What is Mitral Valve Prolapse?
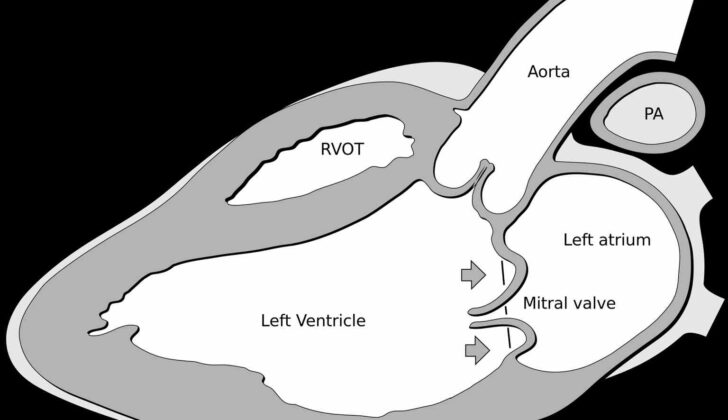
Mitral valve prolapse (MVP) is a condition where the heart’s mitral valve doesn’t function properly. This valve is found in the heart, and its job is to keep the blood flowing in one direction. However, in MVP, sometimes known as floppy mitral valve syndrome or systolic click-murmur syndrome, the valve becomes excessively thick and can collapse backwards. As a result, the valve doesn’t close properly during each heartbeat (a cycle called systole). This condition is usually harmless, but in some rare cases, it can potentially lead to serious health issues like sudden cardiac death, infection of the heart lining (endocarditis), or a stroke.
MVP affects close to 3% of people in the United States. It is usually discovered during routine medical check-ups when the doctor listens to your heart with a stethoscope. An ultrasound of the heart (echocardiography) is used to confirm the diagnosis. MVP is also the main reason for non-ischemic mitral valve problems – conditions that are not caused by reduced blood supply to the heart – in the US.
If MVP causes symptoms, the doctor might suggest a procedure to repair the mitral valve.
What Causes Mitral Valve Prolapse?
Mitral valve prolapse (MVP), a condition where the heart’s mitral valve doesn’t work properly, often happens on its own in disorders affecting the body’s connective tissues. Examples of these disorders include Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta, pseudoxanthoma elasticum, and aneurysms-osteoarthritis syndrome.
Risk Factors and Frequency for Mitral Valve Prolapse
Mitral Valve Prolapse (MVP) is a common condition affecting the heart valves, impacting up to 3% of the population. This amounts to about seven to eight million people in the United States and over 16 million worldwide. There are two types of MVP: primary and secondary.
- Primary MVP is characterized by changes in the heart valve, known as myxomatous degeneration, without any associated connective tissue disease.
- Secondary MVP can be linked to a variety of conditions such as Ehler-Danlos Syndrome, Marfan syndrome, Polycystic kidney disease, Graves’ disease, and Pectus excavatum. It may be associated with notable heart valve leakage (4%), heart infections, heart failure, and even sudden death.
MVP can be due to different genetic factors, which may occur spontaneously or run in families. There are several known affected chromosomes linked with MVP, including MMVP1 – chromosome 16p11.2-p12, MMVP2 – chromosome 11p15, and MMVP3 – chromosome 13q31.3-q32. Less frequently, it may be due to a mutation on the X chromosome, with specific mutations including P637Q, G288R, and V711D, or a specific 1944 base pair deletion.
Signs and Symptoms of Mitral Valve Prolapse
Mitral valve prolapse, or MVP, is a condition that sometimes doesn’t cause any noticeable symptoms. However, when symptoms do occur, they can include unusual chest pain, a rapid heartbeat, difficulty breathing while doing physical activity, and having a low tolerance for exercise. Some people may also experience anxiety, low blood pressure, fainting, and issues related to the autonomic nervous system, which controls functions like heart rate and digestion. In some cases, a type of irregular heartbeat known as a supraventricular arrhythmia might be observed, indicating that the nervous system might be overly active.
One key sign of MVP is a particular sound, heard with a stethoscope, that the heart makes when it beats. This sound, called a mid-systolic click, comes right before a late systolic murmur, which is a specific kind of humming sound that happens later in the heartbeat. Unlike the constant hum of a normal heartbeat, the murmur of MVP changes depending on the body position; it becomes stronger when the person is standing or straining during the Valsalva maneuver, and weaker when the person is squatting.
It’s important to note that the murmur of MVP can sound similar to the murmur of a heart condition called hypertrophic cardiomyopathy, making it crucial for doctors to perform the right tests for a precise diagnosis. One diagnostic test is the handgrip maneuver where the grip strength has a distinct effect on the murmur and the timing of the mid-systolic click in MVP.
Over time, MVP patients have been observed to experience a variety of symptoms related to the autonomic nervous system.
- Panic attacks
- Anxiety
- Difficulty tolerating exercise
- Rapid heartbeat
- Tiredness
- Unusual chest discomfort
- Orthostasis (feeling lightheaded when standing up)
- Mood changes
- Fainting
Testing for Mitral Valve Prolapse
The best way to diagnose Mitral Valve Prolapse (a heart condition where one of the heart’s valves doesn’t work properly) is by using an echocardiogram, which creates a detailed image of your heart. There’s a specific type of echocardiogram called M-Mode echocardiogram, but it’s not usually used to diagnose this condition since the normal movement of the base of your heart can mimic or obscure the symptoms of Mitral Valve Prolapse. Using a two- or three-dimensional echocardiogram is better because it can measure the thickness of your heart’s leaflet (the thin flaps of tissue that make up the heart’s valves) and respectively compare it to the annulus (the base of the heart’s leaflet).
Mitral Valve Prolapse is diagnosed when the heart’s valve displacement is more than 2 mm above the annulus in a long-axis view (viewed from the side or front). We can further classify Mitral Valve Prolapse into two types: non-classic and classic based on the thickness of the heart’s leaflets.
Non-classic Mitral Valve Prolapse means your heart’s leaflet thickness is 0 mm to 5 mm. In contrast, classic Mitral Valve Prolapse is when your heart’s leaflet thickness is more than 5 mm.
We can further break down classic Mitral Valve Prolapse into symmetric and asymmetric types based on where the leaflet tips meet the annulus. In the symmetric form, the tips of your leaflets meet at the same point on the annulus, whereas in the asymmetric form, one leaflet is pushed further into the atrium (the upper chambers of the heart) than the other.
Classic asymmetric Mitral Valve Prolapse can also be categorized into flail and non-flail types. In the flail type, the leaflet tip flips outward, curving towards the left atrium. This can lead to a deterioration of the mitral valve and the condition varies from the leaflet tip turning over to chordal rupture. Because these terms might sound a bit medical – think of it as the valve’s “strings” not being tightly tethered and flopping, which is why we call it the “flail leaflet”. This subtype is more likely to lead to mitral regurgitation (when the heart’s valve leaks blood).
CMR (Cardiovascular Magnetic Resonance imaging) provides a clear picture of the heart but hasn’t been evaluated in patients with Mitral Valve Prolapse. It can help quantify mitral regurgitation before undergoing surgery on the mitral valve.
Occasionally, Mitral Valve Prolapse is discovered incidentally during a cardiac catheterization (which is a procedure used to diagnose and treat certain heart conditions) on a test called left ventriculography. This test shows the displacement of mitral valve leaflets into the left atrium of the heart and late systolic mitral valve regurgitation (the condition when blood leaks backwards in the heart after every heartbeat). In this case, an evaluation by echocardiography is necessary. If there is a mismatch between your symptoms and echo findings regarding the severity of mitral valve regurgitation, then additional tests like cardiac catheterization and left ventriculography may be useful.
Treatment Options for Mitral Valve Prolapse
People with mitral valve prolapse (MVP – a condition where one of the heart’s valves doesn’t work properly) who don’t show any symptoms often don’t need treatment.
However, if they do experience symptoms such as chest pain or heart palpitations, medications known as beta-blockers (for example, propranolol) can help manage these issues.
In severe cases of MVP where there is significant leakage of the mitral valve (known as mitral regurgitation), a surgical procedure to repair or replace the faulty valve may be needed. It’s recommended that this surgery is carried out before symptoms of fluid build-up in the lungs due to poor heart function (congestive heart failure) develop.
It’s important to note that people with MVP have a greater risk of developing a heart infection known as bacterial endocarditis. Although previously, the American Heart Association (AHA) suggested taking antibiotics before any invasive procedures (like dental surgery), they now only recommend this for individuals with specific heart conditions that place them at higher risk of serious issues from bacterial endocarditis.
The likelihood of having a stroke in people with MVP is relatively low. Guidelines from heart health organizations don’t provide specific advice about the use of medication to prevent blood clotting (antiplatelets or antithrombotics) for MVP patients. However, it’s suggested that aspirin might be beneficial for those with unexplained temporary disruption of blood supply to the brain (transient ischemic attacks), particularly if there are signs of high-risk MVP through heart scans. Blood-thinning medication is recommended if blood clots have already occurred or if transient ischemic attacks keep happening despite aspirin treatment.
People with MVP who don’t show symptoms are usually managed with basic observation and regular monitoring. Those with no leakage at the mitral valve are typically reviewed every 3 to 5 years, while those with leakage are generally seen yearly. A healthy lifestyle and regular exercise are important, and any palpitations, anxiety, or chest pain should be investigated further to rule out other conditions.
In cases where there’s severe mitral valve leakage along with heart function issues (systolic heart failure), surgery might be required – this also applies to individuals without symptoms but who have MVP along with systolic heart failure. The preferred surgical procedure is to repair rather than replace the mitral valve. For patients with other significant health conditions who aren’t suitable for surgery, a less invasive procedure to repair the mitral valve may be considered.
The AHA also provides advice for athletes with MVP. Those involved in high-intensity competitive sports can usually participate based on their medical history. They can participate if they haven’t had previous episodes of fainting, abnormal heart rhythms, severe mitral valve leakage, blood clots, reduced heart function, or family history of sudden death related to MVP. Athletes with these conditions can still participate in low-intensity competitive sports.
What else can Mitral Valve Prolapse be?
Doctors need to distinguish between MVP (Mitral Valve Prolapse) and other conditions that can also cause leakage from the mitral valve, also known as mitral valve regurgitation.
What to expect with Mitral Valve Prolapse
In general, MVP (Mitral Valve Prolapse) is not a harmful condition. Many people who have MVP aren’t even aware of it and don’t need treatment. However, there can be some complications linked to this condition, which include infective endocarditis (an infection of the inner lining of your heart), mitral valve regurgitation (a condition where the heart’s mitral valve doesn’t close tightly), arrhythmia (also known as atrial fibrillation, referring to irregular heartbeats), transient ischemic event (a temporary blockage of blood flow to the brain), or systemic embolism (when a blood clot travels through the bloodstream and blocks a blood vessel).
The main factor predicting mortality in MVP is the degree of mitral valve regurgitation, and ejection fraction (a measurement of the percentage of blood leaving your heart each time it contracts).
Possible Complications When Diagnosed with Mitral Valve Prolapse
Common Complications:
- Development of severe mitral valve leakage
- Heart valve infection
- Irregular heart rhythm, known as atrial fibrillation
- A stroke occurring due to blood clots
- Unexpected sudden death
Preventing Mitral Valve Prolapse
Patients with a condition known as Mitral Valve Prolapse (MVP) should reach out to their doctor if their symptoms get worse. MVP is a condition where the two valve flaps in the heart’s mitral valve don’t close smoothly or evenly. It’s beneficial for these patients to consider surgery before they develop a more serious condition called congestive heart failure, where the heart can’t pump blood effectively. So if the symptoms start to worsen, it is important not to delay seeking medical help.