What is Premature Ventricular Contraction?
The heart has an electrical system which helps it pump blood efficiently throughout your body in a regular rhythm. The heart’s beat usually begins with special cells in the heart’s right upper chamber (atrium), known as the sinoatrial (or SA) node. These cells send an electric signal that travels down to another group of special cells, the atrioventricular (or AV) node. This electric signal then goes down a pathway called the bundle of His and Purkinje fibers to the heart’s lower chambers (ventricles). As a result, the lower heart chambers contract and pump blood out to the body’s arteries.
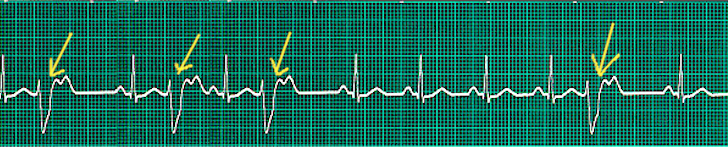
A premature ventricular contraction (PVC) is a type of irregular heartbeat. During a PVC, the heartbeat is started by the Purkinje fibers instead of the usual SA node. This creates a sort of interruption. Because the PVC comes before a regular heartbeat, there’s a noticeable pause before the next regular heartbeat.
PVCs can happen alone or in repeating patterns. If you get two PVCs in a row, it’s called a doublet; three in a row are called triplets. More than three PVCs one after the other is known as ventricular tachycardia, which is a fast rhythm of the heart. If the PVCs alternate with a regular heartbeat, it’s called bigeminy. Similarly, if every third heartbeat is a PVC, it is named trigeminy.
Most people feel PVCs like heart palpitations. They’re usually harmless and don’t typically require treatment.
What Causes Premature Ventricular Contraction?
In most cases, PVCs, or premature ventricular contractions, which are extra, abnormal heartbeats, happen spontaneously without a clear cause.
However, there are some known factors that can contribute to PVCs. These include drinking too much caffeine, having lots of stress, and abnormal levels of minerals in your blood. Specifically, having low levels of potassium and magnesium in your blood, and high levels of calcium can cause PVCs. Other lifestyle factors, such as consuming alcohol, smoking tobacco, using illicit drugs, taking medications that stimulate the body, or not getting enough sleep, can cause PVCs as well.
There are also various heart-related and non-heart related conditions that might cause PVCs. For example, conditions like cardiomyopathy (a disease of the heart muscle), mitral valve prolapse (a condition where the heart’s valve doesn’t close properly), and myocardial infarction (a heart attack) can cause PVCs. This happens because any changes in the heart’s structure that affect how electric signals get conducted can lead to PVCs. As for non-heart related conditions, hyperthyroidism (overactive thyroid), anemia (not having enough healthy red blood cells), and hypertension (high blood pressure) can cause PVCs too.
People who have a higher risk of heart disease and poor heart health are more likely to experience PVCs.
Certain groups of people are generally more at risk for PVCs. These include older adults, men, people with high blood pressure, African Americans, and those with low magnesium, a blocked bundle branch (a type of heart block), low potassium, or an underlying heart disease.
Risk Factors and Frequency for Premature Ventricular Contraction
PVCs, or premature ventricular contractions, are quite common in the general population. Electrocardiogram exams estimate their prevalence from 1% to 4% while for a 24 or 48-hour Holter monitor, it could be as high as 40% to 75%. Interestingly, even young and healthy adults show a similar rate of PVCs as seen in older segments of the population.
Signs and Symptoms of Premature Ventricular Contraction
PVCs, or premature ventricular contractions, are often experienced as a feeling of a skipped heartbeat, followed by a fluttering sensation or heart palpitations. Although not everyone experiences symptoms, some individuals may feel lightheaded, have chest discomfort or pain, experience difficulty breathing (dyspnea), or feel anxious due to PVCs. Rare cases may lead to fainting, or what’s medically referred to as syncope.
- Skipped heartbeat feeling
- Fluttering sensation or heart palpitations
- Lightheadedness
- Chest discomfort or pain
- Breathing difficulty (dyspnea)
- Anxiety
- Fainting (syncope) in rare cases
When assessing a patient with PVCs, it is crucial to understand their medical history, any supplements or medications they’re using, and get a comprehensive social background, including any illegal drug usage. A physical examination might show an irregular heart rhythm if PVCs are occurring at the time. More persistent PVCs could lead to low blood pressure (hypotension). If the patient complains of feeling dizzy, a doctor should look for other potential causes, which might involve an orthostatic examination (checking blood pressure and heart rate changes from a lying to standing position).
Testing for Premature Ventricular Contraction
The initial test usually used to diagnose a heart condition is a 12-lead electrocardiogram. This is a test that tracks the electrical activity in your heart. Doctors utilize this test to search for irregular heartbeats, known as ectopic ventricular beats. However, as these irregular beats are typically infrequent, the electrocardiogram may not always pick them up. This test also allows doctors to differentiate between different types of irregular beats, such as those that originate from the lower chambers (ventricles) of the heart known as premature ventricular contractions (PVCs), and those starting in the upper chambers (atria) of the heart, which are called premature atrial contractions (PACs).
In patients with PVCs, the ECG can reveal other issues including imbalances in the minerals in the blood (potassium, magnesium, calcium), enlargement of one of the lower chambers of the heart (left ventricular hypertrophy), signs of a previous heart attack such as changes in the normal pattern of heartbeat, and signs of a blocked or narrowed artery which can lead to chest pain or a heart attack.
To diagnose the issues causing “palpitations” or an unusual awareness of your own heartbeat, doctors may use a Holter monitor. This is a portable device that you wear for 24 or 48 hours which continuously records your heart’s rhythms. This device helps doctors distinguish PVCs from other heart rhythm problems. It’s also vital to count the number of PVCs over a set time to assess the patient’s risk for heart disease that affects the heart muscle (cardiomyopathy). Event monitors can also be used for this purpose. These are similar to Holter monitors but can be worn for up to 30 days.
Blood tests are also necessary. These help doctors identify the potential causes of the PVCs. Comprehensive blood tests, including checks for levels of potassium, calcium, magnesium, and thyroid-stimulating hormones should be ordered.
Further diagnostic tests, such as echocardiography (an ultrasound of the heart) and stress testing can also be used. The echocardiogram is used to rule out structural heart disease, but only if there is a medical reason to suspect it. Stress testing is another key part of a thorough heart evaluation. This test measures your heart rate while you exercise and can be useful for those who experience PVCs during or after physical activity.
The severity of PVCs is categorized using a grading system known as the Lown Grading system. This ranges from Grade 0 which indicates no evidence of premature beats, up to Grade 5 which indicates a highly irregular pattern that might increase the risk of dangerous heart rhythms.
Treatment Options for Premature Ventricular Contraction
Patients who have asymptomatic Premature Ventricular Contractions (PVCs) usually do not require treatment, especially if PVCs occur infrequently. When admitted to the emergency room, patients who have low oxygen levels in their blood will be given oxygen, and any imbalance in their body’s electrolytes, which are minerals that help regulate bodily processes, will be fixed. They will be also evaluated for drug toxicity. The medical staff will make sure to rule out a heart attack.
In terms of medication, the routine use of lidocaine (a type of local anesthetic) and other drugs used to treat heart rhythm problems is not recommended if the patient is having a heart attack.
Patients who experience frequent PVCs or symptoms related to PVCs require further evaluation to identify the cause. In many cases, consuming too many stimulants such as caffeine or having low levels of potassium and magnesium in the body can cause PVCs. Moderating intake of these stimulants and boosting levels of necessary minerals can help manage these cases. This strategy can also be beneficial for those who don’t have symptoms and only have occasional PVCs but find them bothersome. Besides, such patients could also find reducing stress beneficial.
When it comes to medicine, various classes of drugs can be used to treat patients who suffer from frequent or problematic PVCs. These drug classes include antiarrhythmics (drugs that work to correct heart rhythms), beta-blockers (drugs that relax blood vessels and slow heart rate), and calcium channel blockers (drugs that help reduce high blood pressure). Drugs known as amiodarone and flecainide are commonly used to treat irregular heart rhythms.
There are cases where patients experience very frequent PVCs or PVCs that don’t respond to medication. Such patients may be suitable for a procedure known as radiofrequency catheter ablation. In this, a specialized heart doctor called an electrophysiologist destroys a very small portion of heart tissue causing irregular beats, ensuring a normal heartbeat is resumed. Research has shown that successful treatment can reverse heart damage caused by PVCs.
What else can Premature Ventricular Contraction be?
There are several heart rhythm conditions, some of which can feel very similar to the heart skipping a beat, include:
- PAC (Premature Atrial Contraction) – These often feel like a skip in your heartbeat but are generally harmless. They also don’t cause as long a pause between heartbeats as some other conditions.
- Non-sustained ventricular tachycardia (NSVT) – This is when there are three or more skipped beats in a row. It’s referred to as NSVT until it lasts for 30 seconds or more.
- Sustained ventricular tachycardia
- Bigeminy – This is a repetitive, regular rhythm of the heart where every other beat is a premature contraction.
- Trigeminy – This is a repetitive, regular rhythm of the heart where every third beat is a premature contraction.
- Quadrigeminy – This is a repetitive, regular rhythm of the heart where every fourth beat is a premature contraction.
- Supraventricular tachycardia – This is a faster-than-normal heart rate that begins above the heart’s lower chambers.
- Sinus arrhythmia – This is a normal variation of the heart rate that increases with inspiration (breathing in) and decreases with expiration (breathing out).
- Atrial fibrillation – This is a rapid, irregular beat of the upper chambers of the heart.
What to expect with Premature Ventricular Contraction
Premature ventricular contractions (PVCs), or extra, abnormal heartbeats, generally don’t pose a problem for otherwise healthy people without heart disease and their health outlook is similar to the general population’s. However, those who experience a large number of these abnormal heartbeats (over 1000 a day) might be at risk of developing a condition called dilated cardiomyopathy, where the heart’s ability to pump blood is decreased.
For people who already have heart disease, PVCs could signal a higher risk of dying.
The impact of PVCs on the health outlook varies during exercise. If the PVCs happen during the action of exercising, there’s usually no issue. But if they occur during the period when you’re recovering from exercise, there can be a higher risk of dying in the long-term when compared to the general population’s risk.
PVCs occurring in people with left ventricular dysfunction, a condition in which the left side of the heart doesn’t pump blood properly, are often associated with a high risk of dying. But PVCs that can’t be provoked during an electrophysiology (EP) study, a test that records the electrical activity and the electrical pathways of the heart, usually present a lower risk of sudden death.
However, it’s important to note that there are some limitations when studying PVCs’ health impacts. Some patients might have undetected heart diseases, or long-term risk factors, which can affect their health prognosis.