What is Radiation-Induced Coronary Artery Disease?
Radiation-induced coronary artery disease (RICAD) is a health problem known to affect people who have been treated with chest radiation therapy for cancer, here specifically referring to being exposed to radiation. It’s also known to occur from other types of radiation exposure. The more chest radiation therapy is used as part of cancer treatment, the more people are likely to get RICAD. This condition is believed to be caused by a faster development of atherosclerosis, a disease of the heart’s blood vessels.
RICAD often affects younger patients. It’s closely linked to the type of chest radiation therapy used and the amount of radiation received by the patient. In most cases, it affects the primary blood vessels of the heart’s outer layer, even leading to disease in the main artery on the left side of the heart. This article will help you understand more about the causes of RICAD, how common it is, what symptoms it causes, how it’s diagnosed, screening suggestions, treatment methods, how to differentiate it from other diseases, and the complications it can lead to.
What Causes Radiation-Induced Coronary Artery Disease?
Exposure to radiation can either occur naturally or be caused by medical procedures. Most natural radiation exposure doesn’t result in high levels all at once. Natural radiation could come from things like radon gas from the ground, sun rays, and high altitudes.
However, a lot of people encounter radiation through things like medical imaging or therapies. This is why people, who’ve had radiation therapy (RT), commonly develop a condition called radiation-induced coronary artery disease (RICAD). This condition is often seen in people who have had radiation therapy for certain types of cancer, such as breast, Hodgkin’s lymphoma, lung, esophageal, and thymoma.
The amount and chance of getting RICAD heavily depends on where the radiation was applied and how much was given over time. Patients who receive chest radiation continue to be at risk for RICAD and related heart attacks for up to 25 years after their first radiation therapy. For example, one study showed an increase in heart-related death among patients receiving a certain level of radiation (over 30 Gy) to the chest area. Another study showed that, in breast cancer patients, the risk of significant heart events increased by 7.4% for every Gy increase in the average radiation dose to the heart.
There are also other factors that can increase the likelihood of developing RICAD. These include age (younger patients are at a higher risk), taking heart-toxic drugs such as anthracyclines, and known heart disease risk factors like smoking, diabetes, high levels of fat in the blood, high blood pressure, and obesity.
Risk Factors and Frequency for Radiation-Induced Coronary Artery Disease
Radiation-induced coronary artery disease (RICAD) is often associated with conditions like breast cancer and Hodgkin lymphoma. However, less commonly, it is also associated with lung cancer, esophageal cancer, and thymoma. It has been found that survivors of Hodgkin lymphoma who underwent radiation therapy are 2.5 times more likely to develop coronary artery disease. This is higher than breast cancer patients, who only have a 0.25 times higher risk. This higher risk in Hodgkin lymphoma patients comes from a larger radiation dose compared to breast cancer patients.
The added risk of a heart attack in Hodgkin lymphoma patients who received chest radiation is 125.8 per 100,000 person-years. For breast cancer patients who underwent chest radiation therapy, the additional risk of cardiac death is 125.5 per 100,000 years. Even if the incidence of coronary artery disease in breast cancer patients after radiation therapy is lower, the risk continues to increase with time.
Younger patients who receive radiation therapy are at greater risk for developing RICAD. Evidence from a study on patients treated with radiation for Hodgkin lymphoma found that those under 25 years of age at the time of exposure had the highest risk. Although initially, the incidence of RICAD was higher following left-sided radiation therapy, recent reports have noted higher rates following right-sided radiation therapy, specifically involving the right coronary artery.
Signs and Symptoms of Radiation-Induced Coronary Artery Disease
Radiation-induced coronary artery disease (RICAD) can occur in individuals who’ve been exposed to chest radiation therapy. It usually affects younger patients who’ve been exposed to this type of therapy and it can happen with or without typical risk factors for coronary artery disease.
- RICAD can exhibit symptoms from subtle chest discomfort to silent heart conditions.
- RICAD can present with sudden cardiac death, caused by blockage of the main artery or other important blood vessels.
- Usually, there is a significant delay (on average, about seven years) between the initial radiation exposure and the onset of RICAD symptoms.
- It often affects individuals who are under 50 years old but cases have also been reported in kids and teenagers.
Physical symptoms are similar to those of general coronary artery disease. Upon a physical examination, doctors might observe:
- Unusual resting heart rate and abnormal heart rate post-exercise.
- Dyspnea (breathlessness)
- Ankle swelling
- Pulmonary crackles, which are sounds heard in the base of the lungs due to fluid buildup.
- Jugular vein enlargement due to development of heart muscle disease caused by lack of blood supply.
- Patients with RICAD can also have heart murmurs due to an increased likelihood of valve disease.
- RICAD is linked to a higher incidence of heart valve disease.
Testing for Radiation-Induced Coronary Artery Disease
For people who’ve had chest radiation therapy (RT), monitoring for Radiation-Induced Coronary Artery Disease (RICAD) is crucial. Medical experts recommend that evaluations for coronary artery disease (CAD, a condition where your heart’s blood vessels can become clogged) should start around ten years after the chest RT, with ongoing checks done every five years – regardless of whether the patient has symptoms or not. At present, there’s no definitive guideline on whether symptom-free patients showing signs of obstructive RICAD should be treated with medications or through procedures aimed at improving blood flow (revascularization).
Two substances used as ‘biomarkers,’ brain natriuretic peptides and troponin, have been found to increase in patients with RICAD. Additionally, C-reactive protein, a substance that increases when there’s inflammation in the body, consistently increases in the patients suspected of having RICAD. A non-contrast chest CT scan can show, through a form of measurement called the Agatston score, evidence of calcium buildup in the coronary arteries – a sign of potential heart disease – in patients with RICAD. In patients who’ve had RT because of Hodgkin’s lymphoma (HL), a coronary calcium score of 0 is usually an excellent predictor of the absence of heart disease.
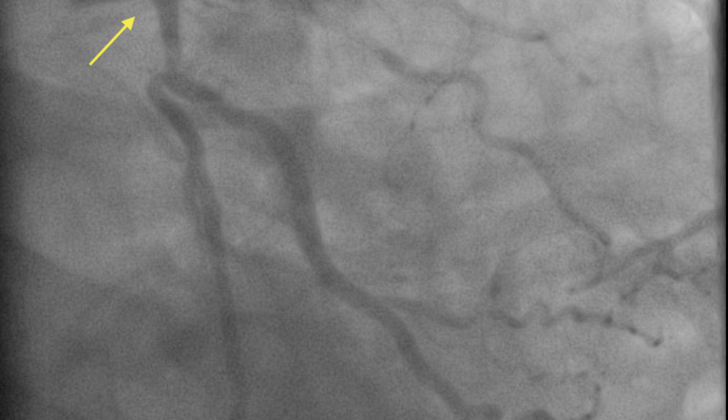
Stress testing lets doctors see how the heart performs under stress and has been used to evaluate CAD in patients. These tests often hint at restricted blood flow (ischemia). Still, it seems that these tests don’t often match up with findings from tests to evaluate coronary microvascular disease, where the tiny blood vessels in the heart are impacted. Using Coronary CT Angiography, which gives us detailed images of the heart and blood vessels, it was found that a number of heart-related abnormalities increased over ten years in patients who had had chest RT due to HL.
In patients who had chest RT for breast cancer (BC), the left main coronary artery, a central blood vessel supplying the heart, is usually most impacted due to the left-sided radiation. Patients with HL after chest RT have the possibility of all major vessels being affected. The reason behind this could be the position of these vessels that leads to higher radiation exposure.
Ideally, evaluation of patients showing symptoms of acute coronary syndrome (a range of conditions caused by a sudden, reduced blood flow to the heart) should follow the same steps as for suspected CAD in the general population. High-risk patients should go through a procedure called invasive coronary angiography, which allows doctors to see blood flow in the coronary arteries. Meanwhile, medium-risk patients should either have anatomical mapping or stress testing to evaluate their coronary arteries.
Treatment Options for Radiation-Induced Coronary Artery Disease
In layman’s terms, if you’ve been diagnosed with RICAD (Radiation-Induced Coronary Artery Disease), which is a heart condition caused by radiation therapy, medicines like aspirin and statins could help prevent severe heart events. Other medicines like captopril, simvastatin, and colchicine have been shown in animal studies to reduce the harmful effects of radiation injury, and might help prevent RICAD. However, these drugs have not been fully tested in human trials for this specific use, and there are no official guidelines yet for using these meds to prevent RICAD.
One common treatment for RICAD is called percutaneous coronary intervention, which is a procedure that opens up blocked blood vessels that supply the heart, in order to improve blood flow. This has been a widely used method, similar to treating patients with CAD (Coronary Artery Disease – a build-up of plaque in the arteries) in the general population. Past studies that looked at patients who received stents (tiny tubes inserted in an artery to keep it open) for certain types of RICAD showed the need for repeat treatment, likely due to the rapid progression of artery blocking. But the advent of drug-eluting stents, which release a drug to block cell overgrowth, has significantly reduced the need for repeat procedures.
CABG (Coronary Artery Bypass Graft Surgery), another treatment option, often faces numerous issues. Radiation therapy not only causes fibrosis (scarring) of the heart arteries, but it can also affect other structures in the front part of the chest, including the chest wall, the pericardium (the sac around the heart), and lung tissue, which, due to scarring can lead to postoperative respiratory complications. Further, people with a history of chest radiation have higher needs for additional surgeries and complex procedures during bypass surgery, such as valve replacements, because they have higher rates of valve dysfunction. Moreover, the scarring and prior damage to the chest wall often lead to poor wound healing after bypass surgery.
Finally, there is evidence that, for these patients, what’s called internal mammary grafts do not stay open as long as in the general population due to prior radiation damage. This makes choosing the pathway for bypass grafting very challenging.
What else can Radiation-Induced Coronary Artery Disease be?
When a doctor is determining if a patient has radiation-induced coronary artery disease (RICAD), they have to consider other health conditions that can appear similar. These conditions can either closely resemble stable or unstable coronary artery disease (CAD) and acute coronary syndrome, or are diseases that are linked to getting thoracic radiation. These conditions include:
- Pericarditis (an inflammation of the sac surrounding the heart, can either be acute or chronic constrictive)
- Pulmonary embolism (a blood clot in the lung)
- Coronary microvascular dysfunction (a poor functioning of the tiny heart arteries)
- Restrictive cardiomyopathy (a heart muscle disorder that affects the heart’s ventricles)
- Pulmonary fibrosis (a lung disease that occurs when lung tissue becomes damaged and scarred)
- Costochondritis (an inflammation of the cartilage in the rib cage)
- Kawasaki disease (an illness that causes inflammation in artery walls)
- Myocarditis (an inflammation of the heart muscle)
- Esophagitis (an inflammation that damages the tube that carries food from your mouth to your stomach)
What to expect with Radiation-Induced Coronary Artery Disease
Patients with RICAD (radiation-induced coronary artery disease) who are younger than the usual patients with CAD (coronary artery disease) tend to have more health complications and a higher risk of death. Besides, there are certain risk factors that can worsen the prognosis for these patients.
For instance, if a patient already has CAD, the risk of facing adverse heart-related events goes up by 60% after undergoing radiation therapy. Not staying physically active, or having a sedentary lifestyle, has also been correlated with an increased risk of heart-related events in patients who have previously had radiation therapy for HL (Hodgkin Lymphoma) or BC (Breast Cancer).
Possible Complications When Diagnosed with Radiation-Induced Coronary Artery Disease
The difficulties that can arise from RICAD are alike to those in the general population suffering from CAD. These include:
- Acute coronary syndrome, a term for situations where blood supplied to the heart muscle is suddenly blocked.
- Ischemic cardiomyopathy, when heart muscle is weakened due to inadequate blood flow.
- Acute heart failure, which means that the heart is not able to pump adequate blood required by the body.
- Arrhythmias, or irregular heartbeats.
- Valvular dysfunction, where the heart’s valves don’t open or close correctly.
- Sudden cardiac death.
Preventing Radiation-Induced Coronary Artery Disease
The process of educating patients begins with a discussion before initiating Radiation Therapy (RT). Radiation therapy is a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors. Patients should be made aware of their risk for developing Radiation-Induced Coronary Artery Disease (RICAD), a possible negative outcome of the treatment. This awareness should be based on the anticipated amount of radiation they’ll receive, the prospect of receiving chemotherapy alongside RT, and other risk factors they may have. Chemotherapy is a type of cancer treatment that uses drugs to destroy cancer cells.
Alternative treatment options should also be presented to the patients. If, however, radiation therapy is deemed the best course of action, patients should be referred to specialized healthcare centers that focus on targeted radiation therapy, like photon therapy. Photon therapy is a type of radiation treatment that kills cancer cells with high-energy particles, or photons.
Those undergoing RT should have discussions with their healthcare providers about routine imaging tests to monitor their heart health and measures they can take to lessen their overall risk of Coronary Artery Disease (CAD). CAD is a type of heart disease that occurs when the major blood vessels that supply the heart with blood, oxygen, and nutrients, become damaged or diseased.