What is Aortic Valve Endocarditis Surgical Treatment?
Infective endocarditis is a kind of infection that affects the inner lining of the heart, known as the endocardium. Depending on when the symptoms start and how long they last, this disease can be categorized as acute, subacute, or chronic. The most often affected areas are the heart valves, and in rare cases, the disease can impact other parts of the endocardium.
In recent times, we have seen an increase in the number of cases in the United States and worldwide. This trend has also seen a shift in the primary cause of the disease in the developed world, which is now mainly due to a bacterium called Staphylococcus aureus. Despite modern treatments, the death rate is still worryingly high.
There are some cases where patients can’t respond to the usual treatment or complications arise. For such cases, surgery might be needed. It’s crucial to identify these factors early on.
What Causes Aortic Valve Endocarditis Surgical Treatment?
Infective endocarditis, an infection of the heart’s valves, is usually caused by bacteria called S. viridans and S. aureus. If you have an artificial heart valve and you get this infection within the first two months, it’s likely to be caused by certain types of staph bacteria or S. aureus. But if this infection happens more than a year after you’ve had your artificial valve fitted, it’s usually caused by the same bacteria that affect natural heart valves.
In cases of severe, sudden bacterial endocarditis, you can often blame S. aureus. However, if the infection is less severe and develops over a longer period, S. mutans is the usual culprit. If you use drugs intravenously, have a weakened immune system, or have an artificial heart valve, you could be at risk for a yeast infection of the heart’s valves, usually caused by a type of yeast called candida.
Certain actions or conditions can put you at risk for different types of infective endocarditis. For instance, if you’ve recently had a gastrointestinal or urinary procedure, you’re more likely to get the infection from S. bovis or enterococci. Not taking care of your teeth increases your risk for a type of infective endocarditis caused by a group of bacteria called HACEK or streptococci. Being in a hospital puts you at risk for a type of the infection caused by S. aureus, certain kinds of gram-negative bacteria, or candida (the yeast).
Risk Factors and Frequency for Aortic Valve Endocarditis Surgical Treatment
Research shows that the main cause of infectious endocarditis, a serious heart infection, and its patient profile, have changed around the world. In developed countries, the infection is most commonly caused by a bacteria named Staphylococcus aureus. Patients with this condition are generally older than in the past, and many have artificial heart valves. Additionally, there are more surgeries being performed for this condition than before. There’s also been a rise in this infection following certain types of heart procedures, including less invasive aortic valve surgeries and a procedure known as percutaneous transcatheter aortic valve replacement.
- Infectious endocarditis, a heart infection, is now mostly caused by a bacteria called Staphylococcus aureus in developed countries.
- Patients affected by this condition are generally older now.
- Many of these patients have artificial heart valves.
- More surgeries are being performed for this infection today.
- There’s been a rise in this infection following some heart procedures, especially minimally invasive aortic valve surgery or percutaneous transcatheter aortic valve replacement.
Signs and Symptoms of Aortic Valve Endocarditis Surgical Treatment
Infections in the inner lining of the heart, also known as endocarditis, can cause a variety of symptoms and physical signs.
Symptoms can often include:
- Fever
- Loss of appetite
- Weight loss
- The feeling of being unwell or lethargic (malaise)
- Night sweats
During a check-up, doctors may find:
- A heart murmur
- Small, red or purple spots on the skin, eyes, or inside the mouth (petechiae)
- Enlarged spleen (splenomegaly)
Additionally, there may be other signs that can be found on the hands and feet:
- Thin red lines under the nails (splinter hemorrhages)
- Tiny bumps on finger or toe pads (Osler nodes)
- Small, painless red or bluish spots (Janeway lesions)
Testing for Aortic Valve Endocarditis Surgical Treatment
Infective endocarditis, or IE, is an infection of the heart valves. Doctors use a system called The Modified Duke Criteria to classify IE. They use it to evaluate patients who they think might have this condition. This system has three categories: “definite”, “possible”, or “rejected” IE.
“Definite” IE is split into subcategories:
1. “Definite” IE by pathological criteria: This means there are signs of bacteria on tissues of an abscess or vegetation (clumps of bacteria, cells, and clotting proteins). These findings must be from a sample that was removed from the body.
2. “Definite” IE by clinical criteria: This is decided based on a combination of major and minor criteria from The Modified Duke Criteria. This can be two major criteria, one major plus three minor criteria, or five minor criteria.
Major clinical symptoms include more than one positive blood test for bacteria, a positive culture for a specific bacteria called Coxiella burnetti, or evidence of endocardial involvement, which might be new heart valve issues or the presence of vegetation, an abscess or dehiscence (a surgical wound that has re-opened).
Minor criteria include:
a) A heart condition that increases the risk of IE or the use of intravenous drugs.
b) Fever of more than 38°C (over 100.4°F).
c) Certain vascular events like blood clots, lung infection, aneurysms, brain hemorrhage, or specific skin and eye symptoms.
d) Immune reactions, including Osler nodes, Roth spots, and the presence of rheumatoid factor.
e) A positive blood culture that does not meet the major criteria.
“Possible” IE means there is one major criterion and one minor criterion or three minor criteria present. “Rejected” IE means there may be another reason for the symptoms, or there is no evidence of IE after less than four days of antibiotic treatment, or the symptoms have improved after less than four days of antibiotics.
Doctors use an echocardiogram, which is like an ultrasound for the heart, to look for IE. This examination can show up lumps of bacteria or cells, called vegetation, on heart valves or nearby structures. It can also reveal abscesses, or the partial separation of a prosthetic valve, which are hallmarks of IE.
A kind of echocardiogram, called a transthoracic echocardiogram, should be backed up with a second kind, called a transesophageal echocardiogram, if doctors think a patient might have IE. Sometimes, doctors can’t be sure if a patient has IE until the patient has surgery, at which point doctors can take tissue samples for further analysis.
Treatment Options for Aortic Valve Endocarditis Surgical Treatment
In order to treat infective endocarditis, a condition that causes inflammation of the heart’s inner lining, long-term antibiotic treatment is often needed. The type of antibiotics used, and how long they’re used for, depends on factors such as the type of bacteria causing the infection and whether the patient has a natural or artificial heart valve. Treatment can last from 2 weeks to 6 weeks, starting in a hospital and continuing at home if the patient’s fever has gone down and blood tests show no signs of the infection. However, sometimes antibiotics alone aren’t enough, and surgery may be necessary.
One reason for surgery could be if the disease is causing heart failure, due to the heart valves not working properly. Other reasons could be infection caused by very resistant bacteria, electrical signal problems in the heart, an abscess, or a persistent infection after a week of antibiotic treatment.
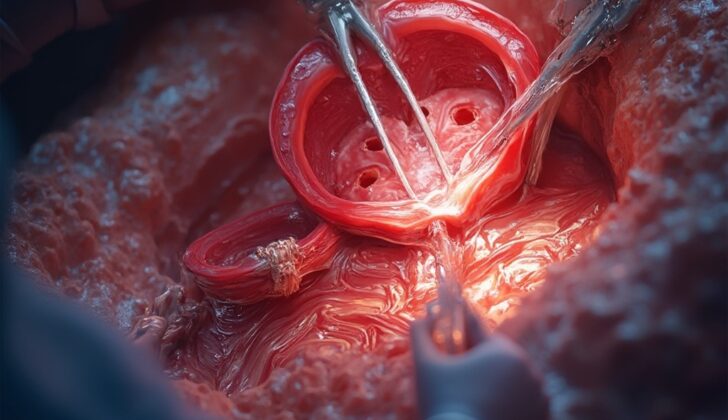
The main idea when performing surgery for infective endocarditis is to thoroughly clean the infected area by removing any infected or dead tissue, then rebuild the damaged parts. An imaging technique called Transesophageal echocardiography is often used during the operation. In most cases, the surgery involves making an incision down the middle of the chest. If the patient’s natural heart valve is infected, it is cleaned and then either repaired or replaced. The type of replacement valve (mechanical or biological) depends on several factors, although it’s strongly recommended not to use a mechanical valve if the patient has suffered a major stroke or brain bleed.
If the infection has severely damaged the heart’s aortic valve, it may need to be completely removed. The resulting gap is then fixed before a replacement valve can be installed. Depending on the size of the gap, either a small patch (of the patient’s own tissue or cow tissue) or a larger synthetic patch might be needed. If the damage is really extensive, it might be necessary to use a donated aortic valve. If an abscess has caused extensive damage to the aortic root (the bottom part of the aorta, the body’s main artery), it may need to be completely replaced. In these tricky cases, using a donated aortic valve is often the best choice.
If a patient’s artificial heart valve gets infected but the part around it is still healthy, the infected valve can simply be replaced. However, if the infection has spread to the aortic root, reconstruction followed by the use of a donated valve or a biological tissue root is a better option.
What else can Aortic Valve Endocarditis Surgical Treatment be?
Nonbacterial thrombotic endocarditis, formerly known as marantic endocarditis, is a condition where tiny clumps or “vegetations” that are not caused by bacteria, form on the heart valve leaflets. It’s more common in people with certain forms of cancer and conditions that cause the blood to clot too much. Libman–Sacks endocarditis is a similar condition where wart-like clumps form, but it’s often seen in people with systemic lupus erythematosus, a disease where the body’s immune system mistakenly attacks healthy tissue.
What to expect with Aortic Valve Endocarditis Surgical Treatment
The hospital death rate for patients with infectious endocarditis, a severe infection of the heart’s inner lining, is roughly 20%, while the death rate within six months of diagnosis is around 30%. This confirms that infectious endocarditis is a potentially deadly disease.
The chances of dying are influenced by various factors such as, the type of organism causing the infection, with higher death rates associated with infections due to S. aureus, P. aeruginosa, Enterobacteriaceae, or fungi. The presence of other health conditions or complications also plays a key role. These include old age, needing dialysis treatment for kidney failure, having an artificial heart valve, severe heart failure, stroke, abscess formation, severe suppression of the immune system due to HIV infection, and the spread of the infection to the areas around the heart valves or the formation of abscesses in the heart muscle.
Interestingly, people who inject drugs, and develop infectious endocarditis on the right side of their heart, have a lower death rate of around 10%. However, despite advances in medical technology and care, the death rate from infectious endocarditis has not decreased. This is due to a range of factors including, elderly patients living longer with multiple health conditions, more hospital-acquired infections in developed countries, and the increasing number of antibiotic-resistant germs.
Possible Complications When Diagnosed with Aortic Valve Endocarditis Surgical Treatment
Heart problems are a common complication of infections; these include conditions like congestive heart failure resulting from damaged heart valves due to infection. Other potential heart issues include abscesses around the heart, infections that disturb the normal electrical rhythm of the heart causing irregular heartbeats, bulging weak spots in the wall of the aorta within the heart that can lead to heart inflammation, blood filling the area around the heart, pressure on the heart due to excess fluid around it and abnormal passages into the heart chambers like the right or left ventricle.
Complications relating to the nervous system can happen too. These could involve blockages or clots in blood vessels, bulbous pouches appearing on brain arteries due to the spread of the infection – these pouches could potentially burst leading to internal bleeding in the brain and sudden death. Furthermore, the infection can spread throughout the body, affecting various vital organs like the liver, lungs, kidneys, and spleen.
- Congestive heart failure due to infected and damaged heart valves
- Abscesses around the heart
- Infections disrupting heart’s electrical rhythm, causing irregular heartbeats
- Bulging weak spots in the wall of the aorta within the heart (mycotic aneurysms of the sinus of Valsalva) leading to inflammation of the heart sac (pericarditis)
- Blood filling the area around the heart (hemopericardium)
- Pressure on the heart due to excess fluid around it (Cardiac tamponade)
- Abnormal passageways into heart chambers like the right or left ventricle (fistulas)
- Blockages or clots in blood vessels (thromboembolic events)
- Bulbous pouches on brain arteries due to infection spread (mycotic aneurysms) which can burst causing brain bleed
- Infection spread to vital organs, impacting the liver, lungs, kidneys, and spleen (systemic embolism).
Preventing Aortic Valve Endocarditis Surgical Treatment
It is crucial to spot and diagnose infective endocarditis, a heart infection, early so that treatment can begin on time, resulting in the best possible health outcomes. It’s also important to identify patients who might benefit from surgery early on. Early surgical treatment is linked to a lower risk of death.