What is Pulmonary Atresia With Intact Ventricular Septum?
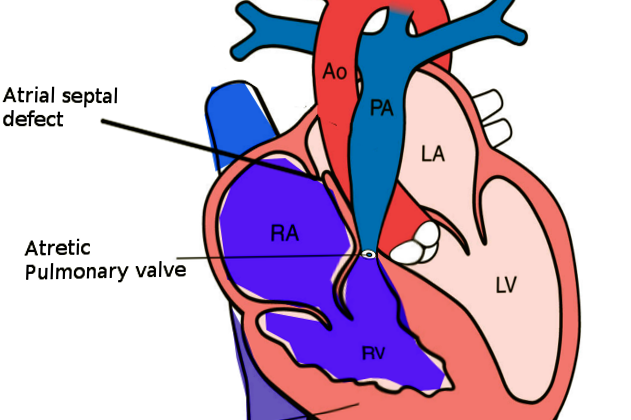
Pulmonary atresia with an intact ventricular septum (PA-IVS) is a rare type of heart disease that babies can be born with, making up less than 1% of all heart defects. It occurs when the passage from the right chamber of the heart to the lungs is blocked or closed off, and there’s no hole between the ventricles, the lower two chambers of the heart. This can often lead to underdevelopment of the right side of the heart and of the tricuspid valve, which controls blood flow from the right chamber to the lung. This defect was first noticed in 1783 and has been studied ever since. There’s a lot of variability in how PA-IVS affects individuals, depending on things like the size of the right ventricle and tricuspid valve and whether the coronary circulations, the blood vessels supplying the heart, are dependent on the right ventricle.
While genetic research suggests a tendency for some heart conditions to be inherited, the exact cause of PA-IVS isn’t known. Some theories suggest it might be caused by problems during the formation of the pulmonary valve in the fetus, obstruction of blood flow through the tricuspid valve, or abnormalities of the coronary arteries. Newborns with PA-IVS often have a bluish coloration to their skin and low oxygen levels, especially after the closure of a vessel called the ductus arteriosus, which is vital for their blood circulation to the lungs. A physical check-up might reveal only one type of heart sound instead of the usual two, a continuous heart murmur if the tricuspid valve is leaking, and possibly a murmur from a persistently open ductus arteriosus.
Diagnosing this condition is mostly done through an ultrasound of the heart (echocardiography), which can detect PA-IVS in about 86% of cases before birth. The ultrasound checks the wall between the upper chambers of the heart, the tricuspid valve, right ventricle, and the arteries going to the lungs. However, to get detailed information about the circulation of blood vessels of the heart, a procedure involving threading a catheter through the vessels to the heart and injecting dye for an X-ray (cardiac catheterization with angiography) is needed. Managing PA-IVS starts with a medication that keeps the ductus arteriosus open, which is necessary for survival before surgery. Surgical intervention is needed in newborns, and the treatment depends on the individual, and it might include repairing the two heart chambers, creating a bypass from the body’s artery to the lungs, repairing one heart chamber, or a heart transplant, specifically considering the features of the right ventricle, tricuspid valve, and the coronary arteries’ layout.
What Causes Pulmonary Atresia With Intact Ventricular Septum?
Congenital heart diseases are usually categorized by their physical characteristics, but they can also be sorted by how likely they are to be inherited. Various studies suggest that the heart conditions called heterotaxy and right ventricular outflow tract obstruction (a blockage that hampers the flow of blood out of the lower right part of the heart) are the ones most likely to be passed down genetically.
For example, people with right ventricular outflow tract obstruction have nearly a 50% chance of passing it to their direct relatives. In comparison, the chances of passing on left ventricular outflow tract obstructive defects (blockages that hamper the flow of blood out of the lower left part of the heart) and conotruncal defects (abnormalities in the heart’s structure) are lower, near 13% and 12% respectively.
The exact defect that leads to a condition called pulmonary atresia with intact ventricular septum (PA-IVS) is still not fully understood. Some theories suggest several possibilities such as damage to the pulmonary valve resulting in a blocked valve, an unusual vein valve limiting the blood flow through the tricuspid valve into the lower right part of the heart, or abnormal development of the coronary arteries.
Risk Factors and Frequency for Pulmonary Atresia With Intact Ventricular Septum
PA-IVS, a rare and diverse heart condition, occurs in about 4 to 5 in every 100,000 live births. Despite the gradual improvement of survival rates over time, the outlook is still challenging. At 1 year, the survival rates are 70% to 75% and at 5 years, it’s between 63% and 67%, varying with the postnatal circulation type. As per a study in the UK and Eire in 1998, the incidence rate was around 4 per 100,000 live births. Another US study in 1984 recorded the incidence at roughly 8 per 100,000 live births.
Nowadays, more PA-IVS cases are being diagnosed during pregnancies worldwide, due to the increased access and use of fetal echocardiography. Fetal heart intervention is a complicated procedure performed scarcely and requires extensive experience and further research to grasp its prognosis and outcomes. Currently, the top three fetal heart interventional procedures are catheter-based aortic stenosis in fetuses with evolving hypoplastic left heart syndrome (HLHS), HLHS with an intact or restrictive atrial septum, and PA-IVS.
PA-IVS impacts all sexes equally and has not been linked to any genetic disorders. However, cases of PA-IVS in identical twins and siblings have been reported. The significance of the genetic evaluations in these cases is still unclear.
- Concerning when PA-IVS happens during gestation, it is suggested it occurs later compared to pulmonary atresia with ventricular septal defect (PA-VSD).
- The pulmonary valve atresia is categorized into two forms: membranous and muscular. It is critical to identify these forms because membranous pulmonary atresia has a better long-term prognosis compared to muscular pulmonary atresia. This is because muscular pulmonary atresia has a higher incidence of irregular connections between the right ventricle and coronary arteries.
- With PA-IVS, the right ventricle frequently forms abnormal connections with the coronary arteries. These connections can lead to the narrowing of the coronary arteries over time which can sometimes cause a dependency of some parts of the heart muscle on the right ventricle for blood supply. This condition is known as RVDCC and its progressive nature can predict a poorer prognosis.
Signs and Symptoms of Pulmonary Atresia With Intact Ventricular Septum
Pulmonary atresia with intact ventricular septum (PA-IVS) is a heart condition that might cause symptoms like blue-tinted skin (cyanosis) and low oxygen levels in the body (desaturation). Symptoms usually present in newborns once the ductus arteriosus, a blood vessel that’s a part of fetal circulation, closes after birth. They don’t usually show signs of poor blood flow (low cardiac output) because the blood bypasses the lungs (through a hole called the foramen ovale in the heart) from the right to left chambers of the heart. However, if there is low cardiac output, it could signal an issue with blood supply to the heart muscle, especially for patients with abnormal connections between their heart and blood vessels (coronary fistulae). In cases of PA-IVS, increased oxygen levels do not improve symptoms, and tests that increase oxygen supply may not yield positive results.
On examining the heart sounds, doctors may notice single first and second heart sounds. If a heart valve (the tricuspid valve) is not closing properly and is leaking blood backwards (regurgitating), a continuous heart murmur might be heard on the left lower side of the chest. Another murmur might also be heard if a patent ductus arteriosus is present, especially after the start of a specific medicine (prostaglandin) to keep the ductus arteriosus open. Regular pulse rate and normal time for color to return after pressing the skin (capillary refill time) are generally observed in these patients, except for ones with severe backward flow of blood at the top chambers of the heart (atria).
Testing for Pulmonary Atresia With Intact Ventricular Septum
Two-dimensional echocardiography, a type of heart scan, is a readily available test frequently used to diagnose a condition known as PA-IVS. This heart disorder is most often diagnosed before birth, thanks to the widespread use of heart screenings during pregnancy. Recent studies showed that about 86% of cases were diagnosed before the baby was born.
While echocardiography can diagnose PA-IVS, it can’t give us all the information we need. For example, it does not tell us about the heart’s circulation, which impacts treatment options and outcomes. For this reason, another test called cardiac catheterization with angiograms is often needed to get a complete diagnosis.
When performing an echocardiogram, doctors will specifically look at:
1. The interatrial septum: This is a part of the heart that allows blood to flow from the right side to the left. This flow is vital in patients with PA-IVS.
2. The tricuspid valve: This is a gate in the heart that controls blood flow. Its size, shape, and performance are crucial as these aspects can significantly influence the type of surgery needed.
3. The right ventricle: This is the chamber of the heart that pumps blood to the lungs. Doctors will assess its size and shape in detail.
The heart scan alone is not enough for a complete diagnosis. That’s where cardiac catheterization comes in. This test can provide additional information about the heart’s circulation, which is particularly important in patients for whom relief of pressure from the right ventricle is a consideration. This procedure is used to diagnose RVDCC, a condition where the heart muscle relies on the right ventricle for the blood supply. Notably, the diagnosis of RVDCC is made when two or more major arteries are narrowed or blocked.
Various techniques can be used for optimal imaging of the heart. These include right ventricle angiogram, aortogram, aortogram with balloon occlusion of the aorta, and selective coronary angiograms. If there’s evidence of damage to the heart muscle on an electrocardiogram, it may suggest RVDCC.
Treatment Options for Pulmonary Atresia With Intact Ventricular Septum
Right after a baby is diagnosed with PA-IVS, a condition where the pulmonary valve in the baby’s heart does not form properly, doctors aim to start using a type of medication called prostaglandins. This drug is important because it keeps an important blood vessel called the ductus arteriosus open. This blood vessel is a crucial source of blood flow to the lungs for babies with PA-IVS. Additionally, managing the resistance in the baby’s blood vessels is important to achieve the best possible blood flow.
Babies with PA-IVS need treatment quickly. This treatment can be done using a slim, flexible tube called a catheter, or can be a surgical procedure. The complexity and variety in the ways this condition can present itself mean that not all patients can be treated with just one method. Ideally, a form of surgery called biventricular repair is most preferred. However, the treatment plan needs to be carefully tailored to each patient. Various factors can influence what type of surgery or catheter-based procedure is best. These factors include the size and function of the tricuspid valve (one of the heart’s valves), the structure of the right side of the heart and the coronary arteries, and the specific nature of the patient’s pulmonary atresia (absence or blockage of the pulmonary valve).
For example, if a baby has severe underdevelopment of the right side of their heart, a two-step surgical procedure known as single ventricular repair may be considered.
Babies with a normal size and functionally healthy right side of the heart, and a tricuspid valve larger than the average (a z-score over 2.5), and normal coronary arteries can benefit from biventricular repair. Another procedure that uses radiofrequency to create a hole in the pulmonary valve can also be an option. If the baby has a longer section of atresia, a surgery to reconstruct the right ventricular outflow tract can help.
For babies with margins of certain values in the size of their right side of the heart and tricuspid valve, a biventricular repair may be attempted, possibly with an additional procedure known as a systemic-to-pulmonary shunt. These babies need regular check-ups to monitor the growth of the right side of the heart; if it doesn’t grow properly, one-and-a-half ventricular repairs could be beneficial. In serious situations, such as those related to problems with the blood supply to heart muscle, a heart transplant may be considered.
It’s important for doctors to remember that patients who are presented with the above treatment options 2, 3, and 4, need an additional procedure, either a shunt (a small tube) to connect the systemic circulation to the pulmonary artery or a stent (a tiny wire mesh tube) to keep the PDA (patent ductus arteriosus) open in the immediate newborn period.
What else can Pulmonary Atresia With Intact Ventricular Septum be?
When trying to diagnose PA-IVS, doctors also need to consider other conditions that might cause a drop in oxygen levels and lead to a blue or purple coloration of the skin (known as cyanosis). These conditions include:
- Tetralogy of Fallot (a combination of four related heart defects)
- Transposition of the great arteries with pulmonary stenosis (a heart condition where the two main arteries leaving the heart are reversed)
- A single ventricle with severe pulmonary stenosis (a heart condition with a narrow or blocked exit from the right ventricle)
- Tricuspid atresia (a heart defect present at birth where a valve between two of the heart’s chambers isn’t formed)
What to expect with Pulmonary Atresia With Intact Ventricular Septum
Multiple studies suggest that survival rates for patients with this heart disorder have gradually improved. This is primarily due to advancements in children’s heart health (pediatric cardiology) and heart surgery (cardiothoracic surgery). According to a study from the United Kingdom and Ireland in 2005, about 71% of patients lived for one year after diagnosis, and approximately 64% lived for five years.
This study identified that low birth weight and having a single-part right ventricle – a part of the heart – can increase the risk of death. Additionally, certain types of this disorder, particularly when the openings of the heart’s arteries (coronary ostia) are obstructed (atresia), can lead to poor outcomes.
A recent study collected data from newborn babies treated for this condition between 2009 and 2019 across 19 centers in the United States. This study aimed to describe patient outcomes, identify factors linked to different results, and assess the effect of the right ventricle’s dependency on the coronary (heart’s arteries) and the obstruction of these arteries on survival without the need for a transplant.
In this study, 295 patients were reviewed. They found that 15.2% of patients had a two-part heart repair, 5.4% had a one-and-a-half-part heart repair, 25.4% had a specific procedure called the Fontan procedure, 9.8% had a heart transplant, and 18.3% of patients unfortunately passed away. Twenty-five percent of patients remained with mixed blood circulation.
The study estimated the cumulative risk of death to be 10.9% at one month, 16.1% at six months, 16.9% at one year, and 18.8% at five years after diagnosis.
Possible Complications When Diagnosed with Pulmonary Atresia With Intact Ventricular Septum
Pulmonary Atresia with Intact Ventricular Septum (PA-IVS) is a severe heart condition that is not compatible with life unless specific late-stage development conditions are met in the womb. Echocardiography, which is a way of making images of the heart, is often used as the main way to identify and understand this condition before surgical intervention in newborns with complex heart diseases. However, it can be difficult to predict the possible risks and outcomes using only this method. Multiple factors measured in echocardiography have been suggested as ways to determine the possible success of a type of heart repair procedure known as biventricular repair, but it’s not yet clear which of these should be recommended for routine use.
Quite predictably, the diameter ratios of certain heart valves (the tricuspid valve and the mitral valve) and certain heart chambers (the right and left ventricles) can be used to predict successful two-chamber repair or the necessity for an intervention that increases blood flow to the lungs. Previous studies have shown that more severe leakage of the tricuspid valve (tricuspid regurgitation) is usually a good indicator for the two-chamber repair. However, measuring this leakage in newborns has a large amount of subjective interpretation and can be affected by other conditions, including the state of the pulmonary blood vessels and the type of breathing support being used.
Preventing Pulmonary Atresia With Intact Ventricular Septum
PA-IVS, or Pulmonary Atresia with Intact Ventricular Septum, is a rare and tricky type of heart defect that can show up in very different ways. It’s believed to be caused by problems during an important stage of a baby’s development in the womb. This condition can look a lot like other serious heart defects – like tetralogy of Fallot, another condition that makes it hard for the blood to get to the lungs properly.
A heart ultrasound, otherwise known as an echocardiogram, is very important for spotting this condition. A more detailed test called cardiac catheterization can give even more information, especially about the state of the vessels that supply the heart with blood.
Managing and treating this heart problem can be pretty complex. There are quite a few different treatment steps to follow, and doctors use special guides called therapeutic algorithms to help them decide on the best approach.