What is Atrioventricular Block?
The cardiac conduction system, composed of special fibres, sparks and transmits electric pulses through the heart. The sinus node, which is the main pacemaker of the human heart, sends out a pulse to trigger a contraction of the heart’s chambers, known as the atria and ventricles. On an electrocardiogram (ECG), which records the heart’s electrical activity, the initial heart contraction is indicated by the P wave. The contraction wave then moves from the atria to the ventricles via a pathway called the atrioventricular (AV) conduction system, represented by the QRS segment on an ECG.
The AV conduction system, which is part of the heart’s electrical system, is made up of an AV node and specialized conduction fibers known as the His-Purkinje system. It’s controlled by the autonomic nervous system, which can change its pace depending on the body’s needs. The functioning of the AV conduction system can be assessed through the relationship between the ECG’s P waves and QRS complexes. Normally, the time interval between a P wave and the QRS complex is fixed at 120 to 200 milliseconds.
A delay or disturbance in the transmission of a pulse from the atria to the ventricles is known as an AV block. This can happen due to problems, either physical or functional, in the heart’s electrical system. An AV block could be temporary or permanent, and it’s classified into three types, depending on its severity: first-degree, second-degree, and third-degree. Furthermore, an AV block can be identified as being above the node (supra) or within or below the node (infra-His). Those that are below the node usually present with a wider QRS complex, can advance to a third-degree AV block, and often require the use of a pacemaker.
What Causes Atrioventricular Block?
An AV block, or a delay or interruption in the signals between the upper and lower chambers of your heart, can either be something you’re born with (congenital) or something that develops over time (acquired). Congenital AV block is often related to birth defects in the heart, but it’s more often seen in people without any such issues. It can also be caused by your immune system not working correctly, as you often see in conditions like lupus, or by a viral infection in the mother during pregnancy.
Acquired AV block, on the other hand, can be traced back to conditions like a heart attack, drug side effects, hormone disorders, or exposure to toxins. Yet, the most typical cause is just getting older and the wear and tear that comes with age, leading to the gradual breakdown of the heart’s signaling system.
Half of these age-related scenarios can be traced to diseases that cause scarring and hardening of your heart’s electrical system, like Lenègre disease and Lev disease. A higher-than-normal activity from the vagus nerve, the body’s main relaxation nerve, can also cause an AV block. This is often seen in younger people, though it is usually not serious and doesn’t often require a pacemaker.
Some heart diseases caused by enlarged heart muscles or muscle disorders can also result in a slower heart rate and AV blocks.
Acquired AV block can also stem from heart diseases that cause swelling and damage, like Lyme disease or rheumatic fever, inflammation of the heart due to infection, or even heart surgery, especially surgery on the aortic valve near the heart’s electrical system. Males who undergo a specific procedure to fix the aortic valve are particularly prone to develop an AV block, especially if they already have issues with their heart’s electrical system.
Risk Factors and Frequency for Atrioventricular Block
The exact number of people affected by AV blocks, which are problems with the heart’s electrical signals, is not known. This is because there have not been many large studies done about this condition. We do know that congenital AV block, which is caused by autoantibodies and present from birth, happens in about 1 out of every 15,000 births.
However, this number might be lower than the reality as it doesn’t count cases that result in a baby not surviving to birth. AV block caused by the heart’s conduction tissue degenerating or breaking down is more common in people over 65 years old.
- Third-degree AV block is rare in young people.
- One study suggests that first-degree AV block is more common in African-American patients than in Caucasian patients, regardless of their age (except in their 80s).
At this point, there are still many questions. We don’t have a lot of information about how different types of AV block are related to age, race, or gender.
Signs and Symptoms of Atrioventricular Block
When seeing a doctor for suspected AV block, a common heart condition, they will want to learn about your health background and other relevant factors. This includes:
- Any past or present heart disease
- All medications currently being taken, especially beta-blockers, calcium channel blockers, antiarrhythmic drugs, and digoxin
- Any recent procedures on your heart
- Signs or symptoms related to other diseases that can be linked to heart block, such as amyloidosis and sarcoidosis
- Your regular level of physical activity
- Whether you’ve been exposed to tick bites recently
Some forms of AV block, like the first degree and Mobitz type I, often show no symptoms and are discovered during routine examinations or an ECG. However, people with an AV block can commonly experience breathlessness when exercising, a feeling of tiredness, a sensation of dizziness, and fainting. Cases of cardiac arrest or sudden cardiac death are rare.
Even though a physical exam might not confirm AV block, it’s important for doctors to assess for any underlying heart diseases that might be causing AV block and to check the heart’s pumping efficiency. When examining a patient for AV block, doctors might notice a slow heart rate, an irregular pulse, low blood pressure, and swollen neck veins that show noticeable A waves.
Testing for Atrioventricular Block
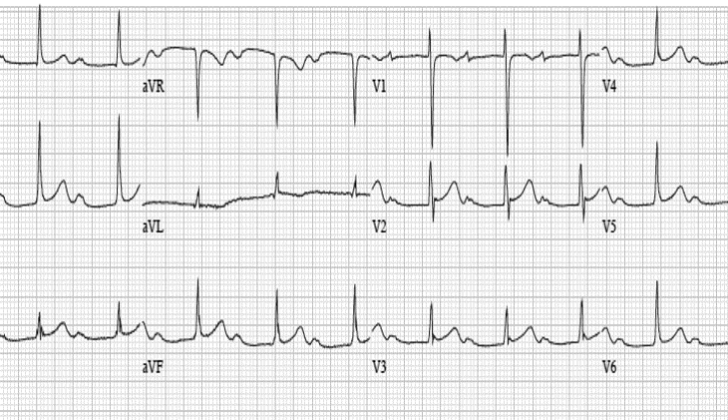
Atrioventricular Block, otherwise known as AV block, comes in different types, each with specific characteristics.
First-degree AV block refers to a heart condition where there is a delay in the transmission of electrical signals. The heart signals are slower than usual, but they aren’t blocked, and every signal reaches the lower chambers of the heart, or the ventricles. If this delay is extremely long, exceeding 300 milliseconds, it is referred to as “marked” first-degree AV block.
Second-degree AV block is when some electrical signals don’t reach the ventricles intermittently. This category is split into two types: Mobitz type 1 (Wenckebach) and Mobitz type 2. Mobitz type 1 has heart signals that gradually get slower until a signal fails to reach the ventricles. Mobitz type 2, on the other hand, involves erratic, unpredictable signal losses. If every other signal is blocked, it’s referred to as a 2:1 AV block. An even more serious type, the advanced or high-grade AV block, is when two or more consecutive signals fail to reach the ventricles.
In the most dangerous type, the third-degree or complete heart block, none of the electrical signals are conducted to the ventricles, i.e., the heart’s upper and lower chambers beat independently of each other. So, the top chambers (atria) beat normally while the ventricles beat at a slower pace.
When it comes to diagnosing AV block, non-invasive procedures are pretty standard. By running a 12 lead ECG, physicians can evaluate the severity of the block and localize the position. However, sometimes it’s hard to link symptoms to the AV block based purely on an ECG. In such cases, doctors can use ambulatory ECG monitoring or exercise ECG as they provide more accuracy in diagnosing AV block. Other tests like echocardiograms or cardiac MRIs can be useful too if doctors suspect associated structural heart diseases, myocarditis, or infiltrative cardiomyopathies.
In certain situations, invasive evaluation like an implantable loop recorder or an electrophysiology study might be needed, particularly if a non-invasive test didn’t give a clear diagnosis. Lastly, a series of lab investigations like thyroid function tests, electrolyte levels, renal profile, and digoxin levels could be conducted based on each patient’s symptoms. Genetic testing may also be done if a hereditary AV block is suspected.
Treatment Options for Atrioventricular Block
In simpler terms, patients with first or second-degree Mobitz type 1 heart block typically don’t need treatment if they aren’t showing symptoms. It’s important to stop any medications causing the heart block and tackle any other reversible causes. These patients can receive their care as outpatients. However, patients with more severe heart block require close monitoring in the hospital as they’re at a greater risk of serious complications like a flatlining heart, rapid heart rate, or sudden cardiac death.
Routine implantation of an emergency temporary pacemaker in second-degree or third-degree heart block cases shouldn’t be an automatic response. It’s crucial to weigh up the benefits and risks in the context of the patient’s broader health. Factors to consider include blood pressure, the severity and duration of symptoms, where in the heart the blockage is located and whether there’s a backup heart rhythm.
In cases where a heart block could be due to reversible triggers like drug overdose or infection, immediate medical treatment is often needed to reverse the condition causing the block. Atropine administered intravenously is a potential first line of treatment where the blockage is expected to be at the top of the heart (the atria). If a patient has symptoms of second or third-degree heart block and signs of a heart attack, dopamine and isoproterenol drugs can also be considered.
A temporary pacemaker could be an option in some severe cases, particularly if the patient is not responding to initial treatments or is experiencing a ‘heart shock’. However, this type of pacemaker should not be used more than necessary as it can elevate the risk of infection and other complications related to implanting electronic heart devices. Patients’ risk of immobility, infection, blood clots, and heart perforation must be considered against the benefits.
In the long term, a permanent pacemaker is the primary treatment for heart block. Patients not showing symptoms with a first-degree or second-degree type I heart block, or a block at the heart’s atrioventricular node, generally won’t need a pacemaker and should be monitored on an outpatient basis. A pacemaker might be needed if they develop symptoms due to the heart block. As a rule, patients with symptomatic second-degree heart block, high-degree AV block, or third degree heart block, not caused by something that can be reversed, should have a pacemaker fitted. Those with second-degree or third-degree heart block along with specific other conditions should have both a permanent pacemaker and a defibrillator fitted. A dual-chamber pacemaker is typically recommended, but a single-chamber pacemaker could be a suitable option in specific cases.
What else can Atrioventricular Block be?
Individuals showing signs of an AV block, a type of heart block, require a thorough examination to figure out the causes. Doctors typically use a tool called a 12-lead ECG (a type of heart monitor) for this. It helps doctors distinguish between an AV block and other heart-related conditions like isorhythmic AV dissociation (two separate rhythms in the heart) and junctional escape rhythm (irregular heart rhythm).
What to expect with Atrioventricular Block
Atrioventricular block, often known as AV block, is the most frequent reason for the implantation of a pacemaker worldwide. Patients with a third-degree AV block, who don’t receive treatment, face a low survival rate of 37% over five years. Those with AV block who don’t show symptoms generally fare slightly better than those who do display symptoms. Comparatively, men diagnosed with a third-degree AV block usually fare worse than women.
Beyond the block itself, variables such as a patient’s age, and the presence of health conditions like high blood pressure, heart disease, diabetes, chronic kidney disease, and underlying heart ailments can also influence how well a patient does. That said, the implantation of pacemakers has been shown to significantly improve the lifespan and quality of life for patients with AV block who show symptoms.
Possible Complications When Diagnosed with Atrioventricular Block
AV block, or Atrioventricular block, can come with several complications. These may include fainting, heart failure, an irregular heartbeat (also known as atrial fibrillation), or cardiac arrest where your heart suddenly stops. In certain cases, there could be abnormally slow heart rate leading to fast, irregular heartbeats, a condition known as bradycardia-induced ventricular tachycardia. In rare cases, it can lead to sudden cardiac death.
Here are the potential complications of AV block:
- Fainting
- Heart failure
- Atrial fibrillation (irregular heartbeat)
- Cardiac arrest (the heart suddenly stops)
- Bradycardia-induced ventricular tachycardia (abnormally slow heart rate leading to fast, irregular heartbeats)
- Rarely, sudden cardiac death
Preventing Atrioventricular Block
Patients with mild heart conditions (first-degree and symptom-free Mobitz type 1 AV block) can generally continue their regular activities. However, they should avoid any medication that could slow down the heart rate. Patients with more severe heart blockages (Mobitz type 2 and third-degree AV block) should have a detailed conversation with their heart doctors about the possible need for a pacemaker.
Most importantly, everyone should understand the serious symptoms of reduced blood flow, which include tiredness, feeling faint, passing out, feeling like they might pass out, or chest pain. It’s crucial for patients to immediately seek medical help if they notice any of these symptoms.