What is Spontaneous Coronary Artery Dissection (Burst Heart Artery)?
Spontaneous coronary artery dissection (SCAD) is a tear in one of the heart’s main surface arteries. SCAD can feature different degrees of damage, ranging from a minor tear in the innermost layer of the artery to a large blood clot forming within the artery’s layers. It’s important to note that SCAD is different from other heart issues as it doesn’t result from usual triggers like injury, artery intervention, or a ruptured plaque deposited in the artery due to heart disease. This condition is often the main reason younger women, including those who have recently given birth, experience acute coronary syndrome (ACS), a range of conditions related to sudden, reduced blood flow to the heart, even if they have no other risk factors.
People with SCAD can experience a range of symptoms and issues. These can include everything from tissue damage or death due to disrupted blood flow to the heart, to less severe cardiovascular issues, life-threatening heart rhythm irregularities, heart failure, and even sudden cardiac death. Most cases of acute coronary syndrome (ACS) usually happen when a plaque deposited in an artery due to heart disease bursts and forms a clot, blocking blood flow. However, ACS can also occur due to SCAD, which causes blood to pool within the artery’s walls, squeezing the main passageway and interrupting blood flow downstream.
In terms of anatomy, the heart’s blood supply comes from three main surface arteries. The left coronary artery splits into the left anterior descending artery (which supplies the front wall, part of the septum, and the heart’s tip) and the left circumflex arteries (that supply the left ventricular front and back sides). Occasionally, a third branch forms between the two main left-sided branches, known as the ramus intermedius.
On the right side of the heart, the right coronary artery is the primary source for blood flow in about 80% of people. It originates from the right portion of a structure called the Valsalva’s sinus, fueling the right atrium, the heart’s natural pacemaker (sinoatrial node), the right ventricle, most of the septum, and the bottom and back left ventricular parts.
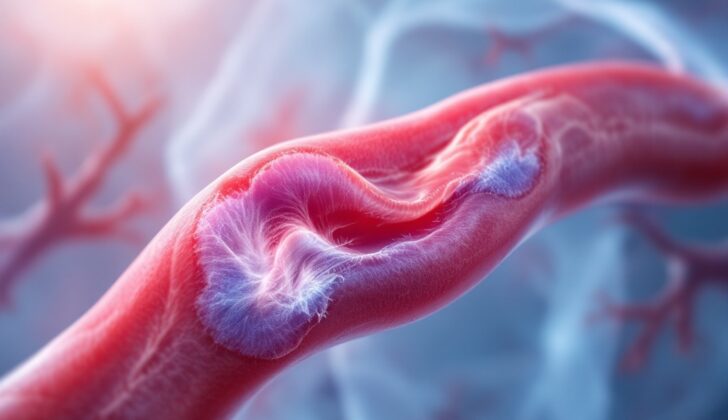
Each artery is composed of three layered sections: the tunica intima (made of endothelial cells, muscle cells, and connective tissue, and the primary site for atherosclerosis – the build-up of plaque), the tunica media (comprised of smooth muscle cells), and the tunica adventitia (formed of collagen and elastic fibers and including smaller blood vessels that oxygenate the larger vessels, lymph vessels, and nerve fibers). The first two layers are separated by elastic sheets.
SCAD happens when blood accumulates in the tunica media, forming a blood clot within the arterial wall layers. This clot dislodges the innermost layer from the outer layer, creating a secondary arterial passage that constricts the original one and impedes blood flow, leading to acute coronary syndrome.
The artery that is most often affected by SCAD is the left anterior descending artery. The frequency of involvement for the different arteries is about 50% for the left anterior descending artery and its branches, around 30% for the circumflex, ramus, and obtuse marginals, 25% for the right coronary artery and its branches, about 15% for multivessel, and approximately 4% for the left coronary artery. The arteries farther from the heart are more likely to develop SCAD.
There are three ways in which SCAD can be detected on an angiogram, a type of X-ray used to visualize blood vessels:
- Type 1: Characterized by multiple layers within the artery or dye staining in the artery walls.
- Type 2: Identified by a narrowing of the artery with a sudden change in diameter.
- Type 3: Seen as a small, localized narrowing (usually less than 20 mm) which can appear similar to atherosclerosis. In this case, the presence of a blood clot within the wall layers should be confirmed by further imaging techniques.
What Causes Spontaneous Coronary Artery Dissection (Burst Heart Artery)?
Spontaneous coronary artery dissection (SCAD) is a condition that is not fully understood, but it’s believed to have multiple causes. SCAD tends to mostly affect young women, including those who are pregnant. This has led to the idea that female hormones, stress, and certain blood vessel conditions like fibromuscular dysplasia (FMD) might be related to its occurrence. FMD is a disease that affects your blood vessels, but it doesn’t involve plaque buildup or inflammation. It’s most common in younger women and can cause problems like aneurysms, narrow blood vessels, and dissected vessels and can impact blood flow to the heart. Research has shown that about 10.5% of those with FMD experience a dissection, and 2.5% develop SCAD.
Some cases have shown similar features between SCAD and FMD, leading to suggestions that SCAD could be how FMD shows up in the blood vessels that supply the heart. However, we need more large-scale research to confirm this link.
SCAD is the most common cause of a type of heart attack in young women who don’t have the typical risk factors for heart disease. It’s especially common among young women who are pregnant, just gave birth, or are taking birth control pills, which suggests female hormones may play a role. In fact, hormones like estrogen and progesterone may alter the structure of the blood vessels, making them more likely to tear or dissect.
The outcome for women experiencing SCAD during pregnancy is often poor. They tend to have larger heart attacks, are more likely to have disease in the main or multiple blood vessels, decreased heart pumping effectiveness, shock due to heart failure, heart attack caused by a completely blocked artery, and heart rhythm issues.
Some studies also suggest there is an association between intense physical or emotional stress and SCAD. In fact, one study found that 40% of SCAD patients had experienced intense physical stress beforehand and 24% had experienced emotional stress. It’s thought that the flood of stress hormones, which can cause a condition known as stress-induced cardiomyopathy, might also contribute to SCAD by putting strain on the blood vessels supplying the heart.
Risk Factors and Frequency for Spontaneous Coronary Artery Dissection (Burst Heart Artery)
Spontaneous coronary artery dissection, or SCAD, can occur in both men and women, although it is much more common in women in their 50s and 60s, with around 90% of cases occurring in this group. The risk factors related to heart disease are generally lower in these patients compared to those with acute coronary syndrome (ACS) due to plaque rupture. SCAD is a rare cause of ACS and accounts for less than 1% of all heart attacks. Since it’s rare in men, there isn’t a lot of data available for them.
- SCAD more commonly affects women in their 50s and 60s.
- The condition is a rare cause of ACS, accounting for less than 1% of all heart attacks.
- Data on the condition in men is limited owing to its rarity in this group.
Several risk factors for SCAD have been identified, including pregnancy, having recently given birth, other artery diseases, and physical and emotional stress. The majority of patients are white women. The likelihood of death from SCAD is low, around 1-2%, and the risk of a repeat ACS incident is about 18%.
- Risk factors for SCAD include pregnancy, recent childbirth, other artery diseases, and stress.
- The majority of people affected are white women.
- The risk of death from SCAD is low, at about 1-2%.
- The chances of having another ACS event is about 18%.
Signs and Symptoms of Spontaneous Coronary Artery Dissection (Burst Heart Artery)
If someone has a spontaneous coronary artery dissection, the main sign they’ll feel is chest pain similar to angina. This affects more than 90% of people with the condition. Those who experience this while they’re pregnant or have just given birth can also encounter severe complications. These might include arrhythmia, or unusual heart rhythms, heart failure leading to shock, or even sudden cardiac death.
You might notice several other signs if heart failure or heart-related shock is present due to the heart not pumping properly. For example, the patient might seem slow or confused, and their skin might take longer to return to its normal color after being pressed. When listening to the heart, a doctor might hear an abnormally fast heartbeat, a specific type of abnormal rhythm called an ‘S3 gallop’, or a slower than normal heartbeat and complete heart block if the right coronary artery is involved.
If a heart attack has affected the front wall of the heart and led to heart failure, a murmur may be present in the heart sounds. This may be due to an acute mitral regurgitation, which can occur when severe heart damage leads to a rupture in one of the muscles that help control one of the heart valves. This tends to affect the muscle that is supplied by the RCA (right coronary artery) only. A particular type of muscle damage called an acute septal wall rupture can also lead to a ventricular septal defect, which will create a murmur.
You can suspect a serious problem called pericardial tamponade if you observe distant heart sounds, raised pressure in the veins in the neck, low blood pressure, and a condition called pulsus paradoxus. This condition might occur if the heart wall ruptures. Regular cardiovascular system examinations are crucial for diagnosing post-heart attack complications as early as possible while the patient is still in the hospital.
During a detailed vascular physical examination, a doctor might see signs that could point to FMD and potential other abnormalities in the blood vessels that are connected to spontaneous coronary artery dissection. For example, a pulse that feels strong and full might suggest the presence of an aneurysm, a bulging blood vessel. And a pulse that feels weak and uneven, along with a whooshing sound when the doctor listens to the artery, could indicate that the artery has narrowed or suffered dissection. Specific sounds over the stomach area and by the kidneys could suggest renal FMD, a specific type of this disease affecting the kidneys. Similarly, a whooshing sound in the neck area could point out that it’s the carotid artery in the neck that’s affected.
Testing for Spontaneous Coronary Artery Dissection (Burst Heart Artery)
If you’re having chest pain and changes in your heart’s electrical activity (seen on an EKG), along with changes in the levels of a heart protein called troponin, this could suggest you have a condition called Acute Coronary Syndrome (ACS). An EKG, or electrocardiogram, is a test that checks for problems with the electrical activity of your heart. It might show changes like an increase in the “ST” segment (a part of the EKG related to the heart’s rhythm), or changes in the T-wave or the ST segment. These changes can indicate damage to the heart muscle. You might also have an echocardiogram, which is an ultrasound of your heart. It could show issues with the heart muscle’s movement in the area supplied by the tiny blood vessels of the heart, called coronary arteries. As soon as doctors diagnose ACS, you would likely go to a room in the hospital called the cardiac catheterization lab for further tests and treatment.
A coronary angiogram is the go-to first test when a patient has ACS. This imaging test looks at the blood flow in your coronary arteries to see if they’re blocked or narrowed. A specific pattern that can be seen on angiogram suggests a condition called a spontaneous coronary artery dissection, which is a sudden tear in the wall of an artery in your heart. This condition can present as ACS. The coronary arteries in this condition may look like beads due to multiple contrast “halos”.
Though commonly the arteries may appear narrowed along a segment (which can be seen in around 70% of patients). A left ventriculogram, a special type of x-ray that checks for issues with your heart’s main pumping chamber, can show whether the heart muscle moves normally. It’s also important to know that a coronary angiogram can cause accidental dissection (a tear inside the artery) in about 3% of patients with spontaneous coronary artery dissection.
Intracoronary Imaging offers a detailed look at the inside of the coronary arteries. Tools like intravascular ultrasound (IVUS) and optical coherence tomography (OCT) allow doctors to see dissection flaps, internal bruising of the blood vessel wall, tears in the inner lining of the artery, and the true and false artery channels. Although intracoronary imaging gives a clearer picture than an angiogram, it is only used if the angiogram is not giving the doctors enough information. But its use might be limited because of its availability, the risk of worsening a dissection, and the preference for less invasive diagnostic methods.
Coronary Computed Tomography Angiography (CCTA) is an imaging test that uses x-rays to provide detailed images of the heart and its blood vessels. However, CCTA isn’t typically used during the early stage of care for acute coronary syndrome. That’s because a non-calcified plaque (a fatty build-up in the arteries) can look similar to an internal bruise in the artery. Also, CCTA is not effective in visualizing smaller vessels often affected by spontaneous coronary artery dissection, which can lead to missing the disorder. However, CCTA can be helpful in the follow-up care for patients with spontaneous coronary artery dissection that involves the heart’s large or main arteries.
Treatment Options for Spontaneous Coronary Artery Dissection (Burst Heart Artery)
Conservative management, or non-surgical treatment, is often the first option for stable patients with a spontaneous coronary artery dissection. This approach works well in over 90% of the patients, as they show signs of healing usually within a month. However, nearly 18% may experience a recurrent heart attack due to the progression of the dissection, with about half of these patients facing a recurring event within the first week.
Patients undergoing conservative management should be hospitalized and monitored for 3 to 5 days, and they need to be followed closely even after discharge. Invasive coronary angiograms, which are x-rays of the blood vessels, are only recommended for high-risk patients, such as those with recurrent symptoms, abnormal stress tests, or complex conditions. For others, stable patients can be monitored with a coronary CT angiography, which is a type of imaging test that helps doctors see the arteries, which supply blood to the heart.
Percutaneous Coronary Intervention, or PCI, a non-surgical procedure used to treat narrowed or blocked coronary arteries, is shown to be associated with suboptimal outcomes and an increased risk of complications for spontaneous coronary artery dissection. It is reserved for those with ongoing ischemia, which means they have an inadequate blood flow to a part of the body, or hemodynamic instability, describing a situation where the circulatory system isn’t functioning properly.
Coronary Artery Bypass Grafting, or CABG, a surgical procedure that improves blood flow to the heart, is considered for patients with spontaneous coronary artery dissection after an unsuccessful PCI case, or continuous ischemia despite non-surgical treatment. However, long-term studies show a high rate of graft failure from blockage in the grafted arteries due to the flow through the healed original vessels.
The medical approach to Acute Coronary Syndrome (ACS), which is a term for different heart conditions, due to spontaneous coronary artery dissection varies from those cases caused by atherosclerosis, a disease where plaque builds up in the arteries.
Patients are initially given anticoagulation and dual antiplatelet therapies following the guidelines for ACS management. However, once a spontaneous coronary artery dissection is diagnosed through an angiography, anticoagulation use is usually stopped as it may worsen the condition. Thrombolytic therapy, which is used to break up blood clots, is not recommended as it can lead to the rupture of a coronary artery and cardiac tamponade, a serious medical condition in which the blood fills the sac around the heart.
Research does not recommend dual-antiplatelets for patients treated without surgery for spontaneous coronary artery dissection. Experts recommend long-term use of aspirin, but there’s no proven benefit of long-term antiplatelets in SCAD. Patients undergoing PCI should receive dual antiplatelets for at least a year according to current guidelines.
Beta-blockers have been shown to decrease the incidence of recurrent spontaneous coronary artery dissection and should always be prescribed. The usage of ACE inhibitors or angiotensin receptor blockers is reserved only for heart attack cases complicated with left ventricular systolic dysfunction, a condition in which the left ventricle of the heart doesn’t pump normally. There’s no role for statins, a type of medication used for lowering cholesterol, as the cause of ACS is not plaque eruption. Chest pain, a common symptom after SCAD, should be treated with various medications.
Prevention of recurrence, meaning a new dissection event, usually at a different location, is important. Beta-blockers can help prevent a recurrence after an initial event. Patients should be encouraged to avoid heavy exercise, high-intensity activity, and prolonged Valsalva maneuvers, which involve forceful exhalation against a closed airway and can increase pressure inside the chest.
What else can Spontaneous Coronary Artery Dissection (Burst Heart Artery) be?
When trying to diagnose spontaneous coronary artery dissection, a condition where the layers of the artery wall in the heart separate, doctors must also keep in mind other conditions that might cause a similar appearance on a heart scan or lead to the same issues. These include:
- Catheter-induced artery dissection: During a heart procedure, a tool called a guidewire might accidentally cause an internal injury, which can then evolve into creating a false tunnel that looks very similar to spontaneous coronary artery dissection. It’s recognized by the fact that there was a recent heart procedure.
- Atherosclerotic heart disease: This condition can resemble spontaneous coronary artery dissection on scans, because it also causes narrowing or blocking of the arteries. Specific imaging tests, such as an Intravascular Ultrasound (IVUS) or Optical Coherence Tomography (OCT), are needed to confirm the diagnosis.
- Coronary artery thrombosis: This condition involves a blood clot forming in the heart’s arteries. Certain factors, such as a ruptured plaque, smoking, tendency to form clots more easily, or a heart condition that can cause clots, may create a blockage that looks like spontaneous coronary artery dissection. The scan will show a fuzzy area with filling defects and a smooth curve at the obstructed place. Intravascular imaging tests help make the correct diagnosis.
- Coronary calcification: Sometimes hardening of the heart arteries or atherosclerosis, can appear as unique spots of calcification or hardening in a scan. Non-calcified plaques might also mimic a blood-filled swelling within the artery wall. This condition is diagnosed through imaging inside the coronary arteries.
These alternatives need to be carefully considered and the right tests need to be performed to secure the correct diagnosis.
What to expect with Spontaneous Coronary Artery Dissection (Burst Heart Artery)
Most people who follow the doctor’s advice and practice conservative management, or non-invasive treatment, usually get better within a month. However, if you’re pregnant and experience a heart attack due to a spontaneous coronary artery dissection (an unexpected tear in the coronary artery), complications may occur and outcomes might not be as positive.
With this medical condition, it’s not rare for the issue to reoccur; these patients need ongoing monitoring after leaving the hospital. To make sure things are improving, additional studies using CCTA (Coronary Computed Tomography Angiography, a heart-imaging test) may be performed.
In case the anatomy of your coronary arteries is particularly risky or if a functional study (a test that assesses how well your heart is working) shows abnormal results, a repeat invasive coronary angiogram may be required. This is a procedure that uses X-ray imaging to see your heart’s blood vessels.
Possible Complications When Diagnosed with Spontaneous Coronary Artery Dissection (Burst Heart Artery)
: The direct complications after a heart attack could include serious heart rhythm issues, a rupture in the heart wall, heart failure, and potentially, a shock caused by an inability of the heart to pump enough blood. Additionally, one in five patients may experience a recurrence.
Potential Complications:
- Ventricular tachyarrhythmias (heart rhythm issues)
- Ventricular free wall or septal rupture (heart wall tear)
- Congestive heart failure
- Cardiogenic shock (shock from insufficient blood flow)
Many patients also report chest pain after spontaneous coronary artery dissection, a rare condition where a tear forms in one of the blood vessels in the heart. This might be a consequence of the initial dissection or it could be related to non-heart related issues as these patients often experience high levels of stress, anxiety, or depression. Further complications include mental health conditions like post-traumatic stress disorder, depression, and anxiety, which could lower the overall quality of life. It’s important to screen these patients for such conditions before they are discharged.
Post-Dissection Issues:
- Chest pain
- High levels of stress
- Anxiety
- Depression
- Mental health conditions (for example, post-traumatic stress disorder)
- Decreased quality of life
Recovery from Spontaneous Coronary Artery Dissection (Burst Heart Artery)
If you’ve had a heart attack due to spontaneous coronary artery dissection (which is a rare condition where a tear forms in the blood vessels of your heart), it’s recommended that you participate in cardiac rehabilitation programs. These programs have been scientifically shown to aid in your physical recovery and improve your psychological wellbeing if you’ve survived a heart attack.
Preventing Spontaneous Coronary Artery Dissection (Burst Heart Artery)
Women who have had a spontaneous coronary artery dissection, an unexpected tear in the heart’s blood vessels, and are considering pregnancy, should talk to their healthcare provider before conception. This is because the condition can recur and may cause serious complications during pregnancy. After experiencing this heart condition, certain exercises should be avoided to help prevent it from happening again. This includes isometric exercises (where muscles contract without moving the rest of your body), high-endurance activities and exercises that involve holding your breath for an extended period.
There could be a connection between this heart condition and female hormones. Therefore, women should steer clear of external sources of hormones like progesterone and estrogen. These might be present in certain contraceptives or hormone replacement therapies. Avoiding these can help mitigate the risk of the heart condition from happening again.