What is Electrical Alternans?
Electrical alternans refers to when the heart’s electrical activity, as seen in a heart rhythm test (ECG), shows an alternating pattern. There are no changes to the heart’s electrical pathways themselves, only how they appear on the ECG. This pattern often points to a condition called pericardial effusion, which is essentially fluid building up around the heart, making it sway. However, it can also point to other heart issues like rapid heartbeats, a condition called Wolff-Parkinson-White syndrome, a slow heart rate that comes from the bottom chambers of the heart, and fast heartbeats that start in the upper chambers of the heart. Knowing the different conditions that can cause this ECG pattern is important for diagnosing and treating, if necessary, the problem effectively.
What Causes Electrical Alternans?
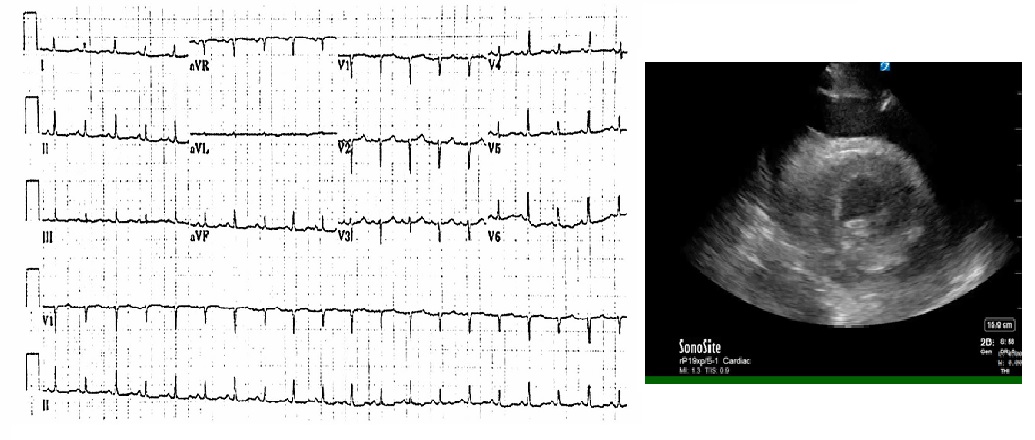
Electrical alternans is typically linked to two conditions: pericardial effusion (fluid around the heart) and tamponade pathology (pressure on the heart due to this fluid). It shows up as a distinct pattern on an ECG – a heart test that measures its electrical activity. This happens because the heart swings back and forth like a pendulum, leading to fluctuations in the heartbeat that the ECG picks up.
Electrical alternans can also be seen when changes occur in the heart’s conduction system – the system that regulates heart rhythm. Any variation in the heart’s rhythms can cause different heartbeats’ strength. These ECG changes resulting from these conditions will be further discussed under the discussion section of the pathology.
Risk Factors and Frequency for Electrical Alternans
Electrical alternans, a condition usually linked with pericardial effusion, can be caused by a variety of problems such as infection, inflammatory syndromes, trauma, cancer, and some unexplained causes. Although there’s usually an underlying reason for pericardial effusion, in 20% of cases, the cause remains unknown. This makes diagnosis and treatment difficult.
Even though pericardial effusion is not very common in patients showing ECG signs of electrical alternans, it is crucial to consider it as a possible issue. If not detected, it could lead to life-threatening complications. Besides pericardial effusion, there are other conditions that can cause electrical alternans to appear on an ECG. These include various types of abnormal heart rhythms and issues with the heart’s electrical pathways.
However, the detailed discussion of these unique conditions causing electrical alternans is beyond the scope of this explanation.
Signs and Symptoms of Electrical Alternans
When a person’s EKG test shows a condition called electrical alternans, they require more tests because the treatment depends on the underlying issues causing this condition. It is critical for the doctors to conduct a detailed medical history and physical examination of the patient, with a special focus on the heart and lungs. If the problem is due to pericardial effusion (fluid around the heart), these patients typically don’t show any symptoms unless tamponade physiology (pressure on the heart) occurs. Tamponade signs include Beck’s triad, which consists of low blood pressure, muffled heart sounds, and swollen neck veins. Some patients may also have rapid and shallow breathing (tachypnea), difficulty in breathing (dyspnea) that resembles Kussmaul breathing, and Pulsus Paradoxus.
- Low blood pressure
- Muffled heart sounds
- Swollen neck veins
- Rapid and shallow breathing
- Difficulty in breathing
If the underlying problem is arrhythmia (irregular heartbeat), patients may have a fast heart rate (tachycardia) and feel lightheaded, tired, have chest pain, shortness of breath, or faint (syncope), amongst other symptoms. It’s also possible they have a history of heart electrical system issues. With arrhythmia suspected, doctors may need to ask about patient’s family history of heart diseases.
Testing for Electrical Alternans
When a condition known as electrical alternans appears on an ECG (a test that measures the electrical activity of your heart), it means further tests need to be conducted to determine the root cause. This might happen if your doctor suspects a fluid buildup around your heart, otherwise referred to as a pericardial effusion.
In this case, a specific test called a transthoracic echocardiogram (TTE) would be done. Think of this as an ultrasound for your heart – it provides a close-up view of its structure and function. It’s an essential tool as it’s incredibly accurate (almost 100%) in diagnosing pericardial effusion. For patients who are unstable, having this examination done right at the bedside becomes even more crucial.
Treatment Options for Electrical Alternans
When someone is diagnosed with a serious condition known as tamponade, the first step is to immediately stabilize the patient. This requires giving them intravenous (IV) fluids, oxygen if necessary, and monitoring their heart. Sometimes, extra IV fluids are needed to help the heart function better and improve blood pressure and heart rate. However, to actually treat tamponade, a procedure called a pericardiocentesis is necessary.
Pericardiocentesis is an operation in which fluid is removed from around the heart. This procedure is usually performed in a specialized room for catheter procedures when the situation is not urgent. Yet, in serious situations such as when a patient is at risk of or going into cardiac arrest, the procedure can be done in the emergency department.
Once the procedure is done and fluid is removed from around the heart, the patient’s condition will need to be further studied to find out what caused this buildup of fluid.
For other conditions that can cause abnormal heart rhythms, including Wolff-Parkinson-White (WPW) syndrome, irregular heart rhythms originating from the ventricles, and bundle branch block (a condition where there’s a delay or obstruction along the pathway that sends electrical impulses to make your heart beat), the treatment will depend on the specific cause. The first and most important step in treatment is to ensure that the patient’s heart function and blood pressure are stable.
What else can Electrical Alternans be?
When discussing heart and lung conditions, doctors may examine or consider a variety of potential health issues. These can include, but are not limited to:
- Alternans bundle branch block
- Aortic stenosis
- Air embolism
- Bigeminy
- Cardiac rupture
- Digoxin toxicity which may cause bidirectional ventricular tachycardia
- Myocardial contusion or damage to the heart muscle
- Massive pulmonary embolus, a serious condition that involves a blockage in the lung arteries
- Severe tachypnea with wide varying tidal volumes, referring to rapid and shallow breathing
- Ventricular septal defect, a heart defect that occurs when there’s a hole in the wall separating the heart’s main pumping chambers
Considering these potential conditions is crucial in determining an accurate diagnosis and appropriate treatment plan.