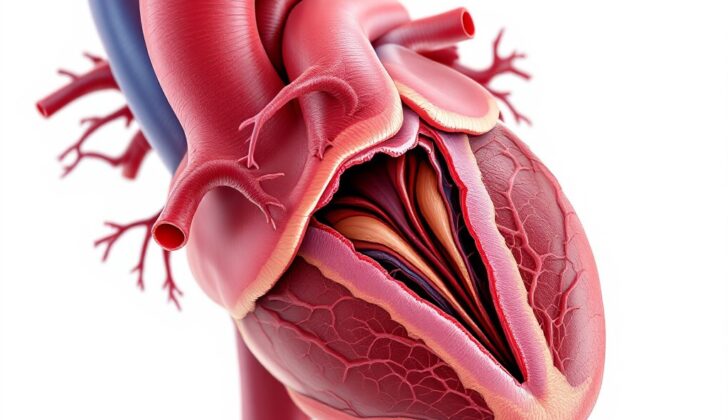
What is Left Ventricular False Aneurysm?
A left ventricular false aneurysm, also known as a pseudoaneurysm, is a rare and serious heart condition. This typically occurs as a complication from a heart attack. This situation happens when a part of the heart’s wall, weakened from lack of oxygen during a heart attack, ruptures and the resulting blood clot, called hematoma, is contained and connected with the heart’s main pumping chamber, or ventricle.
This rupture can sometimes be sealed by the heart’s outer lining, the pericardium, or by a blood clot, scar tissue, or a mass of tissue that forms while an injury, such as a rupture, is healing. This sealing gives it the appearance of an aneurysm, which is a bulge in the wall of a heart artery or other artery. The wall of the false aneurysm is made up only of scar or fibrous tissue and the pericardium, failing to have the full layers of the ventricle – the inner lining or endocardium, and the heart muscle or myocardium.
These pseudoaneurysms usually form in the back and side walls of the heart and display a more constricted neck in comparison to the rest of the sac of the aneurysm. These fake aneurysms are also more likely to rupture, making swift diagnosis and treatment vital.
What Causes Left Ventricular False Aneurysm?
Being an older woman, having a history of high blood pressure, and not having extra blood vessels to bypass blockages during a heart attack, are all factors that can increase the risk of developing a type of abnormal bulge in the wall of the main pumping chamber of the heart, known as a false aneurysm. Such abnormal bulges usually occur due to a weakness in the heart wall following a severe heart attack, which affects the entire thickness of the heart wall.
There are several other things that might cause these abnormal bulges in the heart. These include having heart surgery, an injury to the chest, being born with a heart defect, having a tumor that has spread to the heart, and in rare cases, having an infection of the inner lining of the heart. If you’ve had a heart attack and it mainly damaged the lower part of your heart, you’re twice as likely to develop a false aneurysm compared to if the heart attack mainly affected the front wall of your heart. This is likely because the bottom part of your heart is thinner.
Heart surgery is the second leading cause of false aneurysms. Among different types of heart surgeries, those involving the mitral valve (one of the heart’s four valves) are most likely to lead to a false aneurysm. This is followed by surgeries for congenital heart diseases and diseases of the aortic valve (another one of the heart’s valves).
False aneurysms can also occur after procedures to replace the aortic valve done through small incisions in the chest or groin, or following a blunt or penetrating injury to the chest. Some people are born with heart defects that can cause an aneurysm in the area below the mitral and aortic valves. This happens because the part of the heart that these valves are attached to is not as strong.
Less commonly, conditions such as tuberculosis, syphilis, rheumatoid arthritis, Kawasaki disease (a rare condition in children that causes inflammation of the blood vessels), and Behcet’s syndrome (a rare disease that causes blood vessel inflammation) can also lead to the development of these abnormal bulges in the heart.
Risk Factors and Frequency for Left Ventricular False Aneurysm
Left ventricular false aneurysm is a rare heart condition. It happens in only 0.1% of people who’ve had a heart attack and in 0.8% of people after undergoing a certain type of heart surgery (mitral valve replacement). One research found that the average age of individuals who presented with this condition was 60 years old. These individuals were mostly white (75%) and male (67%). Without treatment, left ventricular false aneurysms pose a 30-45% risk of rupture.
Signs and Symptoms of Left Ventricular False Aneurysm
Patients may display a variety of non-specific symptoms, and around 10% may not show any symptoms at all. Some common indications include chest discomfort, heart palpitations, shortness of breath, and fainting spells. Other potential symptoms can be less direct, such as a cough, a fever, dizziness, pain in the shoulder or back, difficulty swallowing, heart failure, and even stroke. Doctors may also find indicators through physical exams, but these are not typically specific. Some of these signs can include a slow heartbeat, low blood pressure, decreased heart sounds, sound of friction from the pericardium (the sac surrounding the heart), and murmurs. There can be indications of irregular heartbeat, heart failure, and even tamponade (pressure on the heart due to fluid accumulation) caused by a ruptured false aneurysm. It’s also important to evaluate trauma patients for myocardial contusion (heart bruise), as it can often go unnoticed.
- Chest discomfort
- Heart palpitations
- Shortness of breath
- Fainting spells
- Cough
- Fever
- Dizziness
- Shoulder or back pain
- Difficulty swallowing
- Signs of heart failure or stroke
- Slow heartbeat
- Low blood pressure
- Decreased heart sounds
- Sound of friction from the pericardium
- Indications of irregular heartbeat, heart failure, or tamponade
Testing for Left Ventricular False Aneurysm
If your doctor thinks you might have a false aneurysm in your heart’s left ventricle, they will often start with a test called a transthoracic echocardiography. This test can show if there’s a sudden break in the internal lining (endocardium) of your heart leading into a sac, which suggests an aneurysm. It can also detect a ratio of more than 0.5 between the opening into the aneurysm and the size of the aneurysm itself. Additionally, it may show a connection between the aneurysm and a pouch in the ventricle, and can illustrate the flow of blood from the ventricle into the aneurysm during the heart’s contraction phase (systole).
However, the best test for diagnosing a false aneurysm is an angiography of the left ventricle and coronary arteries. During this test, a false aneurysm appears as a narrow opening leading into a wider sac-like space. Also, no coronary arteries (the blood vessels that supply the heart muscle) are seen near the aneurysm. In most cases, an angiography can diagnose a false aneurysm, unless there isn’t enough contrast (a dye used to make structures inside your body more visible) or the x-ray image isn’t at right angles to the aneurysm.
Another tool your doctor may use is cardiac magnetic resonance imaging. This test is powerful as it can show that there’s no inner lining or heart muscle along with the aneurysm. It’s also good for assessing how well your heart is working in terms of function, contraction, blood flow in the heart, and movement of blood within the aneurysm.
Computed tomography (CT) can also be helpful. It can clearly show how the heart wall suddenly ends at the boundary of the aneurysm and can provide valuable images of the coronary arteries and any bypass grafts, which are important for planning a repeat operation in patients with a false aneurysm.
In the operating room, your surgeon may use transesophageal echocardiography to look at the location and size of the aneurysm, check for any blood clots (thrombus) and see if other structures in the heart are affected. It can also show the two-way, irregular blood flow between the left ventricle and the aneurysm sac. Additionally, an X-ray of your chest can reveal any abnormal shapes in the midline of your chest due to the aneurysm. In rare cases, if the false aneurysm has been there for a long time, it may develop calcium deposits that can be seen on an X-ray. Finally, your doctor may use an electrocardiogram to detect any vague changes or inverted T-waves (a part of the EKG tracing), particularly in the lower or outer leads.
Treatment Options for Left Ventricular False Aneurysm
Surgery is the only certain treatment for left ventricular false aneurysms, a type of heart condition. The aim of this operation is to remove the aneurysm and restore the size and shape of the left ventricle, a main pumping chamber in the heart. The surgery is typically conducted through a median sternotomy, an incision made down the middle of the chest. It involves using a heart-lung machine (cardiopulmonary bypass) to take over the heart’s functions during the procedure and placing a clamp on the aorta, the largest artery in your body.
Many different repair techniques have been documented, but they all focus on removal or exclusion of the aneurysm and restoring the normal shape of the left ventricle. One such method involves cutting open the aneurysm, removing any blood clot (thrombus) inside it, and trimming away diseased tissue until only healthy heart muscle (myocardium) remains. Afterward, a patch made from a synthetic material called Dacron is cut to a size larger than the damage in the heart. This patch is stitched into place to cover the affected area. The stitches are carefully placed in generous amounts of healthy tissue to ensure a secure patch. An additional layer of stitches may be added to better control bleeding.
For individuals who are not good candidates for surgery, a minimally invasive procedure called percutaneous embolization can be considered as an option. However, this method is not suitable for those with an active infection of the heart lining (endocarditis) or a blood clot in the left atrium, a different chamber of the heart. This procedure involves threading a catheter (a long, thin tube) through an incision in the groin, up to the left atrium of the heart, and into the aneurysm. Embolization coils are then directed into the aneurysm to close it off, or a special kind of plug called an Amplatzer vascular plug is used to seal the communication site between the left ventricle and the aneurysm.
Follow-up checks are crucial to monitor the progression of false aneurysms. Research suggests patients who have small-sized aneurysms (less than 3 cm) and no symptoms or those who are not fit enough for surgery can be managed medically. This involves taking medications known as beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and anti-platelets and/or anticoagulants to reduce the risk of blood clots. In patients waiting for surgical treatment, these medications are adjusted (optimized) to help prevent the aneurysm from rupturing. Specifically, ACE inhibitors help reduce heart stress by lowering the pressure against which the heart must pump blood (afterload).
What else can Left Ventricular False Aneurysm be?
When dealing with what seems to be a false aneurysm in the heart’s left ventricle, doctors will also consider two other conditions: a true aneurysm and a left ventricular diverticulum. These do have some similarities that could lead to confusion, but there are also differences important in deciding on the best course of action.
- True aneurysm: This is a common complication seen in 10% to 35% of patients following a heart attack. It can be difficult to tell apart from a false aneurysm before surgery, but a notable difference is that a true aneurysm contains all three layers of the heart muscle wall. Unlike a false aneurysm, true aneurysms are not as prone to breaking and can be managed with medication or surgical treatment. During surgery, these aneurysms can be seen completely caving in during left ventricular decompression.
- Left ventricular diverticulum: A very rare occurrence (only 0.42% prevalence in adults), this heart abnormality forms mostly due to infection or trauma, although it can also be present at birth. Seen on a specific type of ultrasound as a bird-beak-shaped cavity coming from the left ventricle, it varies greatly in size, ranging from 5 to 90 mm. This condition can be managed conservatively in symptom-free patients, while surgical intervention is an option for those who are symptomatic.
What to expect with Left Ventricular False Aneurysm
A false aneurysm is a type of heart condition and due to its inherent fragility, the irregular movement of the heart can lead to serious problems like irregular heart rhythms, clot formation, and even heart failure. If left untreated, a false aneurysm can lead to the rupture of the sac-like structure that forms around it.
Patients who have undergone surgical repair for this condition are found to have increased survival rates and symptom improvement. Owing to enhancements in surgical techniques, less invasive medical interventions, and better patient care management, the number of deaths during or immediately after the operation is almost around 10%.
However, it’s important to note that some patients have survived with medical management alone. In these cases, strict control of blood pressure, use of blood-thinning medication (anticoagulation) and expert management of heart failure are extremely crucial.
In some rare instances, long-term survival has also occurred with the spontaneous closure of the neck of the false aneurysm.
Possible Complications When Diagnosed with Left Ventricular False Aneurysm
The most dreaded complication of treating a false heart aneurysm with medicine is the bursting of the aneurysm. For those who survive this method of treatment, a stroke is another major concern, often as a result of clots inside the aneurysm.
Following heart surgery, patients can experience complications that are common in complex open-heart procedures. These include death, bleeding, irregular heartbeat, stroke, and infection. In rare cases, some patients might develop recurring false aneurysms, assumedly due to an inadequate placement of the surgical patch on healthy heart muscle or when the patch is stitched to the aneurysm.
Other post-surgery complications can occur if there is a large reduction in the left ventricle’s volume, which is the heart’s major pumping chamber.
Complications from a particular approach called the transcatheter method to close the false aneurysm can also arise. These may include bleeding, the formation of large bruises from broken blood vessels, and infections at the site of the leg incision. Moreover, the catheter itself could pierce the heart wall and cause new rhythm disturbances, leading to the need for pacemakers.
Common Complications:
- Bursting of the aneurysm
- Stroke
- Death
- Bleeding
- Irregular heartbeat
- Infection
- Recurring false aneurysms
- Complications from reduction of left ventricular volume
- Bleeding from the femoral incision
- Bruises from broken blood vessels
- Heart wall perforation
- New rhythm disturbances requiring pacemakers
Preventing Left Ventricular False Aneurysm
It’s important for patients who have experienced a heart attack (also known as MI or myocardial infarction) or have had heart surgery, to continue regular visits with their doctors afterwards. These doctors can monitor their health and response to the event or surgery. Patients should be aware of any new or lasting chest pain, changes in their energy levels, the start of irregular heartbeats (palpitations), or if they notice their overall health or physical fitness deteriorating.
In some instances, vague symptoms such as arm, back or upper stomach (epigastric) pain that doesn’t go away after a heart-related event, might be experienced. If any of these symptoms occur, patients should seek further medical evaluation. It’s essential to note that these symptoms could be signs that their health is not improving as expected, and further steps might need to be taken.