What is Myocardial Infarction (Heart Attack)?
A myocardial infarction, often referred to as a “heart attack”, happens when the blood flow to part of the heart muscle is reduced or stops completely. Sometimes, myocardial infarctions can occur without any noticeable signs, or they can be severe events leading to sudden death.
A large number of heart attacks are due to coronary artery disease, which is the leading cause of death in the United States. This disease blocks the coronary arteries, preventing oxygen from reaching the heart muscle. If the heart muscle doesn’t receive oxygen for a long time, it can lead to the death and decay of the heart cells.
Patients with a heart attack may feel discomfort or pressure in their chest, which can spread to their neck, jaw, shoulder, or arm. Doctors can identify a heart attack through the patient’s medical history, a physical exam, changes in their electrocardiogram (ECG), and high levels of certain biological markers such as cardiac troponins in their blood.
What Causes Myocardial Infarction (Heart Attack)?
Myocardial infarction, also known as a heart attack, is closely linked to coronary artery disease, which affects the heart’s blood supply. An international study named INTERHEART identified several risk factors that can be changed to reduce the chances of getting coronary artery disease:
1. Smoking
2. High levels of certain blood fats (raised ApoB/ApoA1)
3. High blood pressure
4. Diabetes
5. Abdominal obesity (waist/hip ratio above 0.90 for men and above 0.85 for women)
6. Psychological stressors like depression, financial problems, life-changing events such as divorce or job loss, and family conflicts
7. Not eating fruits or vegetables daily
8. Lack of physical exercise
9. Alcohol use (though this has a weaker link and is somewhat protective)
In this study, these risk factors were tied to acute myocardial infarction (sudden heart attack), except for alcohol use, which had a slight link. Smoking and abnormal levels of certain fats in the blood were the most strongly associated with sudden heart attacks. The dangers posed by diabetes and high blood pressure were found to be greater in women. The positive effects of exercise and alcohol were also more significant in women.
Another risk factor for a heart attack is a moderately high level of a substance in the blood called homocysteine. This factor can be altered independently, and high levels can be treated with folic acid, vitamin B6, and vitamin B12.
There are also some risk factors for a heart attack that cannot be changed. These include being older, being a man (men tend to have heart attacks earlier in life), and having a genetic disposition (increased risk if an immediate family member had cardiovascular problems before reaching 50). The role of particular genes that increase the risk for a heart attack is being actively studied.
Risk Factors and Frequency for Myocardial Infarction (Heart Attack)
Coronary artery disease, a heart condition, is the leading cause of death and disability both in western countries and throughout the world. According to data from 2015, the disease caused over 114,000 deaths in which it was the main driver, and was mentioned as a contributing factor in over 151,000 deaths.
Based on information gathered between 2011 and 2014, it’s estimated that 16.5 million American adults over the age of 20 suffer from coronary artery disease. The prevalence of the disease was found to be higher in males than females across all age groups. Overall, about 3.0% of adults in the United States over 20 have had a heart attack, a common consequence of coronary artery disease.
Certain demographic groups in the US experience different rates of heart attacks:
- Non-Hispanic Whites: 4.0% in males, 2.4% in females
- Non-Hispanic Blacks: 3.3% in males, 2.2% in females
- Hispanics: 2.9% in males, 2.1% in females
- Non-Hispanic Asians: 2.6% in males, 0.7% in females
Data collected between 2005 and 2014 suggests about 605,000 new heart attacks and 200,000 recurrent heart attacks occur each year. The average age for a first heart attack is 65.6 years for males and 72.0 years for females. However, studies show a declining trend in heart attack incidence in the US over the past years.
Signs and Symptoms of Myocardial Infarction (Heart Attack)
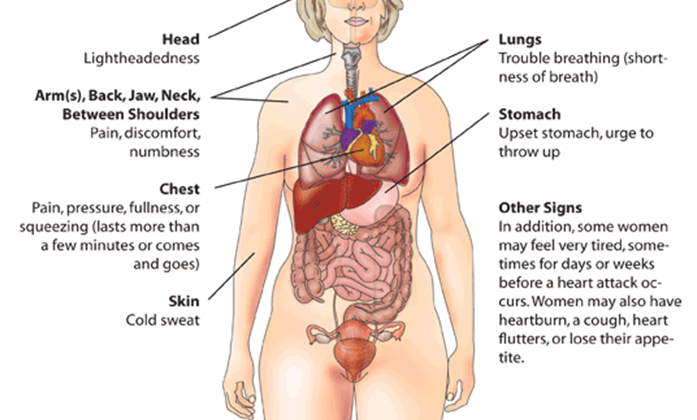
Myocardial ischemia is a condition caused by an imbalance between the supply and demand of oxygen in the heart. This could sometimes result in a heart attack. To identify this condition, doctors usually look at a patient’s medical history, EKG results, and certain blood markers. Symptoms of myocardial ischemia often include chest pain, discomfort in the upper arm, jaw, or upper abdominal area, which can happen during physical activities or while resting. This condition may also manifest as shortness of breath or fatigue, these are known as ischemic equivalents. Chest pain usually feels like a heavy pressure behind the breastbone.
The pain often spreads to the left shoulder, neck, or arms without any clear triggers and may come and go or remain constant. It usually lasts more than 20 minutes and doesn’t get better with changing position or moving. Additional symptoms might include sweating, nausea, abdominal pain, shortness of breath, and fainting. Heart attacks may also have less common or atypical presentations, like heart palpitations, cardiac arrest, or sometimes, no symptoms at all.
- Chest pain or discomfort in the upper arm, jaw, or upper abdominal area
- Shortness of breath
- Fatigue
- Pain radiating to the left shoulder, neck, or arms
- Persistent or intermittent pain lasting more than 20 minutes
- Sweating
- Nausea
- Abdominal pain
- Dizziness or fainting
- Atypical presentations like heart palpitations, cardiac arrest, or lack of symptoms
Testing for Myocardial Infarction (Heart Attack)
When it comes to assessing a heart attack, or myocardial infarction (MI), doctors consider three key factors: the patient’s symptoms, findings from an electrocardiogram (ECG), and levels of specific proteins in the blood known as cardiac biomarkers.
The ECG test records the electrical activity of the heart and is usually the first tool used to help diagnose a heart attack. It should ideally be performed within 10 minutes of the patient arriving in the emergency department. The ECG can show any abnormal changes in the heart’s activity and is often performed several times to track these changes.
Specific signs on the ECG, such as elevation or depression in the ST-segment, might suggest that a coronary artery is blocked. However, an ECG alone is not enough to diagnose a heart attack as several other health conditions, such as pericarditis and Brugada syndrome, can cause similar ECG changes.
Cardiac biomarkers are proteins found in the heart muscles, and their levels rise in the blood when these muscles are damaged, like during a heart attack. The two most important ones are troponin I and troponin T. Even though high levels of these proteins may not pinpoint the exact cause of heart damage, a pattern of rising and falling troponin levels with at least one reading above the normal limit, along with symptoms of a heart attack, suggest that a heart attack has occurred. Troponin levels are often measured several times over six hours to assess the severity and timing of the heart injury.
Imaging tests, like echocardiography, radionuclide imaging, and cardiac MRI, can also provide valuable insights into a heart attack. They can show how well the heart muscles are working, whether any heart tissue has been damaged or scarred, and the impact of this damage on the heart’s function.
Treatment Options for Myocardial Infarction (Heart Attack)
If someone is experiencing symptoms of severe chest pain that lasts less than 12 hours and they have consistent ST-segment elevation on an EKG, they should be given reperfusion therapy. This means that if a facility can, they should perform a procedure to unblock their coronary artery within two hours of getting the EKG diagnosis. If this isn’t possible, the patient should be given medication to dissolve the blood clot within ten minutes of confirming that it is a heart attack and that there would be no harm in taking the medication. After that, if they can be taken to a facility where the procedure can be done within 60 to 90 minutes, it should be carried out there. Otherwise, they may need to have a rescue procedure planned. The preferred medications for this are tenecteplase, alteplase, or reteplase.
Pain, breathlessness, and uncomfortable or scary feelings can be managed with opioids like morphine. Even though studies suggest that morphine may lead to a higher risk of death and other adverse effects, no negative issues have been found when it is used for a certain type of heart attack. To manage feelings of fear or intense discomfort, a mild drug to decrease these feelings can be considered. Patients who have low blood oxygen levels should be given additional oxygen.
When it comes to relieving symptoms and regression of ST depression, a condition where the EKG shows less blood is reaching the heart, intravenous nitrates work better than sublingual nitrates. The dose of this should be increased until the symptoms are gone, the blood pressure of patients with high blood pressure is brought back to normal, or there are no side effects such as headaches or low blood pressure.
Beta-blockers are drugs that can decrease the amount of oxygen the heart needs by lowering the heart’s workload. However, they should not be used if the patient has coronary vasospasm, which is when the coronary arteries tighten.
Blood thinners like aspirin are usually recommended for both STEMI and NSTEMI. An oral starting dose of 150 to 300 mg and a continued daily dose of 75 to 100 mg are recommended for long-term use. Aspirin is effective throughout the lifespan of the blood platelets and helps prevent blockages.
Clopidogrel, prasugrel, and ticagrelor, all of which are P2Y12 inhibitors, are good options too. While clopidogrel requires a 300 to 600 mg starting dose followed by a 75 mg daily dose, prasugrel requires a 60 mg starting dose and a 10 mg daily dose.
For patients undergoing angioplasty, a combined treatment of blood thinners with aspirin and a P2Y12 inhibitor is recommended. If a patient is allergic to heparin, an anticoagulant like bivalirudin is recommended.
In the long term, high-intensity statins, or cholesterol-lowering drugs, are recommended to lower bad cholesterol and stabilize blockages in the arteries. Aspirin is also recommended for lifelong use in these patients. Other medications depend on the kind of treatment procedure the patient had. For example, patients with hypertension, heart failure, or diabetes should take ACE inhibitors. Patients with a low LVEF should take beta-blockers. To keep blood pressure less than 140/90 mm Hg, antihypertensive therapy is recommended.
Lifestyle modifications can also help with long-term management. Stopping smoking is the most effective way to avoid another heart attack. Regularly consuming a diet low in saturated fat and high in whole grain products, vegetables, fruits, and fish is beneficial. It’s also advised to maintain a body mass index of 20 to 25 kg/m2 and a waist circumference of less than 94 cm for men and less than 80 cm for women.
What else can Myocardial Infarction (Heart Attack) be?
- Angina pectoris (chest pain or discomfort due to coronary heart disease)
- Non-ST segment elevation myocardial infarction (NSTEMI, a type of heart attack)
- ST-segment elevation myocardial infarction (STEMI, another type of heart attack)
- Pulmonary embolism (a blockage in the lungs)
- Pneumothorax (collapsed lung)
What to expect with Myocardial Infarction (Heart Attack)
Despite numerous treatment advancements, acute heart attacks (MI) still have a mortality rate ranging from 5% to 30%, with most deaths happening before reaching the hospital. Furthermore, within the first year following a heart attack, an additional 5% to 12% mortality rate can be expected.
The overall outlook depends on the extent of damage to the heart muscle and its pumping efficiency (ejection fraction). Patients whose left side of the heart (ventricular function) remains largely unaffected generally have better outcomes.
However, the prognosis worsens with certain factors such as diabetes, advanced age, delayed treatment to restore blood flow (reperfusion), low pumping efficiency (ejection fraction), the presence of congestive heart failure, elevated levels of C-reactive protein and B-type natriuretic peptide (BNP), and depression.
Possible Complications When Diagnosed with Myocardial Infarction (Heart Attack)
There are different types of heart complications that may manifest in various ways:
- Ischemic
- Reinfarction: a second heart attack
- Extension of infarction: the heart attack area increases
- Angina: chest pain due to reduced blood flow to the heart
- Arrhythmias
- Supraventricular or ventricular arrhythmia: irregular heart rhythms starting in the heart’s upper or lower chambers
- Sinus bradycardia and atrioventricular block: slow heart rate and a delay or complete block in the transmission of the heart’s electrical impulses
- Mechanical
- Myocardial dysfunction: the heart muscle doesn’t contract normally
- Cardiac failure: the heart can’t pump blood efficiently
- Cardiogenic shock: sudden severe loss of heart function leading to a life-threatening condition
- Cardiac rupture: breaking open of the heart wall or a heart valve, either due to a heart attack or a blow to the chest
- Embolic
- Left ventricular mural thrombus: blood clot forms in the left ventricle
- Peripheral embolus: blood clots travel and block blood vessels in other parts of the body
- Inflammatory
- Pericarditis: inflammation of the pericardium, the sac-like covering of the heart
- Pericardial effusion: fluid accumulation around the heart