What is Saccular Aneurysm?
An aneurysm is a bulge or dilation in a blood vessel due to inherent weakness in the wall of the vessel. Although aneurysms can appear in any blood vessel, they are more often seen in arteries than in veins. Aneurysms can be of two types: a true aneurysm or a false aneurysm. True aneurysms involve all three layers of the arterial wall, while false aneurysms, also known as pseudoaneurysms, only involve the outer layer of the artery.
Aneurysms can also be categorized by their shape, location in the body, or cause. They can either be sac-like (saccular) or spindle-shaped (fusiform). Most brain aneurysms (90%) are saccular, unlike aneurysms in the aorta (main blood vessel in the body), 94% of which are fusiform.
This explanation particularly looks at saccular aneurysms in the brain and the aorta. Saccular brain aneurysms can be further classified by their size:
– Small: 5 mm or less
– Medium: 6 mm to 14 mm
– Large: 15 mm to 25mm
– Giant: More than 25mm
Most saccular aortic aneurysms are found in the descending part of the thoracic aorta. Many brain aneurysms produce no symptoms, remain small, and are often discovered by chance during brain imaging or an autopsy. Approximately 85% of cerebral aneurysms are located in the front part of the blood circulation, primarily at the junctions of the arteries in the “circle of Willis” (a group of arteries at the base of the brain) and the middle cerebral artery.
What Causes Saccular Aneurysm?
Cerebral saccular aneurysms, which are a type of brain aneurysm, are not completely understood. It is thought that they are linked with changes in the blood vessels brought about by abnormal blood flow patterns. Inflammation also plays a role in creating these aneurysms. While most are acquired, meaning they develop due to lifestyle or environmental factors, they can also be inherited.
Factors that increase the risk of developing a cerebral saccular aneurysm include:
* Getting older
* High blood pressure
* Heavy drinking
* Smoking
* Hardening of the arteries in the brain (atherosclerosis)
* Head injuries
* Use of drugs like cocaine
* A lack of estrogen
There are also genetic conditions that can increase the risk of developing a cerebral saccular aneurysm. These include:
* Polycystic kidney disease
* Arteriovenous malformation
* Ehlers-Danlos syndrome
* Marfan syndrome
* Loeys-Dietz syndrome
* Fibromuscular dysplasia
* Hereditary hemorrhagic telangiectasia
* Tuberous sclerosis
* A family history of aneurysms
* Alpha-glucosidase deficiency
* Alpha 1-antitrypsin deficiency
* A narrow section in the aorta (coarctation of the aorta)
* Klinefelter syndrome
* Noonan syndrome
* Female gender
Having a family history of brain aneurysms or subarachnoid hemorrhage – a type of stroke caused by bleeding around the brain – greatly increases the risk of aneurysm rupture. Also, exposure to nicotine can increase the risk of aneurysm rupture by impacting the cells of the blood vessels.
Saccular aortic aneurysms, another type of aneurysm that occurs in the aorta (the main artery in the body), have similar causes to saccular cerebral aneurysms. The most common risk factor is atherosclerosis, with other factors including infections, injuries, chronic inflammatory or autoimmune conditions like Behçet disease, giant cell arteritis, rheumatoid arthritis, Takayasu arteritis, systemic lupus erythematosus, ankylosing spondylitis, a bicuspid aortic valve or having previous aortic surgeries. They can also be associated with Turner syndrome, in addition to the conditions listed for cerebral aneurysms.
Risk Factors and Frequency for Saccular Aneurysm
Cerebral aneurysms affect around 3.2% to 4% of people, with most cases appearing between the ages of 30 to 60, equally affecting both genders. After the age of 50, they become more common in women, with a ratio nearing 2:1. Around 20% to 30% of people with cerebral aneurysms have multiple aneurysms. Every year, 6 to 16 out of every 100,000 people experience the rupture of a cerebral aneurysm, leading to 30,000 cases annually in the US alone.
Each year, unruptured cerebral aneurysms have a 1% to 2% chance of rupture. When rupture occurs, between 10% to 30% of people don’t make it to the hospital in time, and only about 30% recover well after appropriate treatment. Such ruptures account for 0.4% to 0.6% of all deaths. Without treatment, ruptured aneurysms risk 20% to 50% chance of rebleeding within the first two weeks. Cerebral aneurysms are rare in children. Most cerebral aneurysms, about 85%, are found in the anterior circulation on the circle of Willis and the middle cerebral artery bifurcation.
- The most common locations of cerebral aneurysms include:
- The junction of the anterior cerebral artery with the anterior communicating artery
- The junction of the internal carotid artery with the posterior communicating artery
- The bifurcation of the middle cerebral artery
In the lower part of the brain, the common sites often include the distal basilar bifurcation (basilar tip), the junction of the basilar artery and the cerebellar arteries, and the junction of the vertebral artery with the posterior inferior cerebellar artery.
In a study of 284 patients with 322 saccular aortic aneurysms, results showed:
- 68% were found in the thoracic aorta
- 24.2% in the abdominal aorta
- 7.1% in the arch of the aorta
- 0.6% in the ascending aorta
When studying aortic aneurysms, it was observed that 6% were saccular aneurysms while 94% were fusiform aneurysms. As saccular aortic aneurysms are less common than fusiform aneurysms, they’re usually included with all aortic aneurysms in most studies. Therefore, the actual number of saccular aortic aneurysms is not well known.
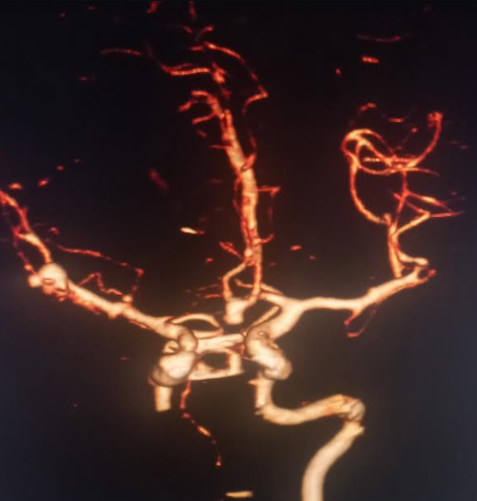
communicating artery and middle cerebral artery bifurcation are visualized.
Signs and Symptoms of Saccular Aneurysm
A cerebral aneurysm is a weak point in a brain blood vessel that can potentially burst. A lot of times, these don’t cause any symptoms and are discovered when a brain scan is done for other reasons. But if symptoms do occur, they could include headache, eye pain, seizures, vision problems, and in severe cases, loss of consciousness.
Indicators of an unruptured cerebral aneurysm may be:
- Headache
- Eye pain
- Seizures
- Visual loss
On the other hand, signs of a rupture include:
- Sudden, severe headache
- Nausea and vomiting
- Stiff neck
- Confusion
- Loss of consciousness
- Light sensitivity
An aortic aneurysm is a weak point in a primary blood vessel in the chest or abdomen. Most people have no symptoms until it becomes larger or ruptures.
The following symptoms can be seen with an unruptured aortic aneurysm:
- Chest pain or tenderness
- Neck pain
- Coughing
- Shortness of breath
- Dysphagia (difficulty swallowing)
- Abdominal pain
- Back pain
Should the aneurysm rupture, one might experience:
- Sudden and severe chest or abdominal pain
- Difficulty breathing
- Low blood pressure
- Paralysis or weakness of lower extremities
- Loss of consciousness
Different scales and classifications are used by doctors to predict the severity and outcome of these conditions, depending on the symptoms and the results of brain scans.
Testing for Saccular Aneurysm
A cerebral aneurysm is a bulging, weak spot in a blood vessel in the brain. Often, these aneurysms are found unexpectedly during head imaging. Those who are at high risk, such as people with a family history of brain aneurysms, may be specifically checked for this condition using imaging techniques like magnetic reasoning angiography, CT scans, or digital subtraction angiography. Thanks to the inflammation and the small, defensive cells found in an aneurysm, an MRI with a special dye can be used to spot aneurysms that are likely to burst.
Ferumoxytol is a small particle that gets picked up by defensive cells in the body and can be used as a special dye in MRIs to detect inflammation. A head CT scan without contrast is the first test for a suspected ruptured brain aneurysm causing SAH (a type of stroke caused by bleeding in the area surrounding the brain). This test can accurately detect the condition if it’s done within 6 hours of symptoms starting. However, it starts to become less effective over time, going down to 95% effectiveness at 12 hours, 92% at 24 hours, and 50% by one week. If an aneurysm is highly suspected but the CT scan is negative, a lumbar puncture can be done to measure the cerebrospinal fluid’s cell count and xanthochromia which are indicators of bleeding in the brain.
An aortic aneurysm, on the other hand, is a bulge that occurs in the main vessel that carries blood from your heart to your body. Like cerebral aneurysms, they are also typically discovered unexpectedly during imaging studies. A chest X-ray can often identify these aneurysms due to the signs of the aortic area causing changes in the surrounding structures. These aneurysms can also be unexpectedly found during heart imaging tests such as an echocardiogram, chest CT scan, or chest MRI.
If a patient is showing symptoms, CT scans or magnetic reasoning angiography are the best methods for viewing the aortic diameter and blood vessels and to identify a possible dissection or rupture. The choice between these options depends on the situation. CT scans are quicker and typically better for very symptomatic patients, while magnetic reasoning angiography can be better for repeated imaging due to the lack of radiation. It’s also best for viewing any aneurysms that involve the main part of the aorta closest to the heart. Also, an echocardiography can be used to measure the aortic sinus diameter, especially those patients with a bicuspid aortic valve, which is a heart valve with two leaflets instead of three.
Treatment Options for Saccular Aneurysm
When figuring out the best way to treat a cerebral aneurysm, factors such as the patient’s age, health condition, aneurysm size and location, symptoms, risk of rupture, and any previous brain hemorrhage (SAH) are taken into consideration. There are three main ways to manage cerebral aneurysms: observing the aneurysm, endovascular therapy, and surgery. In cases where the aneurysm has burst, surgical or endovascular therapy should be used.
Monitoring
If an unruptured aneurysm in the front part of the brain is discovered in a patient older than 64 with no symptoms and no history of brain hemorrhage, the doctor may choose to observe it with regular check-ups and scans. This is especially the case if the aneurysm is less than 7 mm in size. Studies have shown that these aneurysms have around a 1% chance of rupturing each year. Some doctors might use nonsteroidal anti-inflammatory drugs or COX-2 inhibitors to help prevent the aneurysm from growing larger.
Endovascular Embolization
This minimally invasive procedure involves inserting a catheter into the femoral artery and guiding it to the aneurysm. Then, small platinum coils are placed into the aneurysm to create a clot that blocks off the aneurysm and helps prevent rupture. This procedure is often performed under general anesthesia due to its safety and efficiency. It can be used for aneurysms that are hard to reach surgically. Today, doctors are also using flow diversion devices to reduce blood flow into the aneurysm, cause it to clot, and create a new lining at the neck. This basically stops blood from entering the aneurysm.
Surgical Clipping
This surgery involves creating a hole in the skull to access the aneurysm. After the aneurysm is isolated, a small metal clip is placed around its neck to block off the blood supply. Though this process is invasive, the risk of bleeding after surgery is low. However, this operation is associated with a higher risk of complications and death in comparison to endovascular coiling.
Patients whose cerebral aneurysm has ruptured should be monitored in an intensive care unit. Quick treatment to prevent further bleeding is important. Signs of neurological issues due to blood vessel spasm, bleeding, seizures, brain swelling, excess cerebrospinal fluid, or low sodium should be watched for. The key concern in the first 48 hours after a brain hemorrhage is further bleeding. Blood pressure maintenance and measures to reduce inflammation in the blood vessels are often implemented. Regular imaging tests are also conducted to look for remaining or recurring parts of the aneurysm that may need additional treatment.
Aortic Aneurysms
Treatment methods depend on the size, symptoms, and location of the aneurysm, as well as other health conditions. The likelihood of rupture is mainly determined by the aneurysm’s diameter.
Conservative Management
Patients with an aneurysm that is less than 45 mm and causes no symptoms are often managed with medicine and regular checkups. This approach also involves careful control of blood pressure and surveillance for conditions related to aortic aneurysms. Cardiovascular risk reduction measures and serial imaging to monitor changes in the aorta are also important aspects of this strategy. In most cases, beta-blockers are used to manage the blood pressure.
Repair Management
Any symptomatic unruptured or ruptured aortic aneurysms should be repaired. Deciding the exact diameter at which an asymptomatic aneurysm should be operated upon can be challenging, but a diameter of 45mm is typically seen as a safe point for elective surgery. For aneurysms due to genetic causes, even smaller diameters might warrant surgery. Aneurysms that expand by 5mm or more a year also should be repaired. Open surgical repair is usually required for aneurysms that involve the aortic arch, the ascending aorta, and the aortic root, whereas endovascular aneurysm repair is often the preferred approach for those with aneurysms in the descending aorta.
What else can Saccular Aneurysm be?
When we talk about brain (or cerebral) aneurysms, these are the medical conditions that might also be considered as they exhibit similar symptoms:
- Intracerebral hematoma
- Subdural hematoma
- Cerebral stroke
- Intracranial arterial dissection
- Mycotic aneurysm
- Arteriovenous malformations
- Cerebral amyloid angiopathy
- Reversible cerebral vasoconstriction syndrome
- Vasculitis
- Dural sinus thrombosis
- Cerebral venous thrombosis
Similarly, when considering aortic aneurysms, the following conditions may also be taken into account because they share similar symptoms:
- Aortic dissection
- Aortic pseudoaneurysm
- Senile ectasia
- Post-stenotic dilatation
- Acute myocardial infarction
- Pneumothorax
- Superior vena cava syndrome
- Pulmonary embolism
- Hypertensive emergency
- Mediastinal mass
- Lung mass abutting aorta
- Abdominal mass
- Mesenteric ischemia
- Diverticulitis
- Pyelonephritis
What to expect with Saccular Aneurysm
Small brain aneurysms that haven’t burst (less than 7 mm in size) carry a low risk of rupture. However, if a brain aneurysm does rupture, it can be very serious and life-threatening. The fatality rate from a ruptured aneurysm can vary between 25% to 50%, with almost half of surviving patients ending up with a permanent disability.
About one-third of patients can expect a good outcome with the right treatment. Brain aneurysms can also bleed into the brain, causing further damage. The consequences of a ruptured brain aneurysm greatly depend on the size and location of the bleed, the patient’s age, their neurological state when they arrive for treatment, the degree of blood vessel spasm, and other existing health conditions.
Similarly, while the yearly risk of rupture for an aortic aneurysm (a swelling in the main blood vessel in your body) is low when the size is under 45 mm, if it does rupture, it’s often fatal with about 50% of patients not even making it to the hospital. Those who do survive and undergo surgery face high risks of complications. Depending on the location and type of surgery, the overall death rate during or immediately after surgery can range from 2% to 17%, increasing to 25% if the aneurysm is located in the arc of the aorta.
The outcome greatly depends on when the surgery is performed, where the aneurysm is, the surgical method used, the surgeon’s experience, if the patient has other health conditions, and whether the aneurysm has ruptured.
Possible Complications When Diagnosed with Saccular Aneurysm
Cerebral Aneurysms
Cerebral aneurysms, also known as brain aneurysms, can have several complications:
- Cerebral aneurysm rupture: When the brain aneurysm breaks open
- Recurrent bleeding: Bleeding that happens again and again
- Vasospasm: A condition where blood vessels go into spasm, restricting blood flow
- Seizures: A sudden uncontrolled electrical disturbance in the brain
- Cerebral salt wasting: A condition that can lead to low salt levels
- Syndrome of inappropriate antidiuretic hormone secretion: A condition that causes your body to produce too much antidiuretic hormone
- Hydrocephalus: A buildup of fluid in the brain’s cavities
- Stunted myocardium and pulmonary edema: Conditions that can affect the heart and lungs
- Arrhythmias: Irregular heartbeats
- Gastrointestinal bleeding: Bleeding in the stomach or intestines
- Infections: Any kind of infection can become serious
- Deep venous thrombosis: Blood clots that form in deep veins, often in the leg
- Death: In the worst-case scenario, a cerebral aneurysm can be fatal
Aortic Aneurysms
Like cerebral aneurysms, aortic aneurysms also have many potential complications:
- Aortic aneurysm rupture: This happens when the aorta, the main artery in the body, bursts
- Acute myocardial infarction: Another term for a heart attack
- Aortic regurgitation: A condition where the aortic valve doesn’t close tightly, causing blood to leak backward into the heart
- Superior vena cava syndrome or thromboembolism: Conditions affecting the main vein that carries blood from the upper body to the heart or blood clots that move through your bloodstream
- Pneumonitis: Inflammation of lung tissue
- Heart failure: A condition where the heart can’t pump enough blood to meet the body’s needs
- Hemodiaphragm paralysis due to phrenic nerve compression: A condition that causes difficulty in breathing because of pressure on the nerve that controls the diaphragm
- Aortoesophageal fistula: An emergency condition that involves an abnormal connection between the aorta and the esophagus
- Death: Like cerebral aneurysms, aortic aneurysms can also be fatal in severe cases
Recovery from Saccular Aneurysm
For patients who have had treatment for a brain aneurysm, once they have left the hospital most are asked to undergo a comprehensive check-up. This includes testing their mental abilities, behavior, social interactions, physical health, speech, and job-related skills. If the patient has a habit of smoking or consuming alcohol, the healthcare provider will provide counseling to help them quit. For patients who have limited mobility, the healthcare provider will institute measures to prevent deep vein thrombosis. This is a condition where blood clots form in deep veins, generally in the legs. The doctor will also use regular imaging to either confirm that the aneurysm has been completely removed or to monitor the size of the aneurysm if it wasn’t fully treated.
An aortic aneurysm, on the other hand, is a problem with the main blood vessel in your body. After treatment, patients usually start a heart recovery program. They receive thorough follow-up care after leaving the hospital. This care includes controlling their blood pressure and taking steps to reduce their risk of heart disease. These steps can include dieting, exercising, and possibly medication.
Preventing Saccular Aneurysm
It’s important for patients to understand what cerebral (in the brain) and aortic (in the main artery from the heart) aneurysms are and the risks they carry. An aneurysm is a weak spot in a blood vessel that can swell up like a balloon. If it ruptures (bursts), it becomes a critical, life-threatening situation.
Unfortunately, between 10% and 30% of people with a cerebral aneurysm suffer a burst before they can reach the hospital, and only roughly 3 out of 10 fully recover after receiving proper medical care.
It’s essential to avoid smoking and excessive drinking as they can increase the chances of an aneurysm getting bigger or even bursting. Controlling high blood pressure is also recommended, as it’s one of the key causes of aneurysms and can make them worse or cause them to burst. It’s also beneficial to reduce any other risks related to heart diseases as part of overall care.












