What is Tricuspid Regurgitation?
Tricuspid regurgitation is a somewhat common medical condition. In minor cases, it’s usually present but does not cause any significant problems. However, if it becomes severe, it can lead to dysfunction in the heart’s right ventricle, causing serious health issues, or even death. Any changes in the structure of the tricuspid valve, which is part of the heart, can lead to this condition.
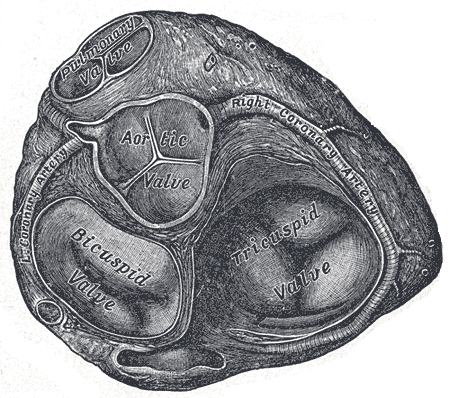
In terms of its anatomy, the tricuspid valve – also known as the right atrioventricular valve apparatus – is made up of four parts. First, there are the valve leaflets, which could range between 2 to 6 in number. The anterior leaflet is often the largest, while the septal leaflet is the smallest. Next, you have something called the fibrous tricuspid valve annulus. Then there are the supporting chordae tendineae. Last but not least, you have papillary muscles which can be anywhere from 2 to 9. Just before the beginning of a contraction in the right ventricle, these muscles contract, putting tension on the chordae tendineae. This helps the 3 valve ‘cusps’ (or flaps) to close properly and prevent backflow across the tricuspid valve.
The tricuspid valve works in coordination with the heart’s electrical conduction system and the supportive structure of the fibroelastic ‘cardiac skeleton’. This valve is located between the right atrium (the chamber where blood enters the heart) and the right ventricle (the chamber responsible for pumping blood), and its area is usually 4 to 6 square cm.
There are some pathologies (or variants) associated with the tricuspid valve. These include conditions like the Ebstein anomaly, tricuspid atresia, congenital tricuspid stenosis, and congenital cleft of the anterior leaflet.
What Causes Tricuspid Regurgitation?
Tricuspid regurgitation refers to a condition where one of the heart’s valves, the tricuspid valve, doesn’t close properly, causing blood to leak back into the heart’s upper right chamber. This condition can be divided into two main types: primary and secondary.
Primary tricuspid regurgitation is due to inherent issues with the tricuspid valve itself. However, this condition is relatively rare, particularly in adults.
Secondary tricuspid regurgitation, on the other hand, is more common. It happens when the right sides of the heart, the right atrium and the right ventricle, or the ring-like part surrounding the tricuspid valve (the tricuspid annulus) become enlarged. Although the tricuspid valve remains normal in structure, it can’t seal properly because of the larger space, which leads to the blood leakage. Potential causes for this can include heart diseases that enlarge or damage the right ventricle or result in high blood pressure within the lungs.
Such conditions include heart muscle diseases (cardiomyopathies), heart diseases that reduce blood flow to the heart muscle, and abnormal heartbeat (atrial fibrillation). Other causes can include conditions like hyperthyroidism or blockage in the artery supplying blood to the lungs.
For younger adults and adolescents, primary tricuspid regurgitation is often caused by heart defects present at birth, but they are quite rare for adults. Some causes for primary tricuspid regurgitation can include infections on the valve caused by substance misuse, cancers, alcoholism, a history of severe burns, or a weakened immune system. Injuries to the heart from things like implanted pacemaker wires, chest injuries, rheumatic heart disease, and medicines that cause damage to the valve can also lead to primary regurgitation.
Congenital conditions (conditions present at birth) can cause primary regurgitation too. For example, a condition known as Ebstein anomaly displaces certain parts of the tricuspid valve, resulting in malfunction. Disorders affecting the body’s connective tissues, like Marfan syndrome or Ehlers-Danlos syndrome, can also result in the tricuspid valve becoming floppy or mildly enlarged, leading to regurgitation.
Risk Factors and Frequency for Tricuspid Regurgitation
Tricuspid regurgitation, a heart condition, affects about 0.9% of people in the United States, regardless of gender or race. The condition typically shows up at different ages, based on the underlying cause. Some people are diagnosed with a related condition, known as Ebstein anomaly, at birth or during early childhood. For those who are 15 or older, the most common cause is a type of heart disease known as rheumatic valvular disease.
Signs and Symptoms of Tricuspid Regurgitation
Patients suffering from right-sided heart failure exhibit various symptoms. Some of them include painful enlargement of the liver or spleen, fluid buildup in the abdomen (known as ascites), and swelling in the limbs (known as peripheral edema). In severe cases, you might see visible pulsations in the neck due to dilated and pulsing jugular veins. A noticeable struggle with physical activities could also be present. It’s pretty common to observe signs of the condition causing the tricuspid regurgitation — for instance, lung high blood pressure might result in feelings of weakness, difficulty breathing, and trouble with physical activities. If the tricuspid regurgitation is a result of an infection in the lining of the heart (called infective endocarditis), patients may have episodes of fever.
The physical examinations for this condition might reveal the following:
- A noticeable distention in the neck veins with a prominent V wave indicating elevated right atrial pressure. This jugular vein distention is more evident when the patient breathes in (a phenomenon called Kussmaul sign).
- Third heart sound or S3 gallop signifying an extremely enlarged right ventricle.
- An audible continuous murmur throughout the heartbeat cycle that is high-pitched and heard loudest in the fourth rib space nearer to the sternum. This murmur’s intensity tends to increase during inspiration, exercise, and leg raising due to increased blood return, but reduces when standing or executing the Valsalva maneuver (breathing out forcefully with a closed mouth and nose).
- Presence of ascites, which is an accumulation of fluid in the abdomen.
- Signs of cachexia and jaundice, which indicate the body is wasting away and liver failure, respectively.
- Atrial fibrillation or irregular heartbeat.
- Peripheral edema or swelling in limbs.
- A heaving palpable right ventricle due to the right ventricle’s enlargement and a fourth heart sound or S4 gallop that increases with inspiration.
Testing for Tricuspid Regurgitation
Doppler echocardiography, a type of ultrasound procedure, is usually used to identify and monitor tricuspid regurgitation, a condition where the valve on the right side of your heart doesn’t close properly. This allows some blood to flow back into your heart’s upper right chamber. This ultrasound will help your doctor understand how your blood is flowing and how fast it’s moving, as well as measure the pressure in your right ventricle – the lower right chamber of your heart.
During this procedure, the doctor will look at several features of your heart. They might find that the tricuspid valve is moving normally or not. There might also be notable valve issues such as Ebstein anomaly (a rare heart defect that’s present at birth), leaflet prolapse (where the leaflets of the valve flop or bulge back into the upper heart chamber), flail leaflet, endocarditis (an infection of the heart’s inner lining), carcinoid heart disease (a heart condition due to a specific type of hormone-releasing tumor), and rheumatic valve disease.
Your doctor will also check whether your right atrium and right ventricle are dilated which means they are abnormally enlarged and if the annulus (the opening of the heart valve) of the tricuspid valve is dilated. They will also observe how the wall between your heart’s chambers is moving as this can show whether your right ventricle is overwhelmed with blood volume. Your right ventricle’s functionality, which can either be hyperdynamic (overactive), normal, or reduced, can be a sign of what’s causing the tricuspid regurgitation and how well your right ventricle is managing the condition.
The regurgitant flow velocity, which measures the speed of the blood flowing back through the tricuspid valve, can help your doctor calculate your right ventricular and pulmonary arterial systolic pressure, the pressure in your lung arteries. This is converted into a pressure gradient using a formula, giving your doctor a clearer picture of whether you’re experiencing pulmonary hypertension (high blood pressure in your lung arteries).
Specific levels and values are used to determine the severity of your tricuspid regurgitation, categorizing it as mild, moderate, or severe.
Other tests may be used to understand your heart’s condition better and to look for symptoms of tricuspid regurgitation. These tests may include a chest x-ray, blood tests to check for abnormal liver function, electrocardiography (a test that checks the electrical activity of your heart), and cardiac catheterization (a procedure to diagnose and treat cardiovascular conditions).
A type of imaging method, Cardiac magnetic resonance (CMR) imaging, might also be used to get a detailed view of the tricuspid valve and to calculate the right ventricle’s size and function. However, this method has its limitations as it can’t separate the flow of blood from the structure of the heart like color Doppler echocardiography can.
Treatment Options for Tricuspid Regurgitation
The treatment for tricuspid regurgitation, a condition where the heart’s tricuspid valve doesn’t close tightly causing blood to flow backward instead of forward, depends on how severe the condition is, its cause, and if there are other related heart conditions like pulmonary hypertension, heart failure, or other valve conditions.
If you have severe tricuspid regurgitation, the plan might include medications, lifestyle changes, tricuspid valve surgery (if needed), and treating the underlying cause of your condition.
With regards to medications, the aim is to manage fluid overload, which happens when your heart is unable to pump out the blood it receives from your veins. Loop diuretics may be used to help remove excess fluid from the body. You might also be advised to limit salt intake and to raise the head of your bed to help with shortness of breath. Other possible medications could include digitalis (improves your heart’s ability to pump blood), potassium-sparing diuretics (prevent your body from losing too much potassium), ACE inhibitors (relax blood vessels), and anticoagulants (prevent blood clots). If you have atrial fibrillation or an abnormal heart rhythm, antiarrhythmic medications can be used to control this.
As for surgery, the need for tricuspid valve surgery is often based upon whether surgery for other heart valve diseases is necessary. For instance, if you need surgery for another heart valve and have severe tricuspid regurgitation, tricuspid valve surgery is usually recommended. When there is a mild or moderate tricuspid regurgitation, tricuspid valve repair might be recommended if there is an enlargement of the tricuspid annulus (the ring of fibrous tissue that forms the base of the heart valve) or a history of right heart failure.
There are situations when tricuspid valve surgery might be needed without relation to any other heart valve disease. If your symptoms persist, despite medications, and you have severe tricuspid regurgitation, doctors might suggest tricuspid valve surgery. The preferred timing is before any significant right heart function loss. In severe cases, even without symptoms, surgery may still be a consideration, particularly if there is ongoing heart dysfunction. However, this is still a debated topic among physicians.
Lastly, the treatment can also depend on the cause of the tricuspid regurgitation. For example, if the condition is caused by endocarditis, a heart valve infection, the treatment usually involves removing the infected valve without immediate replacement. Once the infection is managed using antibiotics and if symptoms of heart failure persist, a surgeon may then insert an artificial valve. However, if your tricuspid regurgitation is due to Ebstein anomaly, a rare heart defect present at birth, and you do not have any symptoms, surgery might not be needed. But if symptoms do occur, surgery to repair or replace the tricuspid valve may be required.
What else can Tricuspid Regurgitation be?
When trying to diagnose tricuspid regurgitation, a doctor might consider whether the symptoms could be accounted for by any of the following conditions:
- Ascites (fluid buildup in the abdomen)
- Cirrhosis (advanced liver disease)
- Ebstein anomaly (a rare heart defect present at birth)
- Eisenmenger syndrome (a long-term complication of uncorrected heart defects)
- Heart failure
- Marfan syndrome (a genetic disorder that affects the body’s connective tissues)
- Cardiogenic shock (a severe reduction of blood pumped by the heart)
- Atrial fibrillation (irregular and often rapid heart rate)
- Dilated cardiomyopathy (a disease of the heart muscle)
- Biliary disease (disease affecting the bile ducts or gallbladder)
- Cor pulmonale (failure of the right side of the heart)
- Mitral regurgitation (a disorder in which the heart’s mitral valve doesn’t close properly)
- Carcinoid tumor (a type of slow-growing cancer)
What to expect with Tricuspid Regurgitation
The outlook for tricuspid regurgitation, a condition where the heart’s tricuspid valve doesn’t close tightly causing blood to flow backward into the heart, is generally positive. However, if you have increased pressure in your pulmonary artery and pulmonary hypertension (high blood pressure in the lungs), it indicates a higher chance of right ventricular dysfunction. This is a condition where the right side of your heart fails to pump blood effectively. As such, it may require more support after tricuspid valve surgery through the use of inotropic medications, which strengthen the heart’s contractions.
Possible Complications When Diagnosed with Tricuspid Regurgitation
Tricuspid Regurgitation, which refers to a condition where the heart’s tricuspid valve does not close properly, can lead to several complications. These include:
- Cardiac cirrhosis, a condition wherein the liver has scarring due to chronic heart problems.
- Ascites, which is the buildup of fluid in the space between the lining of the abdomen and the organs.
- Thrombus formation and embolization, a condition where blood clots form and can travel to different parts of the body.
Meanwhile, there can also be complications related to the medical procedures used to treat Tricuspid Regurgitation, which include:
- Heart block, a condition which disrupts the electrical signals in the heart’s upper and lower chambers.
- Thrombosis of the prosthetic valve, which means blood clots forming on the artificial heart valve.
- Infection, including the risk of infections around the artificial valve.
- Arrhythmias, or irregular heart rates.
Recovery from Tricuspid Regurgitation
The term ‘tricuspid regurgitation’ refers to a condition where the heart’s tricuspid valve doesn’t close tightly, causing blood to flow backward in your heart. When a patient is recovering from surgery for this condition, the following care is typically needed:
Firstly, medication to prevent blood clots (anticoagulation) might be necessary if the patient has a specific type of irregular heart rhythm called atrial fibrillation, or if they’ve had a valve replacement. Secondly, any heart rhythm problems (arrhythmias) that the patient has need to be managed. Thirdly, any infections the patient has should be treated. And fourthly, any signs of heart failure should be addressed.
Patients who have had their valve removed should have a check-up every six months using a test called an echocardiogram, which uses sound waves to produce images of your heart. For those who have had their valve replaced, the same test should be conducted once a year. This regular echocardiography helps healthcare professionals monitor their condition efficiently and decide the best way to manage their heart health.