What is Atrial Flutter?
Supraventricular arrhythmias are a variety of irregular heartbeats that start in the upper chambers of the heart, known as the atria. The most common types include atrial fibrillation and atrial flutter, while other less common ones include certain types of fast heartbeats, like atrial and atrioventricular tachycardias. This summary specifically focuses on atrial flutter.
Atrial flutter is among the most frequent irregular heart rhythms and is marked by a rapid and abnormal heartbeat, which can reach 300 beats per minute. It may lead to symptoms like heart palpitations, fatigue, fainting spells, and in some cases, the formation of blood clots.
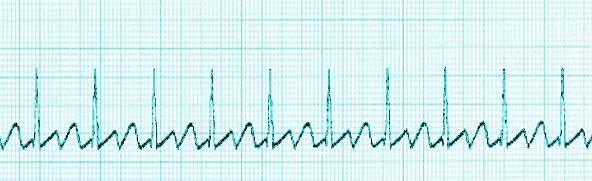
Furthermore, atrial flutter is classified as a macro-reentrant tachycardia, meaning the irregular heartbeat involves a large circuit looping around the heart. It can be “typical” or “atypical” based on where it originates in the heart. Medical professionals can identify these types by looking at heart activity on an electrocardiogram or EKG.
The most common type, known as “typical” or cavotricuspid isthmus (CTI) dependent atrial flutter, starts in the right upper chamber of the heart near the tricuspid valve. This is visible on the EKG as a specific pattern of waveforms. The mechanisms behind this particular irregular heartbeat will be further explained in a later section.
“Atypical” atrial flutter, on the other hand, isn’t dependent on the CTI and can originate from either the right or left upper chambers. In some less common cases, the electrical activation of the heart can proceed in a clockwise direction, changing the appearance on the EKG and making it harder to distinguish from other types of atrial flutter.
What Causes Atrial Flutter?
Atrial flutter, a kind of rapid heartbeat, is caused by a sort of loop, or ‘re-entry mechanism’, in our heart’s electrical system.
For this loop to occur, several factors must be present:
1. Areas in the heart where electrical signals travel at different speeds
2. Parts of the heart having diverse ‘refractory periods’, or rest times, between beats
3. A specific zone where this circuit or loop occurs
These conditions often occur in a common type of atrial flutter in an area of the heart known as the CTI. The start of atrial flutter is triggered by an irregular beat that activates one part of the loop’s pathway that has just finished its rest time, and initiates the fast heartbeat from a part that is ready for action.
Risk Factors and Frequency for Atrial Flutter
Atrial flutter is a type of irregular heartbeat or cardiac arrhythmia. It is the second most common kind of arrhythmia after a condition called atrial fibrillation.
It can often coincide with atrial fibrillation, though we do not fully understand how often this happens compared to atrial fibrillation alone.
Atrial flutter is usually seen in patients who have diseases such as chronic obstructive pulmonary disease, pulmonary hypertension (high blood pressure in the lungs), and heart failure. However, having atrial flutter without any heart abnormalities is rare. It usually occurs when there are irregularities in the size of the atria (upper chambers of the heart).
Atrial flutter is more common in males than in females, with old age being a significant risk factor. People with atrial flutter may often have other health problems, such as high blood pressure, diabetes, and a history of alcohol abuse. Increasing age also raises the risk of developing both atrial flutter and atrial fibrillation.
Signs and Symptoms of Atrial Flutter
Atrial flutter is a heart condition that can cause a variety of symptoms. Some people may not notice any symptoms at all, while others may feel palpitations, or a rapid, fluttering heartbeat. You might also feel lightheaded, tired, or short of breath, especially if your heartbeat is very fast. Being unable to exercise as much as usual can be another sign of atrial flutter.
More severe symptoms can occur in some cases. If your heart rate gets too high, you might experience low blood pressure, fainting, or near-fainting. Others might not have any symptoms until they develop serious complications. These could include suddenly worsened heart failure, heart damage caused by sustained rapid heartbeat, or a stroke triggered by a clot that travels from the heart to the brain.
When a doctor examines somebody with atrial flutter, they might find a few key physical signs. These can include a pulse that feels consistently fast or irregularly paced, visible swelling in the neck veins, crackling sounds in the lungs when breathing, a rapid heartbeat, a swollen abdomen, and swelling in the lower legs when fluid builds up in the body.
- Feeling of a fast, fluttering heartbeat
- Lightheadedness
- Fatigue
- Shortness of breath
- Decreased ability to exercise
- Low blood pressure, fainting, or near-fainting (in severe cases)
- Fast or irregular pulse
- Swelling in the neck veins
- Crackling lung sounds
- Rapid heartbeat
- Abdominal swelling
- Swelling in the lower legs
Testing for Atrial Flutter
The first step in diagnosis is understanding the root rhythm of the heart, and figuring out what might be causing it.
Electrocardiogram: An electrocardiogram is a test that measures the electrical activity of your heart. In cases of atrial flutter, this test might show what look like flutter waves with no flatlines between heartbeat signals, and a much faster than normal atrial wave of about 300 beats per minute. They could observe variable heartbeat patterns due to something called the Wenckebach phenomenon.
On this test, typical flutter waves might look kind of like a picket fence or the teeth of a saw because of the negative P waves caused by the direction of the vector. If the activation of heartbeats is going counterclockwise, this test might show negative flutter waves with low amplitude in lead I and upright flutter wave in aVL.
Echocardiogram: An echocardiogram is another test, which is used to evaluate the structure of your heart. It can help in understanding if there’s any heart disease. If they see that the chambers of your heart are enlarged, it’s a sign that this condition has been present for a long time and might be hard to control because of fibrosis (an excess of connective tissue).
Evaluation of the ejection fraction from your left ventricle (a measure of how well your heart is pumping) can either be a cause or a result of atrial flutter. Long-term fast heart beats can cause something called tachycardia-induced cardiomyopathy, or this cardiomyopathy and your volume status can trigger the atrial flutter.
It’s also important to look for clots in the heart, particularly if converting your heart back into its regular rhythm is desired. A transesophageal echocardiogram is the preferred choice for this as it can clearly visualise the atrial appendage where clots are most likely to be present.
Laboratory evaluation: It’s necessary to figure out what’s causing the atrial flutter. Tests might include checking your electrolyte levels, thyroid function, whether you have an infection or anemia, and whether there’s a lack of oxygen. By correcting these issues, it can help to alleviate symptoms and reduce the development of atrial flutter and rapid heartbeats.
Sometimes a pulmonary function test might be done. There’s a relationship between lung disease and the presence of certain heart rhythms, including atrial flutter, so treating any underlying lung conditions can help manage the atrial flutter.
Treatment Options for Atrial Flutter
Treatment for atrial flutter focuses on three main aspects:
1. Controlling the rhythm
2. Controlling the rate
3. Taking blood-thinning medications to reduce the risk of blood clots
1. Rhythm control:
Atrial flutter can cause structural changes to the heart over time, making it harder to control the heart rate or convert the heart rhythm back to normal. Different methods can be used to restore the heart’s normal rhythm. These include electrical cardioversion, medication, and catheter ablation.
If a patient with atrial flutter is unstable or experiencing severe symptoms, a procedure called synchronized cardioversion is used to immediately stabilize their heart rhythm. For patients who are stable, medication can be used to restore a normal heart rhythm.
Medications like amiodarone, procainamide, quinidine, disopyramide, flecainide, propafenone, verapamil, diltiazem, metoprolol, carvedilol, and esmolol can help convert the heart rhythm back to normal. However, these medications aren’t always successful and work by preventing early heartbeats that can start abnormal heart activity.
Patients newly diagnosed with atrial flutter should be started on blood-thinners. If no blood clots are seen in the heart, it may be appropriate to consider cardioversion, especially to prevent the worsening of heart changes. Patients who can’t tolerate the medications, or in whom the medications are contraindicated, may require a procedure called catheter ablation which electrically disconnects the area causing the abnormal rhythm.
2. Rate control:
Medications that slow down the passage of electrical signals through the heart, such as calcium channel blockers or beta blockers, can help control heart rate. Digoxin can also be used, but with caution due to its possible side effects. A combination of these medications may be necessary for some patients.
Adequate heart rate control can be difficult because atrial flutter continuously sends out fast signals to the heart’s natural pacemaker, the AV node. The goal should be a heart rate below 110 beats per minute to reduce complications.
For those who can’t tolerate medications or have a slowly beating heart due to the rate control measures, a catheter ablation may be necessary.
3. Blood-thinning medications:
People with atrial flutter have a similar risk of having a stroke to those with atrial fibrillation. A scoring system called CHADS2-Vasc can be used to determine the annual risk of stroke. It includes factors like heart failure, high blood pressure, diabetes, gender, age, and history of vascular disease or stroke. People with higher scores have a higher risk of stroke and should take blood thinners. Even people with lower scores may benefit from taking aspirin or blood thinners.
What else can Atrial Flutter be?
When trying to diagnose certain heart conditions, doctors look at specific signs during a heart activity test (electrocardiogram):
1. Atrial fibrillation: This condition is usually marked by irregular activity where the heart’s upper chambers (the atria) are not working in an organized way. This could be seen in the test as an absence of something called P waves.
2. Multifocal atrial tachycardia: Here the heart has multiple factors controlling its rhythm or ‘pacemakers’ in the atria. This condition can be identified with multiple P waves present in the test results due to these several ‘governing’ points.
3. Atrial tachycardia with variable conduction: This is a condition where the heart beats faster than normal. In the test, this condition can be noticed by an uninterrupted line (isoelectric line) between the heart’s main electrical signals (QRS complexes).
Understanding these signs can help doctors diagnose these conditions correctly and suggest appropriate treatments.
What to expect with Atrial Flutter
The future outlook for patients with a common type of abnormal heart rhythm, called atrial flutter, who undergo a procedure known as catheter ablation, is generally positive. These patients have less than a 5% chance of the problem coming back.
If atrial flutter continues without treatment, it can lead to a condition known as tachycardia-induced cardiomyopathy. This is a type of heart disease that is difficult to manage and may result in frequent hospital admissions due to worsening of the patient’s condition.
Possible Complications When Diagnosed with Atrial Flutter
The primary risk of atrial flutter, a heart condition, is of having a stroke. If the stroke is serious enough, it could cause lasting, or “embolic,” disability.
Another complication is “hemodynamically instability,” which can happen if the heart starts beating too quick—what doctors call a “rapid ventricular response.”
If atrial flutter is ongoing and not controlled properly, it can cause a condition called “tachycardia-induced cardiomyopathy.” This condition weakens your heart muscle and can lead to heart failure, making it hard to control.
Complications can also come from the medications doctors use to treat atrial flutter. These depend on the specific type of drug and how that drug works.
Finally, complications can also occur from a treatment called “atrial flutter ablation,” which is when doctors use heat to destroy the areas of your heart causing the atrial flutter. In this procedure, there are fewer complications if the atrial flutter originates from the right side of the heart rather than the left. This is because to treat left-sided atrial flutter, doctors have to make a hole (“transeptal communication”) to get to the left side of your heart. This process can increase your risk of strokes compared to right-sided procedures.
Potential complications include:
- Stroke leading to disability
- Instability in the manner your heart beats
- Tachycardia-induced cardiomyopathy leading to heart failure
- Complications related to the use of heart rhythm-controlling drugs
- Complications related to the atrial flutter ablation procedure, especially if the flutter is on the left side