What is Thoracic Duct Leak?
The thoracic duct is the largest duct in the lymphatic system, which is part of your immune system. Typically about the length of a ruler and 2 to 5 millimeters wide, it helps drain immune system fluid known as lymph from most parts of your body, with the exception of the right side of your chest, right side of your head and neck, and right arm. When this duct leaks, it can create a condition known as chylothorax, where lymph fluid collects in the space around the lungs.
Usually, the thoracic duct starts at a part near the spine called the second lumbar vertebra and goes up to where the left shoulder vein and left neck vein meet. Around 1.5 to 2 liters of lymph fluid pass through this duct daily. If there is a leak in this fluid transportation system, it can cause a significant health problem due to loss of precious lymph and can cause breathing difficulties as a secondary issue.
What Causes Thoracic Duct Leak?
Leaks in the thoracic duct, which is an important part of the body’s lymphatic system, can happen due to injury or for non-injury related reasons, but are more often caused by some sort of trauma.
A. There are two ways trauma can cause these leaks:
1. Surgical causes: Sometimes, an unintentional injury can occur while a doctor is performing procedures on parts of the body like the esophagus (the tube connecting the throat to the stomach), aorta (the main blood vessel in the body), pleura (the lining of the lungs), lung, or spine, among others. The thoracic duct can have different shapes and locations in different people, and therefore can get injured during these medical procedures.
2. Non-surgical causes: These leaks can also happen due to penetrating injuries (like a knife or bullet wound) or non-penetrating injuries (like a blunt force trauma) to the neck, chest, upper abdomen, and sometimes because of intense straining, forceful vomiting, or due to problems related to a vein in the chest known as the subclavian vein.
B. Non-trauma related causes can be due to cancerous or non-cancerous conditions:
1. Cancerous causes: Conditions like lymphomas (cancer of lymphatic system), primary lung cancers, tumours in the chest area, sarcomas (a type of cancer), and leukemia (blood cell cancer) can cause these leaks.
2. Non-cancerous causes: These leaks can also be a result of non-cancerous tumours, liver disease known as cirrhosis (scarring of the liver), a bulge in the aorta known as thoracic aortic aneurysm, conditions like amyloidosis (build-up of abnormal proteins), sarcoidosis (inflammation in different parts of the body), protein-losing enteropathy (a condition that results in loss of protein from the gut), tuberous sclerosis (a genetic disease causing non-cancerous tumours to grow in brain and other vital organs), and in developing countries, tuberculosis (a serious bacterial infection).
Among all these, surgical injuries and tumours are the most common causes for thoracic duct leaks.
Risk Factors and Frequency for Thoracic Duct Leak
Leaks in the thoracic duct, a significant vessel in the body, are most commonly seen after certain surgical procedures. About 3% to 6% of children who undergo heart surgeries experience this. Similarly, around 3% of patients with non-penetrating chest injuries, and approximately 1.3% of those with penetrating chest injuries, also show signs of thoracic duct leaks.
- Thoracic duct leaks are often seen after an esophagus-related surgery.
- Between 3% to 6% of kids having heart surgeries might experience this.
- Close to 3% of patients with blunt chest injuries have thoracic duct leaks.
- Approximately 1.3% of people with penetrating chest injuries show signs of this condition.
Signs and Symptoms of Thoracic Duct Leak
How quickly symptoms appear can differ depending on the cause. Problems resulting from injuries or surgeries often show up sooner than others.
Patients typically experience difficulty in breathing due to a condition called pleural effusion, which is a buildup of fluid between the layers of tissue that line the lungs and chest cavity. Also, if there is a slow, ongoing leakage of a fluid called chyle, it can lead to malnutrition and a higher risk for infections. This is often seen in non-injury-related causes like cancer. However, in situations involving surgery or injuries, symptoms may be immediate if the fluid loss is more than 500 ml per day.
Upon check-up, doctors may note reduced breath sounds and areas that sound dull when tapped. This dullness is due to the collection of lymph, a fluid that contains white blood cells that help to fight infections.
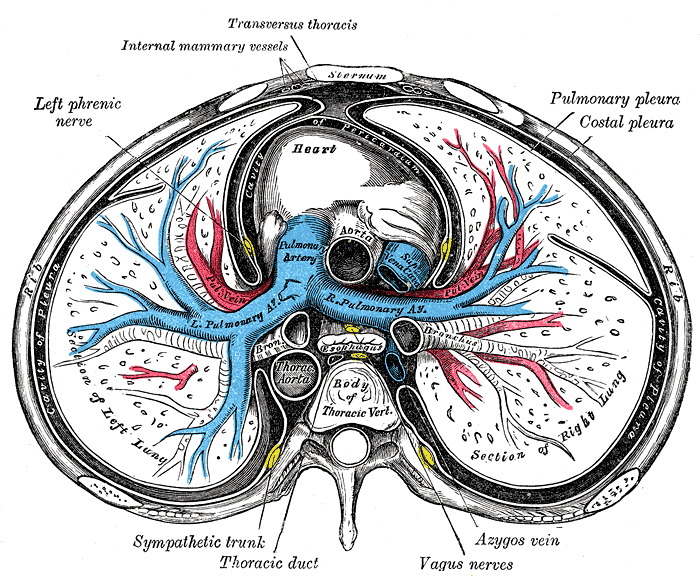
between the right and left lungs, heart, pulmonary pleura, costal pleura,
pleural cavity, ascending and thoracic aorta, pulmonary artery and its right and
left branches, superior vena cava, esophagus, main bronchi, azygos vein, vagus
nerves, thoracic duct, sympathetic trunk, left phrenic nerve, internal mammary
vessel, transversus thoracis muscle, rib, sternum, and thoracic vertebral body.
Testing for Thoracic Duct Leak
When your doctor suspects certain health problems, like issues with your lymphatic system, they might order various blood tests. These could include tests to check your glucose, total protein, triglycerides, albumin, and LDH (lactate dehydrogenase- an enzyme found in many body tissues). They are commonly done part of the routine process to understand your overall health better.
Your doctor might also want to use imaging technology to get a clearer picture of what’s going on in your body. One such tool is a chest X-ray, which can often reveal if you have an accumulation of fluid in your lungs (known as a pleural effusion). In the majority of patients, this fluid buildup tends to accumulate more commonly in the right part of the chest. The side where the fluid is collected can help your doctor understand where the possible damage is in your lymphatic system, an essential part of your immune function.
Doctors may be especially suspicious if the fluid in your lungs does not clear up or keeps coming back. The fluid might look cloudy or milky, although this appearance is not seen in every patient. Analyzing the fluid is an important part of the process. The fluid typically has a high number of white cells (lymphocytes) and properties similar to your blood plasma. If the triglyceride (a type of fat found in your blood) levels are over 110mg/dL and cholesterol is below 200mg/dL, it could be a sign of a condition called chylothorax, which involves lymph fluid leaking into your lungs.
To confirm chylothorax, another, more definitive but costly test is to look for chylomicrons (a type of particle that transports dietary fat and cholesterol through the lymph system to the blood) in your fluid. This test isn’t done routinely due to its cost and accessibility.
Once they have confirmed the presence of chylothorax, doctors usually want to find out what’s causing the fluid leak. This process might involve taking a CT scan of your chest and abdomen. If that doesn’t provide a clear answer, other tests, like lymphangiography (a dye test to visualize your lymphatic system) or lymphoscintigraphy (an imaging method that uses radioactive substances), could show the potential leak site or variations in your lymphatic system structure.
Recently, near-infrared fluorescence has gained attention as a noninvasive imaging method. This could potentially help doctors detect leaks more easily during surgery. However, it has not yet been used for a procedure called percutaneous sclerotherapy, which treats varicose veins by injecting them with a special solution, although, in the future, it could be helpful for this too.
Treatment Options for Thoracic Duct Leak
When dealing with a thoracic duct leak, that is, a leak in the main vessel that carries lymph fluid through the body, it’s important to not only address the leak itself but also understand what’s causing it. These leaks can release varying amounts of fluid. If the leak results in less than a liter of fluid, it’s considered a ‘low output’ leak, while leaks that result in more than a liter are regarded as ‘high output.’
For low output leaks, the main aim is to manage the symptoms by draining the fluid, working on diet control, and treating the underlying cause. A particular medication, Octreotide, might be used to help lower the number of leaks and avoid the need for surgery.
On the other hand, high output leaks usually occur after surgery. Initially, doctors try non-surgical treatment methods, but oftentimes, surgical intervention like tying off (ligation) or blocking off (embolization) the thoracic duct might become necessary.
In addition to these measures, doctors may also recommend a complete rest for the bowel, start parenteral nutrition (nourishment given through a vein), and prescribe medications like Octreotide/Somatostatin and Etilefrine for patients waiting for surgery. The exact timing of the surgery can vary, with some doctors recommending immediate post-operative intervention and others suggesting an initial wait of five days.
Still, in high-risk patients, non-surgical options, such as blocking or disrupting the thoracic duct, might be used. Due to their high success rate and fewer potential complications, these procedures have become a popular first-line treatment for managing chylothorax or accumulation of lymphatic fluid in the chest. The process generally involves accessing the thoracic duct via the abdomen and blocking off the feeding route using a specific liquid mix.
Thoracic duct embolization, or the process of blocking the duct, is usually a successful method with a success rate of around 70%. However, it can lead to after-surgery complications like chronic diarrhea, swelling in the lower extremities, or fluid build-up in the abdomen.
After lung removal surgery, patients with chylothorax are generally managed without draining the fluid from the chest, unless there’s evidence of shifting within the chest cavity, which might require a drain. After that, doctors will evaluate the need for tying off or blocking the thoracic duct. Also, thoracic fistulas, or abnormal connections involving the thoracic duct, are generally managed by directly suturing or tying off the thoracic duct, sometimes using additional agents like biological glues or substances that cause scarring.
If chylothorax is detected three weeks after surgery, visualization procedures are used to find and clip off the leak, which typically yield better results. The success of these non-surgical or conservative management methods will depend on the cause and the amount of fluid being drained, particularly in benign or non-threatening conditions like infection or a condition that causes inflammation in the body’s tissues, known as sarcoidosis.
In patients who are not suitable for surgery, pleurodesis could be an option. This is a procedure that involves introducing substances like talc or certain chemicals into the chest drain through a tube, causing inflammation that helps seal off the space to prevent fluid from accumulating. Pleurodesis can also be performed surgically, which is typically more effective than the non-surgical method.
Thoracic duct ligation and embolization, where the duct is tied off or blocked, are viable treatment methods. After duct ligation, evaluating the tissue under the microscope is generally advised to confirm the success of the procedure.
In situations where definitive procedures fail, a shunt (a tube that allows fluid to pass from one part of the body to another) or bypass of the terminal thoracic duct (the end part of the major lymph vessel in the body) may be required. This bypass is a new procedure which could improve and potentially cure the condition in patients suffering from thoracic leaks due to certain lymphatic abnormalities.
What else can Thoracic Duct Leak be?
When trying to diagnose a condition based on certain symptoms, doctors consider several possibilities. For instance:
- If a patient’s bodily fluid looks milky, it might be due to high cholesterol, an infection causing pus in the pleural space (empyema), feeding through a tube, or a lipid leak.
- If the fluid doesn’t look milky, it could indicate an excess of fluid caused by bacterial/tubercular or atypical pneumonia. Other possible causes include inflammation of the pancreas (pancreatitis), radiation therapy, a severe lung condition known as acute respiratory distress syndrome (ARDS), underactive thyroid (hypothyroidism), or Lupus pleuritis, which is a complication associated with Lupus, causing inflammation in the tissue that lines the lungs.
What to expect with Thoracic Duct Leak
Many patients get better with a careful and measured approach to their treatment, so their outlook is generally positive. However, those patients who have a severe disease or those who can’t control the leakage of chyle – a type of fluid in the body – often have a more negative outlook. In fact, nearly half of these patients face the risk of death if their chylothorax – a medical condition where chyle gathers in the space between the lungs and chest wall – is not treated.
Possible Complications When Diagnosed with Thoracic Duct Leak
Chylothorax complications are generally caused by a continuous loss of a fluid called “chyle”. This fluid contains significant amounts of fats, vitamins that dissolve in fat, proteins, electrolytes, and elements of the immune system like T-lymphocytes and immunoglobulins. The loss of these compounds may lead to weakened immunity and malnutrition.
Complications caused by Chylothorax includes:
- Loss of fats and fat-soluble vitamins
- Loss of proteins
- Loss of electrolytes
- Reduced immune system components
- Weakened immunity
- Malnutrition
Recovery from Thoracic Duct Leak
The treatment plan for a patient with a drainage tube in the space between the ribs (an intercostal drainage tube or ICD) or a long-term catheter involves proper care of the tube or catheter and accurately measuring the body fluid known as chyle that it drains.
It’s also important to replace any electrolytes (vital minerals that carry an electric charge in your body) that have been lost. This should be done alongside regular monitoring of factors in the blood, like lymphocyte (a type of white blood cell) counts, albumin (a protein in your blood), total protein, and the patient’s weight.
The patient is advised to follow a diet low in fat, which can either be taken orally or through a feeding tube (enteral).
Preventing Thoracic Duct Leak
If you have a low output thoracic duct leak (a condition where a tube in your chest that carries a type of fluid called lymph is leaking) and you’re being treated non-surgically, your doctor will give you precise dietary recommendations and will monitor your blood frequently. They’ll check things like electrolytes (substances needed for cells to function), your white blood cell count (to keep track of your immune response), and proteins (essential for your body functions). Good hygiene of your inserted chest drain (ICD) is also necessary to prevent infection.
An infection is possible in this situation, and if your doctor suspects this, they may request a computed tomography scan (used to create detailed images of your internal organs, bones, soft tissue, and blood vessels). It helps them get a more detailed look inside your body and plan further treatment.