What is Evaluation and Management of Perioperative Hypertension?
Hypertension, or high blood pressure, is the most common medical condition diagnosed. It can cause damage to many of the body’s organs, such as the vessels, heart, brain, kidneys, and eyes. This condition is linked with more deaths from heart disease than any other preventable disease, contributing to about 50% of deaths from heart disease and stroke in one major study. It’s estimated that hypertension is behind roughly nine million deaths worldwide every year. It also affects over 60% of people over the age of 60. Despite this, less than 20% of patients around the world successfully control it.
Hypertension is often termed the ‘silent killer’ because most patients do not show symptoms, yet the complications can be very serious. The lack of early symptoms is particularly worrying as starting treatment later can result in heart and kidney damage, along with a higher risk of heart disease, even in those who manage to bring their blood pressure down to normal levels.
Usually, the treatment and management of hypertension is handled by primary healthcare providers like internists, family physicians, and nurse practitioners. However, severe high blood pressure during or after surgery can lead to complications like excess bleeding, heart attack or congestive heart failure, and sudden buildup of fluid in the lungs. Because of this, anesthesiologists, nurses, and all healthcare professionals who prepare and manage patients around the time of surgery need to be well-informed about how to care for patients with hypertension.
What Causes Evaluation and Management of Perioperative Hypertension?
It’s often believed that blood pressure naturally rises as we age. However, recent studies suggest this might not be the case. The Yanomami people, who live in the Amazon rainforest and consume very little salt, have the lowest blood pressure of any society in the world. Conversely, their neighbors, the Yekwana people, who have some exposure to salt, have higher blood pressure, though it’s still much lower than in more modern societies. This suggests that high blood pressure could be linked to salt intake and a modern lifestyle.
Other factors that could increase the risk of high blood pressure include having a family history of it, being overweight, leading a sedentary lifestyle, smoking, and following a diet that’s low in potassium.
Risk Factors and Frequency for Evaluation and Management of Perioperative Hypertension
Systolic blood pressure, the pressure when the heart beats, keeps increasing until around the 90s. Meanwhile, diastolic blood pressure, the pressure when the heart rests, increases until around mid-50s before it starts to drop. This creates a bigger gap between systolic and diastolic pressures. Much of this is due to the stiffness in large arteries, causing less blood to fill the aorta and less bounce back during rest. High blood pressure, or hypertension, impacts roughly 29% of all people, slightly more men (30%) than women (28.1%). Initially, it’s more common in men but after about age 60, it affects more women.
When considering race, hypertension is more common in African Americans than whites, affecting 40.8% of African American men and 41.5% of African American women. It’s seen in 25.9% of Hispanic Americans and 24.9% of non-Hispanic Asians. Comparing different countries, hypertension is more common in Europe than in the United States, with prevalence rates of 38% in Italy and 55% in Germany. This difference may exist because European guidelines suggest starting medication at higher blood pressure levels.
Unfortunately, the percentage of people with hypertension continues to grow. Aging, obesity, and less physically active lifestyles are really driving this upward trend. According to predictions, nearly 1.5 billion people globally will have hypertension by 2025. It’s also increasingly affecting children, largely due to the rise in childhood obesity and inactive lifestyles.
Signs and Symptoms of Evaluation and Management of Perioperative Hypertension
Many patients confirm their high blood pressure (HTN) during a preoperative visit. Remarkably, over a third of individuals experiencing a hypertensive crisis weren’t aware they had high blood pressure. This emphasizes the need to check blood pressure (BP) during preoperative visits, ideally in both arms. Even though there are guidelines for measuring BP, mistakes are common. Measurements should be taken in a quiet room, with the patient sitting down.
The size of the BP cuff matters, too. If a cuff is too small, it can mistakenly suggest high BP; this is the leading cause of wrong HTN reports. A correctly sized cuff should have a bladder cuff length that fits 80% to 100% of the arm’s circumference, and it should be 40% of the mid-upper arm width. The cuff should be placed directly on the skin over the brachial artery. Interestingly, a larger cuff often provides an accurate reading.
Keep in mind that BP readings measure the mean arterial pressure (MAP) first, from which the systolic and diastolic BP readings are then calculated. BP readings can vary between different manufacturers due to their unique calculation algorithms. BP can also be measured in the legs, where it is typically 10 to 20 mm Hg higher than in the arms.
If someone’s BP is between 130/80 and 160/90 mm Hg and they mention they have “white-coat HTN”, it’s essential to confirm this diagnosis with home or ambulatory BP monitoring. “White-coat HTN” tends to become persistent HTN in 1 to 5% of patients each year, especially among older, obese individuals, and those with higher initial BP readings – African American individuals also face a higher risk. White-coat HTN is linked to a slightly increased risk of cardiovascular diseases and overall mortality risk.
When consulting with a patient, it’s crucial to ask about symptoms indicating damage to the body’s organs. High blood pressure can lead to heart diseases like coronary artery disease or increased left ventricular hypertrophy (LVH). Questions should revolve around any experiences of chest pain, breathlessness during exertion, orthopnea (trouble breathing while lying flat), or sudden, frequent breathlessness at night. Also, inquire about the patient’s walking and stair-climbing endurance and any symptoms related to stroke, kidney disease or visual changes that could indicate hypertensive retinopathy.
The physical exam can also show signs of high BP, like changes in various organs. Listening for specific heart sounds like an S3 or S4 gallop could indicate congestive heart failure (CHF). Swollen neck veins could suggest fluid overload or heart failure. Hearing crackles in the lungs could also indicate CHF. If the patient had a previous stroke, any resulting neurological deficiencies should be documented. An eye examination can also identify visual changes due to high BP. However, these examinations aren’t usually included in a preoperative assessment.
Testing for Evaluation and Management of Perioperative Hypertension
Treatment for high blood pressure, or hypertension, is typically managed by primary care doctors, and should ideally start well before any surgical procedure. It’s important that high blood pressure is diagnosed and treated based on several blood pressure readings taken on different visits. Lifestyle changes like a healthier diet, regular exercise, and reducing salt intake are crucial parts of the treatment plan. The aim of any treatment is to not only lower blood pressure, but also to reduce the risk of heart disease.
A number of medications can be used to treat high blood pressure – these can include thiazide diuretics, ACE inhibitors, angiotensin receptor blockers, and calcium channel blockers. Sometimes, other drugs may be used, like loop diuretics, potassium-sparing diuretics, aldosterone antagonists, beta-blockers, alpha-1 blockers, centrally acting drugs, and direct vasodilators.
If you’re due for surgery and have a history of medical issues, it’s important to have a pre-surgery assessment at an anesthesia clinic at least a week beforehand. This gives the team time to make any necessary changes to manage your health better, including any high blood pressure. Some clinics use a team-based approach to look after you before and after surgery.
As part of your pre-surgery evaluation, if your blood pressure is under control and your medical history and physical exam don’t show any concerning signs, you may not need any further tests if the surgery is relatively straightforward. But if the surgery is more invasive or if there are any concerns in your history or physical examination, you may need to have further tests like an electrocardiogram (ECG) or echocardiography. These tests can check for any issues with your heart’s structure and function.
Other tests such as blood tests to check kidney function or electrolyte levels may also be done, especially if you’re on certain high blood pressure medications. A complete blood count is often taken to ensure safe blood levels, especially for procedures where significant blood loss could occur. Therefore, if you have high blood pressure, it’s standard practice to check your kidney function before surgery.
Treatment Options for Evaluation and Management of Perioperative Hypertension
Patients with high blood pressure (HBP) are typically given a diuretic initially, although other medications like calcium channel blockers (CCB), ACE, and ARB can be used in non-black individuals as the first line of treatment. In black patients, treatment should start with a diuretic or CCB, as these have shown to reduce problems with the heart or brain. If the patients have stage 3 kidney disease or chronic kidney disease with significant protein in the urine, they should receive an ACE or ARB. However, these recommendations can vary depending on their heart risks and any damage to organs they may have.
It’s not agreed upon whether patients should take high blood pressure medication on the day of surgery. In general, patients are advised to take their medications as usual with a small amount of water. Diuretics are commonly not given due to fasting. But patients with severe chronic heart failure might need a lower or usual dose of diuretics. Whether or not to give these medications should be decided by the anesthesiologist after measuring blood pressure and listening to the lungs. It is usually agreed upon that patients should receive their beta-blocker on the day of the surgery. However, it has risk such as slower heart rate, stroke, and even death and hence should not be started just before surgery.
On the day of surgery, patients should have normal blood pressure, although it might be higher than normal due to anxiety. If the patient’s blood pressure is very high, the surgery may have to be postponed until it’s controlled better, the patient might be given their blood pressure medication if they hadn’t taken it. Depending on how severe their blood pressure is, the order of their procedure may need to be rearranged to give time for the medication to work and for the blood pressure to come down.
If the surgery is an emergency and has to proceed despite high blood pressure, several safety measures should be taken. This includes reviewing a recent EKG (electrocardiogram) and echocardiogram. If these are not available, they may need to be done as soon as possible. If there’s a big chance of serious heart problems, it might be necessary to closely monitor blood pressure and have medications ready to treat high blood pressure throughout and after surgery, potentially in the intensive-care unit.
In terms of managing high blood pressure during the surgery, the anesthesiologist has to ensure safe blood pressure levels. This can be done using anesthetics, pain killers, and high blood pressure medications that are suitable for the patient’s overall health condition. Certain regional nerve blocks can provide surgical anesthesia with minimal changes in blood flow. Spinal and epidural techniques allow normal breathing but may cause significant decrease in blood pressure. For such situations, increasing blood volume with fluids or vasoconstrictors would be helpful. Even so, a sure rule regarding anesthetics for each procedure is not recommended, because every patient’s health condition needs to be considered.
To avoid acute complications of HBP, it’s important to maintain the blood pressure within a certain range. For patients with high blood pressure and/or significant heart problems, the following targets for blood pressure during surgery can be used as a guideline: SBP approximately 130 mm Hg, MAP 60 to 65 mm Hg, and DBP 70 to 90 mm Hg. However, these ranges may not apply to patients undergoing brain surgery, and their appropriate blood pressure targets may be influenced by their baseline blood pressure, neurological status, and surgical procedure. Therefore, these patients may need a different approach.
In addition, if the surgery is classified as intracranial, intrathoracic, or major abdominal, insertion of an arterial line for continuous measurement of blood pressure may be advisable. If blood pressure fluctuations are major during surgery, hospitalization for 24 to 48 hours postoperatively may be necessary to control high blood pressure before discharge.
In critically ill patients where directly measuring blood pressure is not immediately available, blood pressure should be checked every one to two minutes non-invasively. However, in cases where patients have very high or low blood pressure, are receiving medications that can quickly change blood pressure, or are undergoing surgical procedures that may result in substantial changes in blood pressure or bleeding, direct measurement of blood pressure via an arterial catheter should be initiated as soon as possible.
What else can Evaluation and Management of Perioperative Hypertension be?
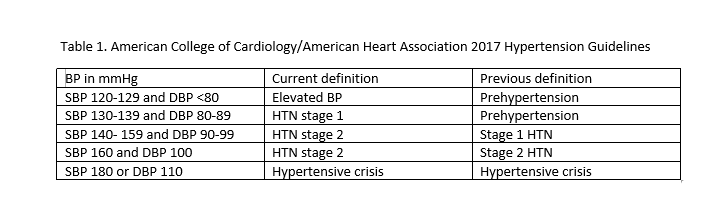
In 2017, standards changed for diagnosing hypertension (high blood pressure). Now, a systolic blood pressure (the first number) of 130 or a diastolic blood pressure (the second number) of 80 are considered to be high blood pressure.
The guidelines also shed light on distinguishing between “white coat hypertension” – where blood pressure readings are high only when they are taken in a medical setting – and “masked hypertension” – where blood pressure readings are normal in a medical setting but high at other times. To differentiate between these two conditions, doctors use a method called ambulatory blood pressure monitoring, a way of measuring blood pressure levels over a 24-hour period as a person goes about their regular activities.
What to expect with Evaluation and Management of Perioperative Hypertension
High blood pressure, or hypertension (HTN), is the leading risk factor for developing heart disease and can increase the risk of death. High blood pressure impacts over 60% of people over the age of 60 in developed countries. However, it’s important to note that this isn’t just an issue for older people. Young adults, even teenagers, with higher blood pressure are also at an increased risk of heart disease-related death when compared to their peers with lower blood pressure.
A lack of physical activity and obesity are contributing factors to high blood pressure in teenagers. Research has shown that rising blood pressure levels are linked to increasing rates of illness and death at all ages. Treating high blood pressure, particularly the higher number in a blood pressure reading (known as systolic or SBP) can significantly reduce the risk of death, heart disease, and stroke.
Although high systolic blood pressure appears to be a stronger indicator of risk in people over 50, the lower number in a blood pressure reading (diastolic or DBP) shouldn’t be ignored. High diastolic blood pressure can increase heart disease risks and is more commonly higher in people under 50. This connection was confirmed in two studies conducted on veterans with high diastolic blood pressures.
As people age, diastolic blood pressure often decreases due to the arteries becoming stiff. Consequently, systolic blood pressure assumes even greater importance as a risk factor starting from midlife.
Possible Complications When Diagnosed with Evaluation and Management of Perioperative Hypertension
High blood pressure (or hypertension, HTN) can cause complications in various parts of our body, including the blood vessels, heart, brain, kidneys, and eyes. The specific problems it may cause include atherosclerotic vascular disease (a disease of the arteries), coronary artery disease (CAD, a disease that affects the arteries that supply blood to the heart), cerebrovascular disease (a disease related to blood supply to the brain), kidney disease, and retinal hemorrhages (bleeding at the back of the eye).
One of the most common heart complications caused by hypertension is congestive heart failure, which is the inability of the heart to pump enough blood to meet the body’s needs. Increased blood pressure can also cause acute pulmonary edema (APE), a condition where excess fluid accumulates in the lungs, making it difficult to breathe. This happens because the increased pressure in the arteries decreases the ability of the heart to pump, leading to fluid build-up. These occurrences can happen regardless of whether the person had any vascularization procedures, or treatment to restore the blood supply. There is a risk of heart failure during surgeries due to the fluctuations in blood pressure and heart rate, so healthcare professionals need to be cautious about fluid management during these situations.
People with high blood, especially those with pre-existing conditions like diabetes, kidney disease, older age, CAD, heart failure, and atrial fibrillation (AFIB, an irregular and often rapid heart rate), are at a higher risk of stroke. The risk is especially high during surgeries involving the heart and carotid artery. In some cases, people undergoing non-cardiac surgery might experience a covert stroke, which is a stroke that doesn’t show immediate symptoms but could lead to cognitive decline, delirium, or a subsequent stroke or transient ischemic attack (a temporary interruption of blood flow to part of the brain) within a year.
There is a risk of acute kidney injury (AKI) during high blood pressure and surgeries. There are many ways to classify this injury, but we usually use the RIFLE and AKIN classifications that help predict outcomes and allow comparison between different studies. Both classifications use serum creatinine (sCr), a chemical waste product that’s produced by your muscle metabolism and to a smaller extent by eating meat, as a parameter, but its levels may take several days to rise after renal insult.
AKI and the need for renal replacement therapy (dialysis, a treatment to filter and cleanse the blood) are serious complications that can occur after surgery. Both these complications increase the chances of other diseases and death. There is a link between AKI and a shortened lifespan, even if the serum creatin levels return to normal. So, medical professionals need to take precautions to prevent the occurrence of AKI during surgeries, such as maintaining the mean arterial pressure (average blood pressure in a person’s arteries during one heartbeat) at least 60 mm Hg in adults, hydrating patients before injecting them with a contrast medium for medical imaging, and exercising care with the use of drugs that are toxic to the kidneys.
Preventing Evaluation and Management of Perioperative Hypertension
Occasionally, high blood pressure or hypertension may be first discovered during the period around a surgical procedure. If this happens, the person giving the anesthesia has to talk about it with the surgeon and/or the patient’s regular healthcare provider. It’s critical to treat hypertension because if left untreated, it can lead to serious health problems. That’s why doctors might suggest patients start medication to lower their blood pressure, a move that could significantly improve their health and quality of life.