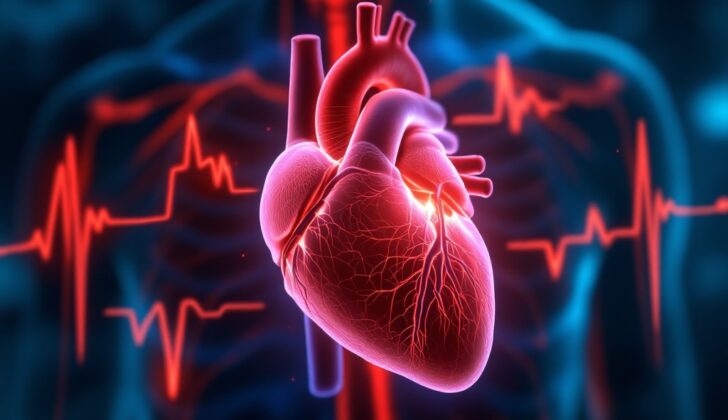
What is Premature Atrial Contractions?
Premature atrial contractions (PACs) are beats that start in your heart’s upper chambers, the atria, but not from the place it normally starts – the SA node. PACs are sometimes also known as atrial premature complexes (APCs) or premature supraventricular beats. Several factors can cause this to happen, including different types of medical conditions, changes in the structure of the heart, certain medications, and unauthorized substances.
What Causes Premature Atrial Contractions?
Premature atrial contractions or PACs occur due to a variety of reasons, and in some cases, the exact cause is unknown. In situations where no heart disease is present, these unknown or ‘idiopathic’ PACs often start from the pulmonary veins, which are the vessels that carry blood from your lungs back to your heart.
PACs can be categorized into three types based on their causes: structural, chemical, or resulting from other health conditions.
‘Structural’ causes refer to problems with the physical structure of the heart. These may include heart diseases such as coronary artery disease (blockages in the heart arteries), hypertrophic cardiomyopathy (a disease where the heart muscle becomes abnormally thick), aneurysms in the left atrial appendage (a small pouch in the heart), left ventricular hypertrophy (thickening of the heart’s main pumping chamber), diseases of the heart valves, defects in the wall that separates the two sides of the heart, and birth defects of the heart. Genetic mutations affecting the heart’s sodium channels, and BMP2 (a gene linked to lung blood pressure issues), can also trigger PACs.
‘Chemical’ causes refer to drugs or substances that can stimulate PACs. These include medications like beta-agonists (drugs that relax muscles of the airways), digoxin (a drug used for heart conditions), chemotherapy drugs, tricyclic antidepressants (a type of medication used for depression), sympathomimetic amines (drugs that mimic the actions of the nervous system), and monoamine oxidase inhibitors (another class of antidepressants). Surprisingly, beta-blockers, which are often used to control heart disease, can also sometimes increase the occurrence of PACs.
Certain health conditions and lifestyle factors can also increase the likelihood of experiencing PACs. These include heart attacks, congestive heart failure (a condition where the heart can’t pump enough blood to meet the body’s needs), high blood pressure, diabetes, chronic obstructive pulmonary disease (a type of lung disease), infection with Coxsackie virus (which can cause various symptoms), high CHA2DS2-VASC score (a method doctors use to estimate stroke risk in people with irregular heart beat), anxiety, pregnancy, tiredness, alcohol, or tobacco use. Interestingly, contrary to popular opinion, caffeine hasn’t been linked to an increase in PACs.
Risk Factors and Frequency for Premature Atrial Contractions
PACs, or premature atrial contractions, are heart rhythm abnormalities that can happen to anyone, regardless of age or other health risks. They’ve even been found in newborn babies without any associated risk factors, although this is still considered unusual. It’s worth mentioning that these abnormalities are more common in elderly patients. It’s more common to identify these abnormal rhythms through consistent monitoring, for example using a Holter monitor, rather than a standard electrocardiogram. This might be partly due to daily changes in our bodily functions, known as circadian rhythms.
As medical technology continues to improve, and becomes more widespread and affordable, we might start detecting arrhythmias more frequently. This is because these devices can pick up on abnormal rhythms that might otherwise go unnoticed.
Signs and Symptoms of Premature Atrial Contractions
Premature atrial contractions (PACs) often don’t show clear signs or symptoms. Many individuals with PACs don’t experience any discomfort and end up finding out they have this condition when tested for other medical issues. However, some symptoms may occur, including a feeling of skipped heartbeats or palpitations. Other symptoms can include shortness of breath, feeling anxious, or even signs of heart failure if PACs are consistent.
Medical examination findings do not always clearly indicate the presence of PACs, as symptoms can be inconsistent and unsteady. When symptoms do present, a doctor might feel abnormal pulses, observe unusual patterns in neck veins, or hear extra or early heartbeats during a listening test of your heart.
- Feeling of skipped heartbeats or palpitations
- Shortness of breath
- Feeling anxious
- Signs of heart failure if PACs are consistent
- Abnormal pulses
- Unusual patterns in neck veins
- Extra or early heartbeats
Testing for Premature Atrial Contractions
An electrocardiogram is a test that doctors use to detect abnormal heart rhythms by measuring the electrical activity in your heart. Premature atrial contractions (PACs) are heartbeats that happen earlier than normal and are a common type of heart rhythm disorder. They usually have a normal heart wave pattern (or QRS complex) and the time between the start of one heartbeat to the next (the PR interval) may be normal, shorter, or longer than usual. In some cases, a PAC may not lead to the next part of the heartbeat (the QRS complex).
PACs can come from one or several places in the heart. The heartbeat created by the PAC usually occurs earlier and looks different than a normal heartbeat. Its appearance can range in height, length, and shape and it may appear upside down or have two phases.
Depending on where the PACs start, the time between the start of one heartbeat and the next could be shorter (if it originates from a lower part of the right upper chamber of the heart, near the part that sends the signal to the lower chambers) or longer than usual. Looking at the results from multiple leads (the stickers placed on your chest during an EKG) may be necessary to spot subtle differences. If the heart wave appears upside-down in the leads that are checking the lower part of your heart, this suggests the PAC is coming from a lower part of the heart. If the heart wave appears upside-down in leads that are checking the left side of your heart, this suggests a left-side start. PACs can also appear within the wave that represents the relaxation phase of the heartbeat in cases of fast heart rates. If your EKG doesn’t show any PACs, a 24-hour heart monitor (Holter monitor) might be needed to catch them.
Doctors might also use a technique that visualizes the pressure in your neck vein (jugular vein) to evaluate PACs. This test is not always accurate, but it can help doctors draw conclusions. This test is easy and inexpensive because it only involves a simple physical exam. If the test is positive, you might see a large vein pulse – this is when the upper chamber of your heart contracts and pushes blood against a closed lower chamber, causing a backflow of high-pressure blood into your vein. This could happen if the upper chambers contract too early when the lower chambers haven’t opened yet (during the contraction phase), which is a sign of PACs.
Mapping the electrical activity in the heart (using a procedure called electrophysiologic mapping) is not usually needed to identify PACs.
Once PACs are identified, an ultrasound of the heart (echocardiography) can show how well your heart is functioning and if there are any structural issues with your heart. It’s important to check for structural heart disease in people with frequent PACs because this can affect how serious the condition is and determine what treatment is needed. Lab tests can also be done to check if you have any mineral imbalances in your blood.
Treatment Options for Premature Atrial Contractions
When it comes to treating PACs (premature atrial contractions – early or extra heartbeats), the treatment largely depends on the symptoms, triggers, and whether or not there are any related heart conditions. Typically, only patients who experience symptoms from PACs need treatment. The first step in the treatment process is often reassuring the patient that PACs are usually harmless and can often be managed by avoiding the things that trigger them. If symptoms persist despite avoiding triggers, then medication might be necessary.
One commonly used type of medicine for PACs is beta-blockers, which are considered relatively safe and are usually the first choice for patients whose symptoms aren’t relieved by avoiding triggers. The use of calcium channel blockers for PACs isn’t as well-established. There are also certain types of antiarrhythmic drugs that can suppress the origin of PACs, but these aren’t commonly used due to their potential to cause other irregular heart rhythms.
If symptoms persist despite medication, or if there are things like heart failure or cardiomyopathy that are connected to the frequent PACs and/or if the PACs trigger other heart rhythm disturbances like atrial fibrillation, more invasive treatments may be considered. Some of these treatments include atrial pacing and catheter ablation (a procedure to scar tiny areas in your heart). Among these, catheter ablation is commonly used. To perform this, doctors use a special map of the heart’s electrical system to find where PACs are coming from. If PACs are coming from the lungs’ blood vessels, those areas are usually ablated (or scarred) to prevent abnormal electrical signals from entering the left atrium (or upper chamber) of your heart.
It’s always best to first try to manage PACs with non-drug methods. Frontline healthcare providers can provide initial reassurance and medical treatments. However, if symptoms continue despite treatment, or if antiarrhythmic medications are needed, a cardiologist should be consulted. Procedures like catheter ablation are performed by skilled heart specialists.
What else can Premature Atrial Contractions be?
Diagnosing premature atrial contractions (PACs) can be quite difficult because the symptoms, physical exam results, and medical imaging findings are often not unique to this condition. Both heart-related and non-heart related issues may cause similar symptoms.
Heart-related causes can be broken down into two categories: those related to heart rhythm, and those not. Rhythm-related causes include:
- Premature junctional contractions
- Premature ventricular contractions
- Narrow or wide complex tachycardias (rapid heart rates)
An EKG, or electrocardiogram, which is a test that checks for problems with the electrical activity of your heart, can be important in identifying these causes. Heart causes not related to rhythm, on the other hand, may include:
- Acute coronary syndrome (a term for conditions caused by sudden reduced blood flow to the heart)
- Heart valve disorders, especially mitral valve prolapse
- Pericarditis (inflammation of the sac that surrounds your heart)
- Heart failure
- Complications from a pacemaker
In addition to these heart-related causes, non-heart-related causes could also mimic the symptoms of PACs. Remember, the following issues may also cause similar symptoms:
- A panic attack or severe anxiety
- Alcohol consumption and use of illegal drugs
- Side effects from prescribed medicines
- Pulmonary embolism (a condition where one or more arteries in your lungs become blocked by a blood clot)
- Hyperthyroidism (an overactive thyroid)
- Anemia (a condition where your blood has fewer red blood cells or less hemoglobin than normal)
What to expect with Premature Atrial Contractions
The outlook for patients with PACs, or premature atrial contractions (heartbeats that occur sooner than normal), largely depends on the root cause of these early heartbeats and if the heart has other structural problems. Generally, PACs without a known cause are not typically a severe short-term issue. However, if they occur frequently, they can carry a higher risk of related heart issues and even overall mortality.
Similarly, frequent PACs can increase the chance of developing atrial fibrillation (an irregular, often rapid heart rate that commonly causes poor blood flow) or atrial flutter (a condition where the heart’s upper chambers beat too quickly). Generally speaking, the existing medical conditions a person has play a substantial role in determining the outlook for their health.
Possible Complications When Diagnosed with Premature Atrial Contractions
When discussing the risk of complications from PACs, it’s important to also consider any existing underlying medical conditions. The complications that may arise from PACs, even if you don’t have any other health issues, include:
- Atrial fibrillation – a heart rate that’s irregular and often rapid.
- Ischemic stroke – a type of stroke caused by a blockage in an artery that supplies blood to the brain.
- Increased risk of death from heart-related issues and overall.
However, if you only have PACs, without premature ventricular complexes (another kind of irregular heartbeat), your risk of sudden cardiac death is not increased.
Preventing Premature Atrial Contractions
It’s crucial to keep up to date with the latest medical knowledge based on solid evidence. This is particularly important for doctors and patients regarding isolated PACs, or premature atrial contractions, which are early, extra heartbeats. These are generally harmless unless they are linked with underlying health conditions. Patients should be informed about potential triggers for these heartbeats so that they understand how to avoid them.
It should also be noted that people can sometimes feel worried or upset because of these premature heartbeats. It’s important for medical professionals to address these emotional aspects appropriately and reassure patients that the condition is typically benign, meaning not harmful in and of itself.