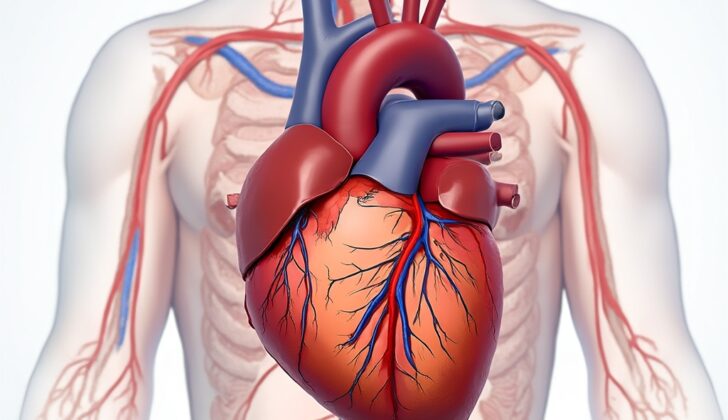
What is Inferior Myocardial Infarction (Heart Attack)?
An inferior wall myocardial infarction (MI), also known as a heart attack, happens when a coronary artery gets blocked, reducing the blood supply to a specific area of the heart. If treatment isn’t prompt, it can cause a shortage of oxygen in the heart muscle followed by a heart attack. In most people, the right coronary artery supplies this part of the heart, but in about 6-10% of individuals, due to left dominance, the left circumflex artery is responsible. Around 40% of all heart attacks involve the inferior wall of the heart. Heart attacks in this region usually have a better prognosis compared with other areas such as the front wall of the heart. The death rate of an inferior wall heart attack is less than 10%. However, certain complications can increase the risk of mortality, including damage to the right ventricle, low blood pressure, slow heart rate, heart block, and cardiogenic shock, a serious condition where the heart cannot pump enough blood to meet the body’s needs.
What Causes Inferior Myocardial Infarction (Heart Attack)?
A heart attack in the lower part of the heart, known as an inferior wall myocardial infarction, is caused by a lack of blood supply and damage to the area. In about 80% of patients, this lower section of the heart gets its blood supply from the right coronary artery, which reaches it via another artery called the posterior descending artery (PDA). However, for the other 20% of patients, the PDA is an offshoot of a different artery, the circumflex artery.
Risk Factors and Frequency for Inferior Myocardial Infarction (Heart Attack)
In 2013, there were about 8.6 million heart attacks, also known as myocardial infarctions, around the world. Inferior wall heart attacks, which are heart attacks that occur in the lower part of the heart, make up about 40% to 50% of all heart attacks. These types of heart attacks generally have a better prognosis, with a death rate between 2% and 9%. However, it’s important to note that up to 40% of inferior wall heart attacks also involve the right ventricle of the heart, which can lead to a worse outcome.
Signs and Symptoms of Inferior Myocardial Infarction (Heart Attack)
When examining a case suspected of acute coronary syndrome (heart-related problems), certain symptoms and signs should be closely checked. These typically include:
- Chest pain, heaviness or pressure
- Shortness of breath
- Excessive sweating (diaphoresis) that may spread to the jaw or arms
- Additional symptoms like fatigue, feeling lightheaded, or nausea
During a physical exam, it’s crucial to monitor the heart rate, as slower-than-normal heart rate (bradycardia) and interrupted heartbeat patterns (heart block) might occur. Blood pressure should also be assessed, alongside any signs of inadequate blood circulation, especially if the person’s right ventricle, one of the heart’s pumping chambers, is also affected.
Testing for Inferior Myocardial Infarction (Heart Attack)
An important part of checking for heart problems involves conducting regular ECG checks early on. The ECG leads II, III, and aVF help us look at the lower part of the heart. An elevation in the ST-segment of these leads indicates a specific type of heart attack known as an inferior wall STEMI. Often, we also notice a reciprocal ST depression in lead aVL. In fact, nearly half of the lower heart wall attacks are linked to right ventricle heart attacks.
To get a better look at the right ventricle, additional right-sided ECG leads should be used. This is done by placing the precordial leads on the right side of the chest, replicating the same pattern as the traditional precordial leads placed on the left side. Particularly, Lead V4R helps in spotting a right-sided heart attack.
If the ECG shows signs of an ST elevation heart attack, the patient should be moved to a specialized heart lab for treatment right away. If the ST elevation is not noticed, then troponin levels should be kept under observation since troponin is a heart protein that rises in the blood level when a heart attack happens.
Treatment Options for Inferior Myocardial Infarction (Heart Attack)
If the ECG shows signs of ST elevation, which is a pattern indicating potential heart damage, immediate emergency measures are needed. The patient should have an urgent heart test called cardiac angiography in the catheterization lab. It’s important that this test is done within 90 minutes to keep the heart vessel open as long as possible.
In certain cases, a treatment called thrombolysis might be needed. This depends on the facilities available or if the patient has to travel a long way to reach a hospital where a catheterization is possible.
If there are signs of damage to the right side of the heart, it’s important to avoid certain treatments such as nitrates, which can reduce the blood volume returning to the heart, and to ensure there’s enough blood volume for the heart to function properly. The right side of the heart is thinner and more dependent on blood volume for its performance. If too much blood volume is lost, this could lead to a significant drop in blood pressure, and if this happens, fluid replacement and possibly medication to increase blood pressure will be needed.
Other treatments include a high dose of aspirin (162 to 325 mg), a type of blood thinner called unfractionated heparin, a medication known as a GP IIb/IIIa antagonist, and additional blood-thinning medications such as clopidogrel.
What else can Inferior Myocardial Infarction (Heart Attack) be?
There are many potential reasons for certain symptoms like chest pain during exercise, sweating, feeling sick, throwing up, and pain that spreads to the right arm. These could be signs of heart disease. It’s also important to bear in mind other serious conditions such as lung blood clots (pulmonary embolism), problems with the aorta (aortic dissection), collapsed lung (pneumothorax), esophagus damage (esophageal rupture), and a condition where fluid builds around the heart (cardiac tamponade).
Sometimes, symptoms might not be typical, especially in women and older patients. So, doctors need to be really vigilant. Symptoms like nausea, vomiting, upper abdominal pain and feeling tired could actually indicate heart-related issues, not just a stomach disorder. Therefore, it’s really important not to dismiss these signs as just a tummy problem.
What to expect with Inferior Myocardial Infarction (Heart Attack)
Although heart attacks in the lower wall of the heart (inferior wall) usually have a positive prognosis, some factors can increase risks. It’s important to note that about 40% of heart attacks in this area also involve the right ventricle of the heart. These types of heart attacks heavily rely on the volume of blood coming into the heart (pre-load) and certain medications, like nitrates, can cause a significant drop in blood pressure.
Adding right-sided ECG leads, especially lead V4r, can help diagnose this condition. If treatment isn’t administered promptly, more heart muscle may die which might lead to cardiogenic shock, a serious condition where the heart can’t pump enough blood to meet the body’s needs.
Furthermore, since the artery that supplies the natural pacemaker of the heart (right coronary artery) is also affected, slowed heartbeat (bradycardia), or complete heart block may occur. This type of complete heart block is reported in 19% of patients who experience acute lower wall heart attacks. The presence of collateral circulation, or natural bypasses in the heart, can affect the frequency of this block.
However, if other diseases also affect the coronary arteries, these natural bypasses to the AV node will be reduced, increasing the chances of a complete heart block.
Possible Complications When Diagnosed with Inferior Myocardial Infarction (Heart Attack)
Possible Heart Problems:
- Cardiogenic shock – a serious condition where your heart can’t pump enough blood to meet your body’s needs
- Atrioventricular block – this is when the electrical signals between the chambers of your heart are blocked
- Need for pacing – this is when your heart needs help to maintain a regular rhythm, often through a pacemaker
- Ventricular fibrillation – a life-threatening heart rhythm problem where the heart beats with rapid, erratic electrical impulses
Recovery from Inferior Myocardial Infarction (Heart Attack)
Cardiac rehabilitation is a crucial part of recovery. It’s also important to control blood pressure, decrease cholesterol and blood sugar levels, and maintain a healthy body weight. These steps can contribute to better heart health.
Preventing Inferior Myocardial Infarction (Heart Attack)
It’s important to stop smoking for better overall health. Additionally, incorporating a healthy diet into your daily routine can improve your wellness. Regular exercise should also be part of your lifestyle to maintain good health and fitness.