What is Aortic Insufficiency (Aortic Regurgitation)?
Aortic regurgitation (AR), also known as aortic insufficiency, is a type of heart valve disease where the aortic valve doesn’t close properly. The aortic valve is normally made up of three wing-shaped parts that attach to the aortic wall. However, if these “wings” or the root of the aorta where they attach gets sick, it can lose its ability to function properly. In AR, blood flows backwards from the aorta into the left ventricle, which is a chamber in the heart, instead of flowing forwards throughout the body. This happens during the relaxed phase of the heart’s pump cycle. Chronic AR was first noticed in 1832 in patients with syphilis who also had a large aortic root. How AR shows up in patients depends on how quickly it comes on.
What Causes Aortic Insufficiency (Aortic Regurgitation)?
Aortic insufficiency is a condition that can occur due to problems related to the aortic valve leaflets, aortic root, annulus, or ascending aorta. Causes of acute aortic insufficiency can include bacterial heart infection, traumatic and non-traumatic rupture of the ascending aorta, balloon procedures to open a narrowed aortic valve, issues with a prosthetic valve, and leaks around a prosthetic valve. Certain medications, such as dopamine stimulators used to treat Parkinson’s disease (e.g., bromocriptine), can also sometimes lead to aortic insufficiency. These medications increase the stress on the aortic valve, which can cause scarring and further complications.
The causes of long-lasting or chronic aortic insufficiency can include a number of conditions. These range from rheumatic heart disease, which is the most common cause in developing countries, to various types of heart infections, congenital valve abnormalities, age-related aorta enlargement, hypertension, and even certain medicines. There are also certain diseases, such as osteogenesis imperfecta (a disorder causing brittle bones), Crohn’s disease (a type of inflammatory bowel disease), and Whipple’s disease (a severe infection) that can lead to chronic aortic insufficiency.
Certain autoimmune diseases that affect the whole body, such as lupus, rheumatoid arthritis, and Marfan’s syndrome (a genetic disorder that affects the body’s connective tissue), can also contribute to aortic insufficiency. There’s also a link between aortic insufficiency and Turner Syndrome, a genetic disorder affecting women that can cause a variety of medical and developmental problems. In a study with 253 patients with Turner Syndrome, more than half had some degree of aortic insufficiency.
Risk Factors and Frequency for Aortic Insufficiency (Aortic Regurgitation)
The Framingham Heart Study, which began in 1948, was designed to identify risk factors for heart disease. This research involved 5,209 men and women aged between 28 and 62. The study found that 4.9% of these individuals had aortic insufficiency, a heart condition, with 0.5% experiencing moderate or severe symptoms of this disease.
The occurrence and severity of aortic insufficiency tends to rise with age, most notably between the ages of 40 and 60. It affects 2% of people over the age of 70, and in a subsequent research called the Framingham offspring study, 13% of men and 8.5% of women were found to have the disease.
The prevalence of aortic insufficiency varies widely across the globe, largely due to the different health issues prevalent in industrialized and developing countries. For instance, in industrialized countries, the disease is often seen in older people, due to slow-progressing disease processes and other health conditions that increase their risk. In contrast, in developing countries, the condition often appears in younger individuals, with a sudden onset. Here, two of the main causes are rheumatic heart disease and infective endocarditis.
It is important to note that the frequency of this heart condition varies based on gender and geographic location.
Signs and Symptoms of Aortic Insufficiency (Aortic Regurgitation)
Acute aortic insufficiency is a condition where the aortic valve doesn’t close tightly, allowing some of the blood that was just pumped out of the heart to leak back into it. It can cause a variety of symptoms including coughing, palpitations, shortness of breath when exercising, and chest pain. Chronic aortic regurgitation, on the other hand, may not cause symptoms for a long time. However, when it does, these may include shortness of breath when lying down, palpitations, difficulty breathing at night, fainting, and chest pain.
For an accurate diagnosis, a thorough medical history and physical examination are required. During the exam, the doctor listens for certain sounds, like a diastolic murmur – a particular sound that blood makes as it flows through a leaking aortic valve. This sound can be more noticeable when the doctor asks the patient to squeeze their hand.
In acute cases, patients may look sick and have a fast heart rate and low blood pressure. They may also have a normal or slightly high pulse pressure and a normal heart rhythm. The same physical exam may show different results in chronic cases. These patients might have a wide pulse pressure and a shifting, pounding heart rhythm. They might also hear a special type of murmur, called an Austin Flint murmur.
There are some special signs doctors look for that might signal aortic insufficiency. However, these signs are not always present:
- Austin Flint murmur: This is a special murmur caused by the leaky aortic valve forcing the mitral valve (another heart valve) to close early.
- Pulsus bisferiens: This is a double pulse that can be seen when tracing the heart’s activity.
- Corrigan sign: This is a bounding, or very strong, pulse felt in large arteries, such as the carotid artery in the neck.
- De Musset sign: This involves the patient’s head nodding in time with their heartbeat.
- Muller sign: It is a pulsating uvula, observed during heartbeats.
- Quincke sign: Alternating reddening and paleness of the nail bed when pressure is applied.
- Traube sign: It is a peculiar pistol-shot sound heard over the femoral artery (in the thigh).
- Waterhammer Pulse: These pulses feel like they quickly fade away or are “bounding.” This can be felt more strongly by lifting the limbs.
Testing for Aortic Insufficiency (Aortic Regurgitation)
The 2017 guidelines from the American Society of Echocardiography classify aortic insufficiency, also known as aortic regurgitation, in a few different ways:
* Type 1 is when the valves of the aorta are working correctly, but there’s an issue with dilation, or widening, or a hole (perforation) in a leaflet of the valve. There are four subtypes of Type 1 aortic insufficiency, ranging from enlargement of different parts of the aorta to a perforation in the aortic cusp, which is a part of the valve.
* Type 2 is due to too much tissue in the valve leaflets or a disruption to the place where leaflets of a valve meet, leading to the leaflets of the aortic valve sagging or protruding.
* Type 3 is due to several factors that interfere with the motion of the aortic valves.
There’s also a system in place to classify chronic aortic insufficiency:
* Stage A includes patients who are at risk of developing the condition.
* Stage B describes people with mild to moderate progressive aortic insufficiency.
* Stage C represents those with severe aortic insufficiency who aren’t showing symptoms. Among this group, some people also might have issues with left ventricular dilation or a lower ejection fraction, which refers to how well the left ventricle is pumping blood out into the body.
* Stage D includes people with symptomatic and severe aortic insufficiency.
To identify aortic insufficiency, doctors can use a number of diagnostic tools. An electrocardiogram may show certain changes in heart activity, and a chest x-ray can provide signs of congestion in the lungs or widening of the area in the chest that contains the heart and other vital organs.
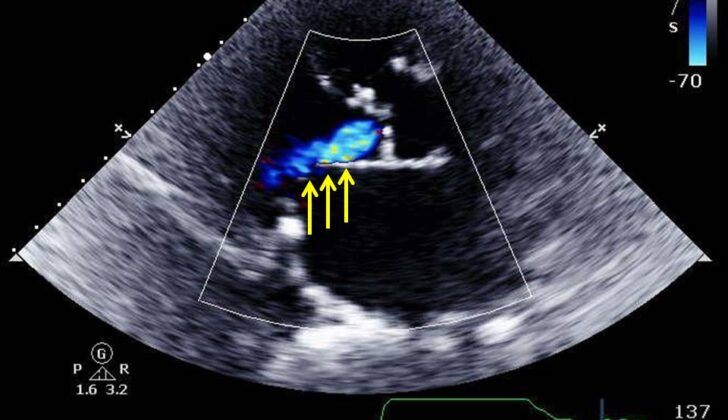
However, the best test to diagnose aortic insufficiency is typically echocardiography. This lets doctors visualize the aortic valves and other areas of the heart, helping them understand exactly what’s wrong. There are different ways to measure heart function using echocardiography, including looking at the direction and speed of blood flow in certain parts of the heart.
If a person is thought to have aortic insufficiency but isn’t showing symptoms, doctors may recommend exercise stress testing to monitor heart activity during physical effort. Other imaging techniques, like CT scans, MRI, and cardiac catheterization, can also be helpful in certain circumstances. These can give doctors a close look at the structure of the aorta and the heart’s pumping action – helping to determine the severity of the condition.
Treatment Options for Aortic Insufficiency (Aortic Regurgitation)
For acute aortic insufficiency, high blood pressure can be controlled with certain medications, such as angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or calcium channel blockers. Beta-blockers, typically recommended for managing aortic dissection, are not recommended for patients with severe aortic insufficiency, as they can cause increases in the time the heart takes to fill with blood and allow more blood to flow back into the heart. Antibiotics may be necessary for treating heart valve infections, and they should be chosen based on the specific pathogens found in blood cultures. In severe cases, such as infections, aortic dissection, or trauma, patients may require immediate surgery.
For chronic aortic insufficiency, the type of medical therapy used depends on the stage of the condition. Common treatments include angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or calcium channel blockers. Patients in specific stages of the disease with certain symptoms and reduced heart function may be given beta-blockers if they can’t have surgery due to other health conditions.
Based on health guidelines from 2014, aortic valve replacement (AVR) is usually recommended for various stages and conditions of aortic insufficiency. This replacement is not advised if certain levels such as the amount of blood pumped out by the heart and the size of the ventricle exceed defined limits, due to poor outcomes after surgery. In these cases, the patient is watched carefully with periodic check-ups.
In some cases, aortic valve repair may be a preferred option. This technique aims to preserve the existing valve. Some studies have reported good long-term survival rates and low occurrence of repeat operations after aortic valve repair – although, in some cases, the number of repeat operations were higher than for those who underwent AVR. Therefore, additional studies are needed to confirm the effectiveness and safety of aortic valve repair.
One study examining transcatheter aortic valve replacement (TAVR) and aortic valve repair has shown that the underlying causes and disease mechanisms affect decision making on the type of surgical interventions considered for different patients with AR.
What else can Aortic Insufficiency (Aortic Regurgitation) be?
When diagnosing aortic insufficiency, sometimes known as a leaky aortic valve, it’s important to consider other medical conditions that might be confused with it. For example, the lack of proper functioning of the aortic valve has been mistaken for serious infections, lung infections, or non-valve-related heart problems in the past.
Moreover, the diagnosis becomes more complex when aortic insufficiency coexists with other medical conditions. For instance, the backward flow of blood, a characteristic symptom of aortic insufficiency, can also result in heart failure or could be a result of a tear in the aorta wall. So, it is essential to recognize these conditions as they can affect treatment decisions.
Another condition that might be mistaken for aortic insufficiency is pulmonary regurgitation, a condition where the blood flows backward into the heart from the lungs. Both these conditions can produce a similar sound – known as a diastolic murmur – which can be heard through a stethoscope. However, doctors can distinguish between the two based on how the sound changes with breathing. Aortic insufficiency’s sound gets louder when you breathe out, while the sound of pulmonary regurgitation, especially in a patient with lung-related high blood pressure, amplifies when you breathe in.
Finally, heart conditions like coronary heart disease which can lead to a heart attack or heart failure should also be considered during the diagnosis. These conditions are, however, related to the heart muscle and vessels rather than the valves themselves.
What to expect with Aortic Insufficiency (Aortic Regurgitation)
The future health condition of a patient with aortic insufficiency largely depends on when symptoms began and how far the disease has progressed. If the patient doesn’t show any symptoms of aortic regurgitation, the outlook is generally good, unless the disease worsens suddenly.
Patients with serious aortic regurgitation but who maintain good heart pump function and quickly have their aortic valve replaced usually have positive long-term health outcomes. However, these patients must be closely monitored after valve replacement to see if more procedures are needed or if they develop heart failure or other issues.
On the other hand, patients who experience a decline in heart pump function and worsening symptoms have a less optimistic forecast. Under current guidelines, these patients are usually considered unfit for aortic valve replacement surgery which affects their prognosis negatively.
Possible Complications When Diagnosed with Aortic Insufficiency (Aortic Regurgitation)
Health professionals need to be cautious about a variety of complications that can arise when treating aortic insufficiency. Currently, surgery is the best method to fix aortic insufficiency, and the use of Transcatheter Aortic Valve Replacement (TAVR) is affecting the results after surgery. Initially, TAVR wasn’t recommended for pure native aortic insufficiency because of the lack of aortic valve hardening and the challenges with fixing the implanted valves in place.
A 2017 large-scale study of 331 patients with aortic insufficiency evaluated the use of TAVR. It found that TAVR is linked to many procedure-related complications. Additionally, the need for traditional surgery after the procedure, blockage of heart arteries, injury to the area around the aortic valve, and requirement for a permanent pacemaker were reported in patients using the newer models.
The other reported problems overall included:
- Continued aortic insufficiency after the procedure
- Need for a second operation
- Need for a second valve replacement
- Stroke
- Severe or life-threatening bleeding
- Major complications related to blood vessels
- Acute kidney injury
While the study showed some improvements when using TAVR to treat pure native aortic insufficiency, more research is needed to see if further improvements are possible. This would justify including TAVR in current guidelines.
Preventing Aortic Insufficiency (Aortic Regurgitation)
It’s important for patients to understand the symptoms that may be associated with their aortic regurgitation, a condition where the heart’s aortic valve doesn’t close tightly. For those who haven’t had surgery, they should regularly check for changes in their heart’s function with a monitoring tool called echocardiogram, the frequency of which depends on how severe their condition is. For those with a mild condition, they’ll need an echocardiogram every three to five years. If the condition is moderate, they’ll need an echocardiogram every one to two years. If the condition is severe, they’ll need an echocardiogram every six to twelve months or more often if their heart keeps getting larger. After surgery, patients are usually asked to return after six weeks to three months for an echocardiogram to check how well their heart is functioning.