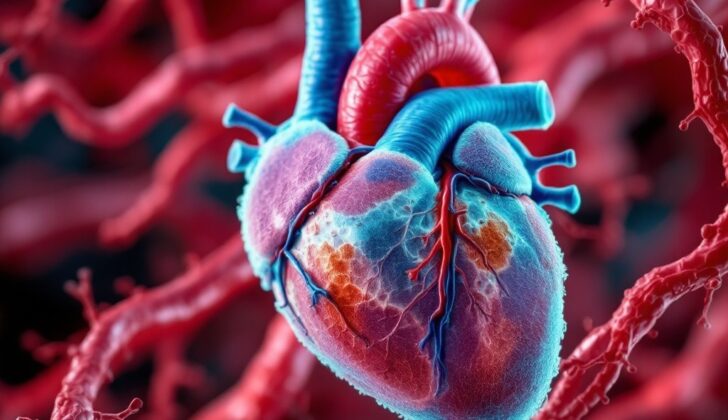
What is Chronic Coronary Occlusion?
Chronic Coronary Occlusion or Chronic Total Occlusion (CTO) refers to a condition where the blood vessels that supply the heart become completely blocked, causing no forward blood flow. This blockage should be present for at least three months to be labeled as chronic. The major arteries affected by this condition are the right coronary artery (in 43% to 55% of cases), the left anterior descending artery (about 24% of cases), and the left circumflex artery (17%-20% of cases).
Functional CTOs are when the blockage is severe, but not completely closing off the arteries. These cases have some forward blood flow due to the development of new routes the blood can take, or collateral circulation. However, this isn’t enough to support the heart in future instances where oxygen is in high demand, which indicates a need for treatment to reestablish blood flow.
What Causes Chronic Coronary Occlusion?
Chronic total occlusions are a type of heart blockage that forms when a blood clot in the heart hardens and turns fibrous. About 40% of people with this kind of blockage have previously had a heart attack. The risk factors for developing a chronic total occlusion are the same as those for coronary artery disease, a condition that affects the arteries of the heart.
Risk Factors and Frequency for Chronic Coronary Occlusion
Coronary artery blockage, also known as coronary occlusion, is a condition that affects a significant number of people with coronary artery disease – somewhere between 18% to 35%. This means that, for every five patients with coronary artery disease, one or two of them might have a complete blockage in one of their coronary arteries.
Chronic coronary occlusion tends to affect men (around 85% to 98% of cases) and older people (with the average age being around 64). But, it’s important to note that being older or male does not guarantee success in the procedures used to treat this condition; the results vary.
Though age is associated with a higher risk of chronic occlusion in two types of arteries – the right coronary and left anterior descending arteries. This isn’t the case for another artery known as the circumflex artery.
- Coronary occlusion affects 18% to 35% of patients with coronary artery disease.
- The condition, particularly when chronic, is more common in males (85% to 98% of cases).
- It is also more common in older people (with an average age around 64).
- The effect of age and sex on the success of treatment can vary.
- Increasing age is linked to a higher risk of this condition in the right coronary and left anterior descending arteries, but not in the circumflex artery.
Signs and Symptoms of Chronic Coronary Occlusion
Generally, the signs and symptoms of blocked coronary arteries depend on how severe the blockage is. The symptoms are due to a lack of oxygen supply to the heart muscle or issues with the heart’s contraction.
Individuals with a partial blockage may experience chest pain, shortness of breath, and fatigue, especially during physical exertion. These symptoms often go away when the person is at rest. Unfortunately, if the arteries are fully blocked, the symptoms may not improve even when resting, and medications may not provide relief. As such, doctors need to thoroughly examine a patient’s medical history, including any potential risk factors like family history, smoking, obesity, high blood pressure, lack of exercise, excessive drinking, diabetes, and a sedentary lifestyle.
During a physical exam, doctors will perform a full body check for signs of raised, fatty deposits on the skin (xanthomas) and assess the patient’s blood circulation. This is followed by a thorough examination of the cardiovascular system.
Testing for Chronic Coronary Occlusion
An electrocardiogram (EKG), a test that checks the heart’s electrical activity, can sometimes show changes in patients with a long-term blockage in the arteries that supply the heart (chronic coronary occlusion). However, these changes are not always specific, which means they aren’t solely linked to this condition.
Most often, it’s during a procedure called a coronary angiography, typically due to persistent chest pain, that a chronic coronary occlusion is detected. This procedure is also opted for when there’s a need to open narrowed or blocked blood vessels that supply blood to the heart or when tests suggest that there’s a lack of blood and oxygen reaching the heart tissues. During a coronary angiography, a small tube (catheter) is inserted into a blood vessel in the leg or wrist and threaded towards the heart. A special dye is then injected via this tube into the heart’s blood vessels. This allows doctors to see the flow of blood in the arteries supplying the heart and check for any blockages.
In addition, it is common to find chronic coronary occlusion in older patients who have other medical conditions and display a higher level of heart function impairment.
Treatment Options for Chronic Coronary Occlusion
Treatment for heart disease largely depends on how severe the condition is. This can include lifestyle changes, medication, and medical procedures such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG).
In the case of subtotal coronary occlusion, which means the artery is partially blocked, the treatment is similar to that for stable angina, a type of chest pain caused by inadequate blood flow to the heart. Initially, beta-blockers are the preferred medication to prevent symptoms. If beta-blockers cannot be used, or if they cause side effects, alternatives include calcium channel blockers and long-acting nitrates. Short-acting nitrates can be used for instant relief from angina. Additionally, various therapies can be used to prevent the condition from getting worse and to reduce the risk of heart problems. These can include aspirin, cholesterol-lowering medication, quitting smoking, controlling blood pressure, losing weight, and managing diabetes. Regular exercise and stress reduction are also recommended. It’s important that these patients have regular check-ups, ideally every 6 to 12 months.
If the coronary artery is completely or almost completely blocked and does not respond to medication, a procedure such as PCI or CABG may be needed. The best procedure for each patient depends on the specifics of their condition.
For disease in a single vessel, PCI is usually preferred. This is a procedure that involves a small incision in the groin or wrist. A wire is threaded through the blood vessels to the blocked artery in the heart, and then an opening is created in the blockage using a guidewire. After that, a catheter is guided over the wire to the blockage, a small inflatable balloon is used to push the blockage aside, and finally, a stent (a small metal mesh tube) is placed in the artery to keep it open.
For disease affecting multiple vessels, CABG is usually the preferred treatment.
What else can Chronic Coronary Occlusion be?
There are numerous medical conditions that can resemble chronic coronary occlusion, especially when symptoms like chest pain or shortness of breath are present. These include:
- Atherosclerosis (plaque in the arteries)
- Angina pectoris (chest pain due to reduced blood flow to the heart)
- Unstable angina (a condition where chest pain not relieved by rest)
- Coronary artery vasospasm (a contraction of the heart arteries)
- Myocardial infarction (heart attack)
- Hypertensive heart disease (heart problems due to high blood pressure)
- Isolated coronary artery anomalies (rare heart defects that you’re born with)
These conditions usually have similar symptoms which make it challenging to diagnose without specific tests. Therefore, if a person experiences chest pain or shortness of breath, it’s important to seek medical attention promptly.
What to expect with Chronic Coronary Occlusion
The outlook mainly depends on how severe the disease is. People with only a partial blockage in their coronary arteries generally have a better outlook than those with a total blockage. A total blockage in the coronary arteries often leads to a poorer overall outlook, with higher chances of death and severe heart-related incidents in several populations.
Individuals with untreated coronary artery blockages have been found to face a higher risk of death. Additionally, they are more likely to experience major heart-related events, including death due to a heart attack compared to patients with multiple blocked coronary arteries who have been fully treated.
Possible Complications When Diagnosed with Chronic Coronary Occlusion
The disease can have serious complications, including a greater chance of experiencing heart-related events like irregular heartbeats, heart attacks, or even death. There are also risks involved with the procedure to treat it, known as PCI. These risks are significant heart-related issues, heart attacks, severe perforation classified as Ellis grade 3 or higher, bleeding that needs treatment, sudden kidney damage, rejection of the graft in CABG procedures, and potentially death.
Common Complications of the Disease and its Treatment:
- Greater chance of heart-related events (arrhythmias, heart attacks)
- Death
- Significant heart-related issues with PCI treatment
- Severe perforation that is Ellis grade 3 or higher
- Bleeding that requires treatment
- Sudden kidney damage
- Rejection of the graft in CABG procedures
- Potential death with PCI procedure
Preventing Chronic Coronary Occlusion
Successfully improving the blood flow to the heart helps with long-term survival rates, reduces the need for bypass surgery, and enhances the heart’s left chamber’s function in patients suffering from Chronic Total Occlusion (CTO). It’s been found that smoking, high blood pressure, and diabetes are strongly linked with CTO.
As a part of the treatment, it’s important for doctors to not only take care of patients but also educate them about their condition. Understanding the nature of the disease, its process, and the goals of the treatment like changing lifestyle habits, taking medicines regularly, and understanding the risks and benefits of medical procedures is vital for successful treatment. Moreover, patients should also be provided with educational brochures and other resources related to their disease to help them understand their condition better.