to diagnose rosacea, an individual must exhibit at least one primary feature and one secondary feature.
- Primary features of rosacea include:
- Transient erythema (temporary redness)
- Non-transient erythema (constant redness)
- Papules (small raised bumps on the skin)
- Pustules (small pus-filled bumps)
- Telangiectasia (visible blood vessels)
- Secondary features of rosacea include:
- Sensitivity of facial skin (burning or stinging)
- Plaques (patches of skin)
- Edema (swelling)
- Ocular manifestations (eye symptoms)
- Non-facial involvement
- Phymatous changes (enlargement of the skin)
In 2019, the Global Rosacea Consensus (ROSCO) Panel introduced similar categories for rosacea classification, which include:
- Diagnostic features:
- Phymatous changes
- Persistent erythema
- Major Features:
- Flushing and transient erythema
- Papules and pustules
- Telangiectasia
- Minor Features:
- Burning sensation
- Stinging or painful sensation
- Dry sensation
- Localized facial swelling
Testing for Rhinophyma
Rhinophyma is a skin condition that doesn’t require lab tests or scans for diagnosis. It’s identified and classified by examining the patient. There are different types and levels of severity for this condition.
Here are the four main types of rhinophyma:
- Glandular rhinophyma: This type occurs due to the growth of sebaceous glands (small glands in the skin that secrete a lubricating oily matter).
- Fibrous rhinophyma: This involves the abnormal growth of connective tissue (tissue that supports, connects, or separates different types of tissues and organs in the body).
- Fibroangiomatous rhinophyma: This is characterized by fibrosis (thickening and scarring of connective tissue), telangiectasias (small dilated blood vessels near the surface of the skin), and inflammatory lesions (abscesses that are caused by inflammation and filled with pus).
- Actinic rhinophyma: This type is caused by the growth of elastic fibers in bumpy masses, which result in disfigurement.
Rhinophyma is also classified based on its severity. The scale defined by researcher Freeman and his colleagues starts with an early vascular type and progresses to:
- Moderate diffuse enlargement (widespread swelling)
- Early localized tumor (start of a small growth)
- Extensive diffuse enlargement (widespread, significant swelling)
- Extensive with localized tumor diffuse enlargement (significant swelling with a small growth).
Another way to classify rhinophyma is by grading it as minor, moderate, or major. According to a system used by researcher El-Azhary and his team:
- Rhinophyma is minor if there is the presence of dilated blood vessels with minor skin thickening.
- It’s moderate if skin thickening is accompanied by small rounded lumps.
- It’s major if there are noticeable nodules (abnormal growth of tissue) and nasal hypertrophy (abnormal enlargement of the nose).
The National Rosacea Society also has a standard grading for rosacea and phymatous changes (changes related to an overgrowth of tissue), rated from 0 (absent) to 3 (change in shape of the nose with a knobby component).
After the doctor has evaluated your rhinophyma, they will discuss treatment options with you. You always have the option to opt-out of any surgical treatment. If your condition is either severity level 1 or 2, you might choose to simply continue to observe the situation. It’s advisable to take clinical photos at regular intervals to keep track of any changes.
Treatment Options for Rhinophyma
Rosacea, a skin condition that causes redness and visible blood vessels in the face, can be effectively managed with treatments such as antibiotics and isotretinoin, a medication typically used for severe acne. This approach usually works best for mild to moderate cases. Isotretinoin helps reduce symptoms by reducing sebum (a waxy substance produced by the skin) and the size of the skin’s oil glands. However, certain topical treatments, such as Retin-A, might make rosacea worse due to increased irritation and redness.
Rhinophyma, a severe form of rosacea which results in a bulbous, enlarged red nose, can’t be addressed with these treatments. Its management often involves surgical procedures to remove excessive tissue and reshape the nose. But before surgery, the patient should stop taking oral isotretinoin as it could hinder skin healing.
In the past, X-ray therapy was used to treat rhinophyma as it was known to decrease the size of oil glands and promote the shrinking of skin structures that produce hair and oil. This approach is now avoided due to the risk of skin cancers.
Surgical procedures for rhinophyma aim to reduce the enlarged oil glands and reshape the nose. This involves substantial removal of the affected tissue, reshaping of the nose, and controlling of excessive bleeding to prevent complications after the surgery. There are different techniques used in these procedures, including full-thickness resection with reconstruction, partial removal of the tissue, cryosurgery (freezing off the tissue), and dermabrasion (a procedure that exfoliates the outermost layers of skin). However, each of these techniques has its own set of challenges and may not be suitable for everyone.
Surgery can also involve the same technology used for tattoos or hair removal, including electrosurgery and electrocautery, where heat or electric current is used cut or destroy tissue. A technique known as Coblation, where radiofrequency energy is used to remove tissue at a low temperature, can also be used.
Laser treatment is another popular choice. Lasers such as the CO2 laser or the Er: YAG laser, have been used successfully to cut and vaporize the skin in a controlled manner, with an aim to destroy the overactive oil glands. Other types of laser, such as diode laser, Nd: YAG laser, and KTP laser have also been used successfully.
Research is also underway on non-surgical treatments for rhinophyma. It has been proposed that certain proteins may play a role in rhinophyma’s skin thickening, and medications such as tamoxifen, which is an anti-estrogen drug, might help inhibit these proteins and thus, reduce fibrosis or tissue thickening.
What else can Rhinophyma be?
Rhinophyma, a skin condition that causes the nose to become large, bulbous, and red, has a unique appearance. However, it can be confused with other conditions that look similar. For instance, one case initially thought to be rhinophyma was later confirmed to be basal cell carcinoma, a type of skin cancer. In fact, basal cell carcinoma is believed to develop in 3 to 10% of patients with rhinophyma, easily hiding amidst the lumpy skin.
Besides basal cell carcinoma, several other conditions have also been misdiagnosed as rhinophyma. These include:
- Adenoid squamous cell carcinoma
- Squamous cell carcinoma
- Sebaceous adenoma
- Sebaceous carcinoma
- Angiosarcoma
- Sarcoidosis
- Lymphoma
- Metastatic lung cancer
- Granuloma eosinophilicum
In parts of the world where leishmaniasis—a disease caused by the Leishmania parasite—is common, any patient with a progressively swelling nose resembling rhinophyma should be tested for this disease. The testing involves a smear and a PCR test, while treatment generally uses a drug called intramuscular meglumine antimoniate.
What to expect with Rhinophyma
The surgical treatment of rhinophyma, a skin condition that causes a large, red, and bumpy nose, often results in improved physical appearance in the short-term. However, there are few studies that discuss the likelihood of the condition returning in the long term.
For instance, in a survey of 52 people who received a specific type of laser treatment, all who responded confirmed that they were still experiencing the positive effects of the treatment after five years. However, another study tracked the return of rhinophyma in 21 individuals who were treated by shaving off the affected skin. Just around half of these individuals, after an average follow-up period of 13.2 months, reported a slow return of the condition.
The cause of this recurrence may be due to the fact that shaving does not entirely remove the part of the skin where oil and hair grow, coupled with a worsening of the underlying condition.
We are still awaiting more research to understand this condition, its recurrence, and its treatments better.
Possible Complications When Diagnosed with Rhinophyma
Common complications of surgical treatments include the formation of scars and a long healing period. The tip of the nose and the sides of the nostrils are particularly at risk for scarring because the cartilage is closer to the skin’s outer layer.
Techniques like heated scalpels, ablation therapy or laser treatments can also potentially lead to damage from heat, causing more scarring, burns, and changes in skin texture. If the skin is cut too deeply by mistake, it can also make the healing process more difficult, as the structures underneath the skin are essential for the skin to reform.
It’s important for surgeons to take care not to damage the nasal cartilages when using any excision technique.
Common Side Effects:
- Scarring
- Long healing time
- Risks related to certain treatments: thermal damage, additional scarring, burns, changes in skin texture.
- Complications from deep skin cuts
- Potential damage to nasal cartilages
Recovery from Rhinophyma
After a surgery where a lump or mark is removed from the skin, the usual aftercare involves applying antibiotic ointment, as well as ointments containing vitamins A and D, and petroleum jelly. This is done to help the wound heal and to keep it moist. Special bandages that don’t stick to the wound, and agents that help stop bleeding, can be used for 7 to 10 days. This helps to keep bleeding under control, lowers the risk of infection, and aids in the healing of the wound. Some studies discuss the use of special wound dressings, such as calcium alginate, a substance derived from seaweed that’s used in wound healing, oxidized cellulose polymer soaked with fibrin sealant, which is a protein that aids in blood clotting, and a gauze soaked in petroleum and microfibrillar collagen, a type of protein, or triple antibiotic ointment.
There are also reports of successful healing after using fibrin glue, which is a type of medical adhesive, following dermabrasion, which is a skin-resurfacing procedure. Lastly, there have been reports of a technology that speeds up skin healing called sprayable skin. This technology involves preparation of a cell suspension from the patient’s own cells which is sprayed under a bandage that keeps out air. This can hasten the process of reepithelialization, which is where new skin cells grow to cover a wound.
Preventing Rhinophyma
Patients should be informed on how to properly manage early-stage rosacea, a skin condition that causes redness and visible blood vessels, as well as advanced rosacea (also known as phymatous rosacea) which can lead to skin thickening and bumpy texture. While the progression to a stage called rhinophyma (skin thickening on the nose) can’t be stopped completely, managing the condition effectively can lessen its symptoms. This, in turn, can reduce the mental stress that often accompanies the condition.
A vital part of managing early-stage rosacea is learning what to avoid to prevent skin flushing (reddening) and lasting redness. Patients are advised to avoid environmental factors such as extreme heat and cold, and sunburn. Emotional triggers like excessive stress and anxiety should also be controlled. Physiological stimuli like caffeine, alcohol, spicy foods, and heavy exercise should be limited. Certain external factors, like chemical peels and other skin irritants, should also be avoided. Given that rosacea can increase transient epidermal water loss (quick evaporation of water from the skin’s surface), it’s essential for these patients to moisturize regularly.
Consistent use of sunscreen is also important to avoid worsening the condition from sunburns and to prevent an increase in free oxygenated radicals (harmful molecules) that can aggravate rosacea. For patients with more severe rosacea, they can start using a skin cream called metronidazole which has been shown to effectively reduce bumps and pimples. Oral antibiotics, like tetracyclines, or erythromycin for those who can’t tolerate tetracyclines, can provide anti-inflammatory benefits. Those with advanced rosacea should be informed about the usefulness of a medication called oral isotretinoin which can reduce the growth of enlarged oil glands and the amount of superficial blood flow. They should understand that surgical treatment might be necessary to remove excess skin, but it should be noted that there’s a possibility of the disease coming back after the tissue is removed.