What is Junctional Rhythm?
The sinoatrial node, known as the SA, works as your heart’s natural pacemaker. It is tucked under the outer layer of the heart surface and takes the shape of a crescent. There is another structure called the atrioventricular node or AV, which sits in the lower part of the right atrium of the heart. This is in an area near the opening of the vein that collects oxygen-depleted blood (coronary sinus ostium), a band of fibrous tissue (the tendon of Todaro), and the wall of the heart between two chambers (the septal tricuspid valve annulus). This region is often called the “triangle of Koch”.
Just like every other organ, these nodes need blood supply to work. The SA node gets blood from an artery that usually branches off from the right coronary artery (about 60% of the time) or from the left circumflex coronary artery (in around 40% of the cases). For the AV node, the blood is primarily supplied by a branch of the right coronary artery or sometimes from the left circumflex artery. Another artery that supplies blood to the AV node is a branch of the left anterior descending artery.
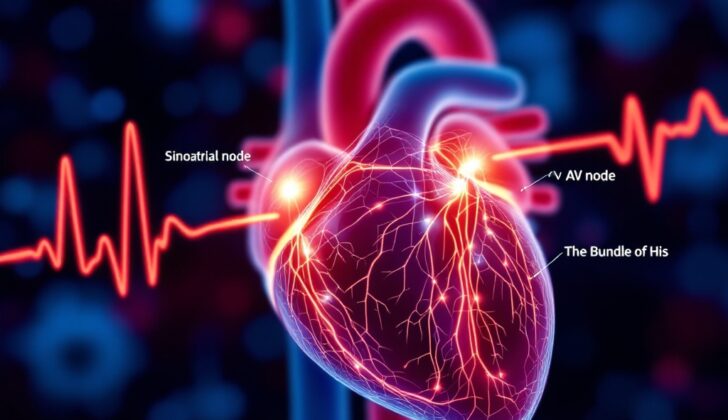
Normally, the SA node starts each heartbeat. This electric signal travels through the heart’s upper chambers (atria) to the AV node and from there it reaches the Bundle of His, a bundle of fibers that play a part in the electrical conduction system of the heart. These signals then move to the lower chambers of the heart (ventricles) through a network of fibers called the Purkinje fibers.
Sometimes, however, the heart can beat originating from the AV node or this Bundle of His located near where the upper and lower heart chambers meet. This is called a junctional rhythm. Depending on the rate of this rhythm, it’s referred to differently:
* Junctional bradycardia: less than 40 beats per minute
* Junction escape rhythm: 40 to 60 beats per minute
* Accelerated junctional rhythm: 60 to 100 beats per minute
* Junctional tachycardia:-more than 100 beats per minute
What Causes Junctional Rhythm?
The electrical activity in your heart, more specifically in the SA node, can sometimes be blocked or weakened. This can lead to what’s known as a “junctional rhythm”. Many medical conditions or medications can be responsible for this change in heart rhythm. These can include things like trauma to the chest, heart disease, illnesses affecting the connective tissue of the body, radiation therapy, or side effects from certain medications.
Certain conditions and medications that can affect heart rhythm are:
* Chest injuries
* Sick sinus syndrome – a condition where the heart’s natural pacemaker isn’t working right
* Radiation therapy – treatment often used for cancer
* Collagen vascular disease – disorders that involve your connective tissues
* Myocarditis – inflammation of the heart muscle
* Some medications like Clonidine, Reserpine, Adenosine, and Cimetidine
* Heart rhythm controlling drugs (antiarrhythmics) from class I to IV
* Lithium – often used in mental health treatment
* Amitriptyline – another medicine used in mental health
* Different types of muscular and inherited disorders
* Very intense vagus nerve stimulation like during endotracheal suctioning
* Certain heart rate controlling drugs like beta-blockers, calcium channel blockers, Digoxin, and Ivabradine
* Opioids and cannabinoids, which are types of drugs
* Some conditions like underactive thyroid (hypothyroidism), sleep apnea, low oxygen levels (hypoxia), high brain pressure (intracranial hypertension), high potassium levels in the blood (hyperkalemia), anorexia nervosa, protein build-up in organs (amyloidosis), heart lining inflammation (pericarditis), and specific infectious diseases like Lyme disease and rheumatic fever
* Drug-induced heart rhythm disturbance due to Digoxin, for example
* Conditions affecting the supply of blood to heart muscle like coronary artery disease or conditions after repairing a congenital heart disease.
Also, having a severely diseased SA node can cause a junctional rhythm, as well as conditions that completely or partially block the electrical signals in the heart, such as a high-grade second-degree heart block and a third-degree heart block.
Risk Factors and Frequency for Junctional Rhythm
Junctional rhythm, a particular type of heartbeat, is often found in individuals struggling with sinus node dysfunction (SND). Roughly 1 in every 600 heart patients over 65 in the United States suffers from SND. This rhythm may also occasionally appear in patients with sick sinus syndrome, young kids, and athletes with a higher vagal tone, especially while they’re asleep. Both men and women have an equal chance of experiencing a junctional rhythm.
Signs and Symptoms of Junctional Rhythm
People with a condition known as “junctional rhythm” may experience various symptoms or sometimes none at all. The symptoms one experiences depend largely on what’s causing the junctional rhythm in the first place. For example, someone with worsened heart failure might feel short of breath, wheeze, and have swelling in their lower legs. On the other hand, someone with rheumatic fever might experience symptoms such as a fever, joint pain, a skin rash and also possess a heart murmur due to damaged heart valves.
In addition to these, some people may experience more general symptoms like dizziness, fatigue, fainting or near fainting, and occasional heart palpitations. During a physical examination, the doctor might notice visible vein pulsations and a regular heart rate that can range anywhere from 20 to over 100 beats per minute.
Testing for Junctional Rhythm
If you show signs of junctional rhythm, a type of abnormal heart rhythm, your doctor will start with a thorough assessment. This will include a review of your medical history and a physical exam. They’ll check your vital signs which include your breathing rate, blood pressure, body temperature, and heart rate. They’ll also review all the medications you’re currently taking and perform an electrocardiogram (ECG), which is a test that records the electrical activity of your heart.
During this assessment, your doctor will determine if your heart is able to pump enough blood to meet your body’s needs, a condition known as being hemodynamically stable. They’ll also check for any signs of heart disease or heart failure, as these conditions can be connected to junctional rhythm.
Your doctor might also order some additional tests. These could include thyroid function testing (as thyroid issues can affect the heart), pulmonary function testing (which measures how well your lungs are working), routine blood work, and an echocardiogram (an ultrasound of the heart). All these tests will help your doctor better understand what’s causing your symptoms and how best to treat you.
Treatment Options for Junctional Rhythm
The primary goal of treating a junctional rhythm, a specific heart rhythm that originates in a part of the heart called the junction, depends on what’s causing this rhythm in the first place. For example, if the junctional rhythm is happening due to a problem with the sinus node (a natural pacemaker in your heart) resulting in a very slow or absent pulse, it should be left alone since it’s keeping the heart beating in such cases.
Therefore, before deciding on a treatment plan for a patient with a junctional rhythm, it’s crucial to figure out what’s causing this rhythm first. However, healthy people who have this rhythm and aren’t experiencing any symptoms might not require any treatment at all. Typically, they might have this rhythm because they have a strong vagal tone that suppresses the SA node’s automaticity or natural rhythm.
In the event a patient is experiencing toxicity from a drug called digoxin, they would be treated with a medicine called atropine and an antibody specifically made for digoxin. If these treatments don’t work and a patient’s heart rate speeds up excessively, a medicine called intravenous phenytoin could be used in a monitored setting. This is because these patients can run the risk of developing low blood pressure.
In the case of children, ongoing junctional tachycardia (a rapid heart rhythm) with symptoms indicates the need for a procedure called percutaneous radiofrequency ablation, which essentially heats up the part of the heart causing the abnormal rhythm to rectify it.
Finally, patients with conditions like sick sinus syndrome (a collection of heart rhythm disorders), or advanced heart block (a serious condition where the signals from the upper part of the heart are blocked from reaching the lower part), may need a permanent pacemaker, which is a device implanted into your chest to help control your heartbeat.
What else can Junctional Rhythm be?
Doctors need to consider several conditions that can cause symptoms similar to the ones being experienced. These conditions include:
- Digoxin toxicity
- Atrioventricular nodal reentrant tachycardia
- Atrioventricular reentrant tachycardia
- Sinus node dysfunction
- High-grade second-degree heart block
- Third-degree heart block
What to expect with Junctional Rhythm
The outlook is generally positive when a healthcare provider is able to quickly identify the rhythm of the heart.
Possible Complications When Diagnosed with Junctional Rhythm
If not quickly recognized, symptoms like fainting, tiredness, or lightheadedness can develop. These could lead to further complications.
Preventing Junctional Rhythm
It’s beneficial for patients to have educational resources that they can easily understand and access. If possible, this education can be given through means that the patient is already familiar with, such as using online sources or reading materials like brochures.