What is Tetralogy of Fallot?
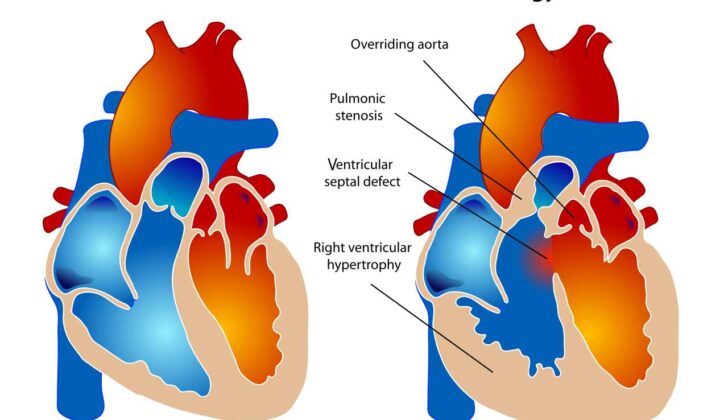
The Tetralogy of Fallot (TOF) is a heart defect that a person is born with. It is made up of four physical changes in the heart: a big hole in the lower part of the heart that’s not supposed to be there (a ventricular septal defect or VSD), an aorta (the main artery that carries blood away from the heart) positioned in a wrong place, a complication that causes difficulty in the blood’s exit from the heart’s right side (right ventricular outflow tract obstruction), and the heart’s right side becoming thick due to pressure (right ventricular hypertrophy). Additionally, parts of the heart’s structure, like the pulmonary valve, are often underdeveloped.
The symptoms a person with TOF experiences can depend on whether they have any other heart-related issues. Around 40% of people with TOF have additional heart problems. These can include holes in the heart wall, narrowness of arteries, abnormally formed organs, and the over-growth of blood vessels. Certain conditions can develop while the baby is still in the womb such as the narrowing of the heart’s exit.
TOF can also be associated with various anomalies. For example, in some patients, the main artery carrying blood to the lungs can be underdeveloped, but can take on unusual sizes and shapes. In some cases, the right and left arteries leading to the lungs join together and their blood flow depends largely on the ductus arteriosus, a blood vessel present in a fetus. For others, their lung’s blood supply comes from other sources, not relying on the ductus arteriosus. Operation of these cases can be challenging due to the complexity of unifying these blood supplies.
In some people with TOF – about 3% to 6% – there can be a scenario where the leaflets of the pulmonary valve are “rudimentary”, or undeveloped. This is referred to as “TOF with absent pulmonary valve”. In these cases, the main arteries to the lungs tend to be swollen, and a small heart valve can cause obstruction in blood flow. Usually, these patients have an absent ductus arteriosus and a right-sided aorta. Sometimes, a lung artery could originate from the aorta, or could be completely absent.
About 2% of those with TOF also have a heart wall defect called an atrioventricular septal defect (AVSD). These patients typically don’t show signs of heart failure as their condition limits overcirculation in the lungs. A surgery to correct this can safely be carried out within the first few months of their life.
What Causes Tetralogy of Fallot?
TOF, short for Tetralogy of Fallot, is a common heart defect that occurs when the outflow part of the heart doesn’t form properly. It’s grouped with other heart defects like truncus arteriosus, and double outlet right ventricle. If certain pathways called NOTCH and WNT don’t work properly during the early stages of an embryo’s development, it may cause the heart to develop inappropriately.
Around 75-80% of TOF cases are “nonsyndromic”, which means they occur on their own without any other health problems. In these cases, around 7% are due to changes, or “mutations”, in certain genes, including NOTCH1, FLT4, and TBX1.
It’s also worth noting that certain gene mutations have been linked to nonsyndromic TOF. These mutations are often seen in families with a history of heart defects. So, unsurprisingly, heart defects do sometimes run in families. This doesn’t necessarily mean the exact same defect will occur in all family members, but the overall risk of a heart defect is higher compared to the general population.
20-25% of TOF cases accompany other syndromes or chromosomal abnormalities. The most common accompanying conditions are Down’s syndrome and 22q11.2 deletion syndromes. The latter can range from severe DiGeorge syndrome, which comes with facial abnormalities, immune deficiencies, hypocalcemia, and learning disabilities, to the less severe Sprintzen or velocardiofacial syndrome.
Because patients with the 22q11.2 deletion often have accompanying aortic arch malformations, TOF can sometimes be related to aortic arch defects. When a patient with TOF also has pulmonary valve atresia, they are 40% more likely to have the 22q11.2 deletion. Therefore, genetic testing is often recommended for unborn babies diagnosed with TOF in order to check for the 22q11.2 microdeletion, as patients with this deletion often face worse outcomes.
TOF can also occur in patients with certain known genetic mutations, including those with Alagille syndrome, Kabuki syndrome, CHARGE syndrome, and Noonan syndrome. It can also be present in individuals with certain syndromes where the mutations are unknown, such as VACTERL association and Goldenhar syndrome.
Risk Factors and Frequency for Tetralogy of Fallot
Congenital heart disease (CHD) is present in about 1-1.2% of all live births. One specific type of CHD, known as Tetralogy of Fallot (TOF), is the most common type that causes blue discoloration due to lack of oxygen. TOF affects men and women equally, and it occurs in 1 out of every 3,000 births, accounting for 5-7% of all CHD cases. Nowadays, due to advancements in medical treatments and surgeries, we see more children and adults living with CHD. In the US, there are now about 1 million adults living with CHD, and 15% of these are TOF cases.
- Congenital heart disease (CHD) appears in about 1-1.2% of all babies born alive.
- Tetralogy of Fallot (TOF) is the most frequent type of CHD that leads to blue discoloration due to lack of oxygen.
- TOF affects men and women equally, and appears in 1 of every 3,000 births.
- TOF represents 5-7% of all CHD cases.
- The number of children and adults surviving with CHD has increased due to medical and surgical advancements.
- There are approximately 1 million adults living with CHD in the US, 15% of whom are TOF patients.
However, without surgical intervention, the survival rate for TOF patients reduces significantly as they get older. For example, if TOF is not corrected with surgery, the survival rate is estimated to be 66% at 1 year of age, dropping to 40% by 3 years of age, 11% by 20 years, 6% by 30 years, and down to 3% by the age of 40.
Signs and Symptoms of Tetralogy of Fallot
Tetralogy of Fallot (TOF) is a heart condition that causes varied symptoms based on the severity of the disease. Symptoms can range from a bluish color in a newborn (cyanosis) to trouble breathing and difficulty performing physical activities in adults. In some cases, the condition can be diagnosed before birth with the use of a fetal echocardiogram. This early detection can be life-saving, especially in severe cases where urgent treatment can prevent serious complications.
The symptoms of TOF can vary. Some cases are not severe and may not cause symptoms right away. These cases are often referred to as “pink Tets.” Patients may only have a loud heart murmur. Alternatively, if TOF is causing more obstruction, infants might show signs of overworked lungs after the first few weeks of life. Over time, even moderate cases of TOF can worsen and cause increased cyanosis, especially during crying or in episodes of decreased blood volume.
Some episodes, known as “Tet spells,” can occur in young TOF patients who haven’t yet received treatment. These episodes are marked by rapid, deep breathing and a decrease in the loudness of the heart murmur. These episodes can be dangerous and lead to fainting or even cardiac arrest. Once the patient turns about 4 to 5 years old, these spells tend to become less frequent and may even stop occurring altogether.
Patients with TOF and no functioning pulmonary valves can show severe respiratory distress, due to the large blood vessels in the lungs pressing down on the windpipe and main bronchi. Some patients’ conditions can be improved simply by positioning them facing down while others may need ventilatory support.
Physical exam findings in TOF patients often include a typical first heart sound with a typically inaudible second heart sound due to pulmonic component. The intensity of their heart murmur, usually described as crescendo-decrescendo with a harsh systolic ejection quality, could serve as an indicator of the degree of obstruction. A prominent ventricular impulse and a systolic thrill may be palpable, and a continuous murmur can be heard over the back and axillary regions in those with pulmonary atresia and aortopulmonary collaterals.
TOF patients who are adults may have complications arising from TOF repair, such as severe valve leakage leading to the enlargement of the right ventricle, severe tricuspid valve leakage, and arrhythmia. In rare cases involving those who did not undergo surgical repair, symptoms of chronic lack of oxygen could include high blood viscosity, abnormal blood clotting, stroke, brain abscess, and bacterial infection of the heart’s inner lining.
Testing for Tetralogy of Fallot
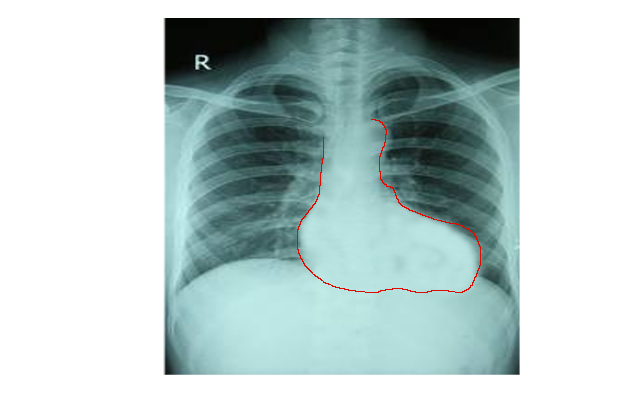
To diagnose Tetralogy of Fallot (TOF), a heart disorder, doctors most often use chest X-ray, electrocardiogram, and echocardiogram. These are imaging tests that take pictures of your heart.
A chest X-ray can show the shape and size of your heart. In cases of TOF, the heart usually looks normal in size. However, the top (apex) of the heart tends to turn upwards. The main artery that carries blood from the heart to the lungs (main pulmonary artery) can appear concaved or “boot-shaped”.
An electrocardiogram (ECG or EKG) records the electrical activity in your heart. In TOF cases, the EKG often shows unique patterns due to enlargement and strengthening of the right chambers of the heart. This could include going off in a specific direction (right axis deviation), having tall or large R waves or qR waves in lead V1 (the first lead of the EKG) and having upright T waves (part of the EKG waveform) in V1.
The echocardiogram is the best tool for diagnosing TOF. It uses sound waves to take moving pictures of your heart. These images can give your doctor useful information about the structures and workings of your heart. They can look at the severity and location of issues like obstructions in the right ventricular outflow tract (RVOTO), which lead blood out of the heart; ventricular septal defects (VSDs), which are holes in the wall separating the heart chambers; and any issues with the aorta or coronary arteries. However, this method sometimes struggles to look at the arteries farthest from the heart.
Adults who have had TOF treatment might also get a cardiac MRI or CT scan. These scans use magnetic and X-ray technology to create detailed images of your heart. Before these types of tests were available, doctors often used diagnostic cardiac catheterization for TOF diagnosis. This test is more invasive and involves threading a thin tube through your blood vessels to your heart. While it can still provide valuable details about the heart, it is not usually the first choice now. That said, it can still be useful in certain cases, such as assessing the severity of RVOTO, examining certain heart structures, and stenting ducts and RVOT. But doctors must tread carefully because this procedure can bring on serious episodes of low oxygen in the body.
Treatment Options for Tetralogy of Fallot
Newborns with serious right-ventricular outflow tract obstruction (RVOTO) that leads to low oxygen levels and a bluish color, need to be treated promptly before they undergo surgery or a procedure that improves heart function. Therapy could involve medications developed to keep a crucial blood vessel open and ensure sufficient blood flow to the lungs.
Sometimes, frightening episodes, known as ‘Tet spells’, can occur, which require swift and intensive care. Treatments may include positioning the child to increase blood flow, oxygen therapy to help open up the lung arteries, and giving intravenous fluids to enhance the heart’s blood flow. Medications might be required to slow the heart rate, improve blood flow, or increase blood pressure.
Pain relief medications can also be administered to manage the discomfort and anxiety experienced during a Tet spell. A Tet spell that isn’t managed properly might lead to loss of consciousness and can be life-threatening.
Without surgery, the survival rates for patients with a heart condition called tetralogy of Fallot (TOF) with no other heart defects are not promising. Many patients don’t survive past a few years if left untreated. Therefore, surgical procedures or interventions that help improve and stabilize blood flow to the lung are needed.
The timing of TOF repair is still debated among medical professionals. Many hospitals lean towards early repair, while others suggest delaying the full surgical repair till after the first three months of life.
There may be several reasons for opting for initial surgical palliation, such as technical difficulties related to the size of the infant’s arteries, risk of post-operation complications, unfavorable coronary artery anatomy, and the surgeon’s preference.
Less invasive alternatives to surgical palliation include specific procedures that do not require the heart and lungs to be bypassed. These procedures also avoid the need for serious surgical cuts, such as opening the chest.
More recent approaches tend to limit the incision size, which reduces the risk of complications. Also, care is often taken to ensure the heart’s electrical system is not damaged during the process.
In cases of TOF with a poorly developed or blocked right ventricular outflow tract (RVOT) or a large coronary artery crossing the RVOT, a conduit, or tube, is used to connect the right ventricle to the pulmonary artery. However, these conduits usually have a relatively short lifespan and might need replacing within a few years.
Children with certain TOF complications might require a special medication in their early life as their collaterals might not be sufficiently developed. These patients could undergo an early comprehensive repair or they could undergo a segmented repair, depending on their exact situation.
There are other possible surgical interventions, including reduction of the size of pulmonary arteries or a surgical connection between the right ventricle to the pulmonary artery, among others. Post-surgery, early extubation or removal of a tube placed into the windpipe can improve cardiac output. These treatments aim to provide the best possible results for those affected by TOF.
What else can Tetralogy of Fallot be?
“Tet spells” are a type of health issue that can cause difficulty breathing and an increase in blueness of the skin due to low oxygen. Other heart problems can result in similar symptoms. These may include:
- Complete transposition of the great arteries (d-TGA) with narrowing of the pulmonary artery
- Double outlet right ventricle with severe narrowing of the pulmonary artery
- Tricuspid atresia, a condition where the tricuspid valve in the heart hasn’t formed correctly
- Ebstein anomaly, a rare heart defect that’s present at birth
Isolated severe blockages of the pulmonary or aortic valves can also cause similar symptoms. Furthermore, respiratory tract infections such as bronchiolitis or pneumonia, as well as pneumothorax (collapsed lung), should also be considered when diagnosing these symptoms.
What to expect with Tetralogy of Fallot
While surgical procedures today are generally safe with roughly a 2% mortality rate and a 90% survival rate extending past 20 years, it is common for patients to experience long-term heart and blood flow abnormalities. This is especially true for patients who have moved past the third decade of their lives. For instance, those who undergo pulmonary regurgitation, a condition that happens when the heart’s pulmonary valve doesn’t meet properly and can lead to heart enlargement, dysfunction and a condition called diffuse interstitial fibrosis that sustains this dysfunction.
Heart dysfunction can also negatively impact the left ventricle due to abnormal interactions between the heart chambers.
It’s common to see symptoms like a high QRS interval (a measure of the electrical conduction time of the heart), sustained ventricular tachycardia (a fast, regular heart rate beginning in the lower chambers of the heart), or a history of fainting, result in exercise intolerance, heart failure, and death.
In recent research on grown-up patients who have undergone surgery for tetralogy of Fallot, a complex heart defect, it has been found that the highest risks of death relate to several factors. These include:
– Being younger than 50.
– The presence of abnormal signals in heart MRI scans, which often indicate extensive heart tissue scarring or fibrosis, and poor heart function.
– Oxygen uptake measuring 17 mL/kg/m2 or below.
– Abnormally high levels of B-type natriuretic peptide (a hormone that the heart produces when it is under stress).
– Sustained atrial arrhythmias (abnormal heart rhythms).
Further, different types of heart rhythm problems, usually intra-atrial reentrant tachycardia and cavotricuspid isthmus-dependent atrial flutter, can be seen as patients age after heart defect repair. They make up around 20% of the observed heart rhythm abnormalities in these patients.
Another factor affecting the prognosis of these patients is the possibility of needing a pulmonary valve replacement due to worsening pulmonary insufficiency, which puts them at risk of bacterial endocarditis, an infection of the inner lining of your heart.
A recent international, multi-center study established that patients with heart defect repair who undergo pulmonary valve replacement showed a lower risk of death and sustained ventricular tachycardia. Although, it didn’t provide concrete insights on ideal timing for the procedure or if a classical surgery or a less invasive transcatheter pulmonary valve placement procedure would provide better outcomes.
Possible Complications When Diagnosed with Tetralogy of Fallot
The process of performing surgery to install a Blalock-Taussig shunt, which is to relieve symptoms in certain heart conditions, can potentially harm nerves in the throat and diaphragm. Depending on the size of this shunt, this could lead to either an overflow of blood into the lungs causing heart failure, failure to grow or even turning blue from insufficient oxygen intake. The clotting of the shunt could pose a serious risk to one’s life, requiring an urgent additional operation, intervention with a catheter to eliminate the clot or in the worst-case scenario, external support for the heart and lungs (Extracorporeal Membrane Oxygenation or ECMO).
After heart defect repair surgery, common early complications may include:
- Build-up of fluid around the heart or in the chest cavity that might require drainage
- Chylothorax (liquid accumulation in the lungs)
- Bleeding necessitating another operation
- Minor wound infection
- Backflow of blood into the lungs in up to 14% of patients
- Leftover defects in the heart’s wall leading to inadequate oxygen
- Obstruction in the heart’s right ventricle.
In up to a fifth of patients, irregular heart rhythms can occur after surgery which can lead to low blood flow from the heart to the rest of the body, dangerously low blood pressure, and unstable blood flow through the heart and body. Corrective measures may include electrolyte balancing, cooling the patient, decreasing stimulating drugs, synchronizing the heart’s rhythms, increasing sedatives for pain control or antiarrhythmic drugs. If these treatments do not work, ECMO may be required until the heart rhythm normalizes. Young patients less than six months of age or patients receiving certain stimulating drugs after surgery are more likely to experience this complication.
Patients undergoing treatment via the transatrial-transpulmonary approach are seen to have fewer heart rhythm issues and virtually no need for a permanent pacemaker for postoperative heart rate abnormalities. Damage to the heart’s electrical system though can give rise to right bundle branch block, two-sided bundle branch block in 8-12% of patients, and complete heart block in 3-5% of patients. A stiff right ventricle can occur post-surgery due to a combination of causes and this can be managed by a careful balance of fluids and certain medication usage.
Heart rhythm abnormalities may occur after heart defect repair surgery, including increased heart rate in the ventricle, irregular heart rhythms or fast, irregular heartbeats. Decreased oxygen in the blood due to these conditions are associated with late death in patients.
As the condition advances, atrial flutter and fibrillation become increasingly common. Large right atrial size and considerable backflow of blood into the right atrium are implicated in the development of these abnormal heart rhythms.
Among all the long-term complications, failure of the pulmonary valve ranks higher. This is largely due to the persistence of blood flow back into the right ventricle and weakening of both right and left ventricles.
Patients with congenital heart disease are known to be at risk for intellectual disabilities due to associated syndromes, genetic or developmental disorders, and medical and surgical therapies. These patients may need additional educational resources, physical, occupational, and speech therapies that may even extend into adulthood.
Pregnancy complications in women who had correction of their heart defect are typically similar to the general population. However, complications may arise due to associated heart conditions that might affect the well-being of both the mother and the child. Unrepaired heart defects during pregnancy carry additional risks, including death.
Without surgical intervention, patients with Tetralogy of Fallot face mortality risks, largely from low oxygen spells, strokes, and brain abscesses. If left untreated, the lifespan of infants with severe restrictions in the right ventricle is significantly reduced.
Preventing Tetralogy of Fallot
Tetralogy of Fallot (TOF) is a type of congenital heart disease, meaning it’s a heart condition a person is born with. Thanks to advancements in surgical treatments, many adults are now living with TOF. As these individuals age, they may need further surgeries or non-surgical procedures, like a valve replacement done through a small tube inserted into a vessel (transcatheter pulmonary valve replacement.) They may also need treatments for irregular heartbeats (arrhythmia treatments), and lifestyle changes to prevent heart and blood vessel diseases related to abnormal levels of fats in the blood (dyslipidemia) and diabetes.
Most people living with TOF might have limitations when it comes to exercising, measured by things like how much oxygen their bodies can use and their heart rate. However, they can still participate in physical activities, but guidelines should be tailored to each person’s condition. It’s advised that people with TOF who have severely weakened heart muscle function, severe blockage to blood flow leaving the heart, or regular occurrences of irregular heartbeats, should avoid competitive sports. They may still be able to participate in low-intensity activities.
Pregnancy is usually handled well by women with TOF, provided they have good fundamental circulatory health. However, pregnancies in women with severe blockage in the blood flow from the heart to the lungs, severe backflow of blood through the heart’s pulmonary and tricuspid valves, as well as weak function of the right and left main pumping chambers, can lead to heart failure and irregular heartbeats. These women may also have a higher chance of needing a cesarean section, experiencing a miscarriage, giving birth prematurely (14%), and having smaller than average babies (10%). Therefore, these women are usually considered to have a low to moderate risk. Furthermore, they have a higher likelyhood of having a baby with a heart defect compared to the general population.