What is Atrioventricular Reciprocating Tachycardia?
Atrioventricular reciprocating tachycardia (AVRT) is a specific type of fast heart rate categorized as supraventricular tachycardia (SVT). This condition involves certain electrical and physical characteristics of the heart. AVRT revolves around a circuit, consisting of two or more pathways with differing electrical properties, such as the speed of conduction, refractory periods, and directionality.
Many ways exist in which an AVRT can form and function, including:
* Two communication pathways between the upper and lower chambers of the heart (the atria and ventricles).
* One extra pathway, on top of the usual route via the atrioventricular node, completing the circuit.
* Several extra pathways, which may perpetuate the SVT.
AVRT often begins with an out-of-place heartbeat originating from either the atria (upper chambers of the heart) or the ventricles (lower chambers of the heart). This heartbeat travels down one path of the circuit because of the unique electrical properties of the tissues involved. These properties allow a rapid heart rate of 150 to 250 beats per minute to start and continue.
AVRT is the most common abnormal heartbeat associated with Wolff-Parkinson-White (WPW) syndrome. In this condition, electrical signals usually move through an extra pathway, visible on an electrocardiogram (ECG). The ECG reveals an abnormally quick beginning to the heartbeat, followed by a particular wave known as a delta wave, resulting in a widened heartbeat signal. Abnormal heartbeats originating from the atria, especially atrial fibrillation, can travel rapidly to the ventricles through these bypass pathways, which can be dangerous.
By contrast, permanent junctional reciprocating tachycardia, a rare form of AVRT, uses the atrioventricular node as its main limb with a slower transmitter acting as a-return pathway. This form of tachycardia tends to have a slower heart rate (between 130 and 150 beats per minute) and often loatsens’t respond efficiently to medical treatment. There are also other rare forms of AVRT that use special pathways (called Mahaim pathways) between different parts of the heart.
What Causes Atrioventricular Reciprocating Tachycardia?
The tricuspid and mitral valves in the heart usually act as an electrical barrier between the upper and lower chambers, except at a specific spot called the atrioventricular node. In some cases, extra muscle tissues, known as accessory pathways, connect the upper and lower chambers. These pathways can bypass the usual protective barrier created by the tricuspid and mitral valves. These accessory pathways can transmit electrical signals in various directions, making the heart beat in abnormal ways.
Patients with a rare heart problem called Ebstein anomaly often have more of these accessory pathways. This makes the treatment of their abnormal heart rhythms more difficult. The properties of these extra muscle tissues often resemble those found in the Purkinje fibers – a part of the heart’s electrical system. They usually conduct signals very rapidly, and are often resistant to a drug called adenosine, which is used to treat heart rhythm disorders.
Nevertheless, some accessory pathways can slow down the electrical signals. These are known as Mahaim accessory pathways and are unique as they respond to adenosine. This is important as it affects how heart rhythm disturbances are treated in these cases.
Risk Factors and Frequency for Atrioventricular Reciprocating Tachycardia
The fourth most common type of fast heartbeat, known as Supraventricular tachycardia (SVT), in people over 20 years old is atrioventricular reciprocating tachycardia (AVRT). It sits behind atrial fibrillation, atrial flutter, and another type called atrioventricular nodal reentrant tachycardia (AVNRT). However, among children, AVRT is the most common type of SVT.
- In babies, the highest occurrence of AVRT happens from 1 month to 1 year old, with the condition resolving by itself in 90% of babies by their first birthday.
- However, around 30% of these may experience a recurrence of AVRT early in their childhood, between the ages of 6 and 9.
- There may be multiple abnormal electrical pathways in the heart in 4% to 10% of patients. This is especially true for patients with a specific heart defect known as Ebstein anomaly.
- It’s very important to identify these extra electrical pathways during a special heart study. If they’re found, these extra pathways can be eliminated with a procedure that uses high-frequency energy (radiofrequency ablation) or extreme cold (cryoablation). This can help to prevent AVRT from happening again.
Signs and Symptoms of Atrioventricular Reciprocating Tachycardia
AVRT, also known as Atrioventricular Reentrant Tachycardia, shows various symptoms depending on any existing health issues a person may already have. The most common symptom is palpitations, which feels like a rapid, abnormal heartbeat. It’s also possible to experience dizziness, chest pain or feeling faint.
- Palpitations (a rapid or irregular heartbeat)
- Dizziness
- Chest pain
- Feeling faint (syncope)
Testing for Atrioventricular Reciprocating Tachycardia
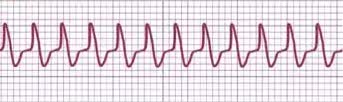
A quick overview of what an ECG does: an experienced heart specialist can use a 12-lead EKG (a type of heart rhythm test) to tell the difference between various heart rhythm problems. These include orthodromic AVRT (where a hidden extra pathway is involved), AVNRT, antidromic AVRT (where the extra pathway is involved in a different way, resulting in a broad heartbeat pattern), and ventricular tachycardia. Interestingly, artificial intelligence is showing high potential in differentiating between these heart rhythm problems, even matching the performance of experienced heart specialists.
Depending on the nature of the ECG readings, it can raise suspicion of different conditions. In patients who exhibit a narrow QRS complex (a particular pattern on the EKG), it could suggest either Orthodromic AVRT or AVNRT. Things like the length of the RP interval (another part of the EKG reading) and carotid palpations (feeling the pulse in the neck) can provide further clues.
That said, wide QRS readings can signal towards conditions like Antidromic AVRT, AVNRT with a bundle branch block (delay or blockage of the electrical impulse along the path to the lower heart chambers), or ventricular tachycardia. A specific issue with the electrical conduction system of the heart, known as WPW syndrome, could also result in wide QRS readings.
Further investigation via an electrophysiologic study can be used to narrow down the diagnosis. In this study, small tubes (catheters) with electrodes are inserted into the heart to track and distinguish the rhythm abnormalities. They can also treat the rhythm problem by delivering controlled radiofrequency or cryoenergy to the offending pathway or rhythm focus. Although traditional techniques use fluoroscopy (a type of X-ray) that exposes the patient to radiation, some centers are using novel methods to minimize radiation exposure.
During this study, AVRT can be identified if there is a block in the bundle branches (the pathways that the electrical impulses take), which results in an increase in the VA interval (the time it takes for an electrical impulse to travel from the ventricles to the atria). This finding can help to pinpoint the location of the accessory pathway. Specific pacing techniques can also help to further identify the presence and location of an accessory pathway.
Treatment Options for Atrioventricular Reciprocating Tachycardia
Managing a type of arrhythmia called AVRT involves stopping the current episode and preventing recurrences. If the patient is unstable, confused, or is suspected to have chest pain related to heart artery issues, immediate electric shock treatment is suggested.
For stable patients, doctors can try simple methods to slow the heart rate, such as having the patient perform a Valsalva maneuver, which involves straining against a closed-off windpipe, or a carotid massage, where the doctor puts pressure on the carotid arteries one at a time. If these don’t work, the doctor can give an intravenous dose of a drug called adenosine, which is very effective at stopping this type of fast heartbeat with minor and temporary side effects. If needed, the dose can be increased. Another drug, verapamil, can also be used, but careful monitoring is needed for patients with weakened hearts. Other drugs that can be used include procainamide or beta-blockers.
AVRT that presents with a wide heartbeat tracing (QRS complex) can be harder to diagnose in the moment. If this type of AVRT is confirmed, some medications should be avoided, and instead, procainamide can be used.
To prevent future episodes of arrhythmia, most patients, especially younger ones, should have a procedure called a radiofrequency ablation to remove the extra pathway causing the fast heartbeat. If this procedure fails, if the patient refuses to have it, if the patient is too young or too small for the procedure, or if doctor expects the arrhythmia to get better with age, drugs to prevent arrhythmia can be used.
These drugs include beta-blockers like propranolol, sodium channel blockers such as propafenone, and amiodarone. They all work in different ways to slow the heart down. Propranolol is often used as the first choice, especially in babies. Amiodarone can also be very effective, but it can have unpleasant long-term side effects so it’s used when other drugs don’t work. For babies, the drugs can be stopped after one year in most cases, except in those who were diagnosed before birth, who have an increased risk of persistent fast heartbeats. For these babies, and for children above 15 kg with persistent fast heartbeats, radiofrequency ablation can be a very effective treatment.
What else can Atrioventricular Reciprocating Tachycardia be?
When a doctor is trying to diagnose a condition called orthodromic atrioventricular reentrant tachycardia (AVRT), they would also consider other heart conditions that have similar symptoms. These include regular, narrow heart rhythms such as increased heart rate (sinus tachycardia), irregular beating of the atria (atrial flutter), and rapid heart rhythm that starts in the heart’s upper chambers (AVNRT).
When it comes to diagnosing antidromic AVRT, another type of heart rhythm disorder, the doctor would also consider the possibilities of conditions with regular, wide heartbeat patterns, such as ventricular tachycardia where the lower chambers of the heart (ventricles) beat very quickly.
What to expect with Atrioventricular Reciprocating Tachycardia
Patients with AVRT generally have a good prognosis, as the irregular heart rhythm can usually be stopped using methods like vagal maneuvers, adenosine, or treatments such as radiofrequency ablation or cryoablation. But if AVRT happens in a patient with WPW syndrome, who has an abnormally functioning pathway, the advent of a condition called atrial fibrillation can lead to sudden cardiac death if it rapidly affects the ventricles of the heart.
The chance of this resulting in an irregular heart rhythm called ventricular fibrillation in these patients can be up to 0.3%, and the risk of life-threatening events can be 70 times higher compared to the general population.
Possible Complications When Diagnosed with Atrioventricular Reciprocating Tachycardia
AVRT, or atrioventricular reentrant tachycardia, can lead to complications such as shortness of breath, chest pain, a feeling of fainting or actual fainting. Though it’s rare, sudden heart failure can happen as the first sign of a specific form of AVRT, especially in people with atrial fibrillation who have one or more abnormal pathways. Especially at risk are those whose abnormal pathways signal very quickly, as indicated by short RR interval in their heart rhythms.
Radiofrequency ablation is a treatment used to correct irregular heart rhythms. However, it can also lead to complications in 2 to 4% of patients. Data from a large national patient registry highlighted complications such as:
- Cardiac tamponade, a severe emergency condition where fluid accumulates around the heart
- Acute myocardial infarction, or heart attack
- Femoral artery pseudoaneurysms, a type of blood vessel damage
- Atrioventricular block, a type of heart block
- Pneumothorax, or collapsed lung
- Pericarditis, inflammation of the sac surrounding the heart
Despite these potential complications, improved procedures and advanced mapping systems have helped in reducing the complications related to radiofrequency ablation.
Preventing Atrioventricular Reciprocating Tachycardia
Educating patients is highly important in handling their conditions. They need to understand the symptoms of a fast heartbeat, also known as a tachyarrhythmia. Additionally, it’s important for patients to learn about the pros and cons of a treatment called radiofrequency ablation (RFA) and how heart rhythm medication can affect them in the long run.