What is Uremic Pericarditis?
The pericardium is the stretchy bag-like structure that wraps around our heart. It is made of two layers, named the visceral and parietal layers, which have a small gap in between them – often referred to as a “potential” space. Under normal conditions, this space contains anywhere from 15 to 50 mL of fluid that helps reduce friction. Acute pericarditis means that the pericardium becomes inflamed. Various factors can cause pericarditis, including infection, autoimmune reactions, cancer, and uremia.
Uremic pericarditis is a rare yet serious condition that occurs as a result of end-stage kidney disease (ESRD). This was first described by Richard Bright in 1836. It used to be more common in the early days of dialysis treatment. However, as dialysis methods have improved, it has become less common. It was once believed that viral illnesses could create uremic pericarditis. The disease is marked by a rough, fibrous surface on the heart. If there is fluid present, it usually contains a large number of proteins and mononuclear cells.
The people most likely to experience uremic pericarditis are those with end-stage kidney disease and those with severe azotemia, a condition where there’s a high level of urea nitrogen in the blood (BUN) typically above 60 mg/dL. Symptoms of uremic pericarditis include chest pain, especially when lying down, a distinct heart sound known as a pericardial rub that is often audible, and in severe cases, cardiac tamponade, a serious condition where fluid collects around the heart interfering with its normal function. To diagnose uremic pericarditis doctors usually perform an electrocardiogram, which normally shows unusual elevations in the patterns of ST and T-waves. The most common way to treat this condition is to lower the BUN levels through dialysis.
What Causes Uremic Pericarditis?
People with advanced kidney disease, or end-stage renal disease, often have trouble keeping fluids and electrolytes (minerals in your blood like sodium, potassium, and calcium) balanced. This can result in a build-up of harmful by-products like nitrogen waste.
Research has shown that the buildup of these harmful substances, along with an overload of fluids and an imbalance of electrolytes, contributes to a condition called uremic pericarditis. This is an inflammation of the pericardium, which is a thin, two-layered sac that covers the outside of the heart. Some research suggests nitrogen waste products can cause inflammation leading to pericarditis. Other researchers believe changes in the body’s acid balance, high calcium levels, and high uric acid levels can play a role in causing uremic pericarditis.
Uremic pericarditis can occur if a patient with stable advanced kidney disease doesn’t get enough dialysis, a treatment that cleans the blood when the kidneys can’t. This can also happen to patients with advanced kidney disease who need more dialysis due to other health issues. Some patients have reported increased pericarditis after missing dialysis treatments or not getting enough dialysis because of problems with their vascular access, the site on the body where the blood is removed and returned during dialysis.
Risk Factors and Frequency for Uremic Pericarditis
Uremic pericarditis is a condition that’s hard to track because its symptoms and diagnosis can vary a lot. It used to be found in between 3% and 41% of patients, but these numbers have gone down in recent years. Nowadays, due to advancements in a type of treatment called hemodialysis, and a better understanding of how metabolism changes with ESRD, the condition is found in about 5%-20% of patients, and even less than 5% in the last few decades.
Signs and Symptoms of Uremic Pericarditis
Uremic pericarditis is a medical condition often seen in patients with chronic kidney disease or those on dialysis. These patients typically experience chest pain, which is relieved when leaning forward. In contrast to non-uremic pericarditis, which is characterized by sudden onset of pain in the chest, the onset of uremic pericarditis is gradual. Other possible symptoms include fever and shortness of breath. These symptoms are similar to those experienced during a heart attack, so it’s important to rule out any heart-related problems.
In cases associated with dialysis, cardiac tamponade can occur in 20% of patients and hypotension in 60% of cases, especially in those on the verge of tamponade. This is quite high compared to those without cardiac tamponade, which is at about 6%.
A medical exam might detect a pericardial friction rub – a scratchy and squeaky sound best heard near the left edge of the sternum when the patient leans forward and holds their breath. This sound is almost always present in uremic pericarditis but can come and go. The rub consists of three different sounds related to:
- Atrial systole (heartbeat phase when the atria contracts to send blood to the ventricles)
- Ventricular systole (heartbeat phase when the ventricles contract to send blood out of the heart)
- Rapid ventricular filling during the diastole phase (heart relaxing and filling with blood)
Testing for Uremic Pericarditis
If your doctor suspects that you have uremic pericarditis, which is an inflammation of the pericardium (the sac-like membrane around your heart) due to kidney failure, they will likely use certain tests to make their diagnosis.
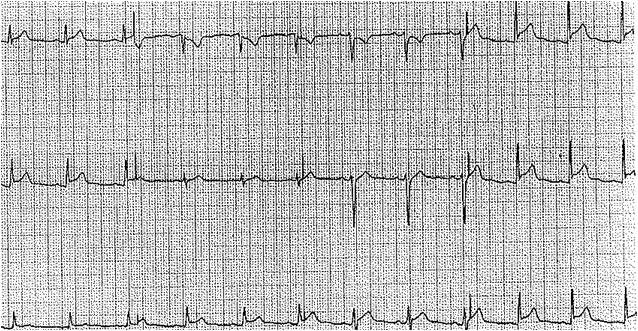
One of these tests is an electrocardiogram (ECG) which is a test that measures the electrical activity of your heart. In patients with pericarditis, the ECG often shows certain changes in the heart’s pattern, such as diffuse and widespread ST and T-wave elevations. This is different from an ST-segment elevation myocardial infarction, which is another way to say a heart attack, where these elevations are limited to certain areas. As the pericarditis progresses, these elevations may return to normal, and there may also be T-wave inversions seen.
Besides an ECG, other cardiac biomarkers might be elevated, like troponins which are a group of proteins that help regulate the heart’s contractions. But these are not necessary to confirm the diagnosis of pericarditis.
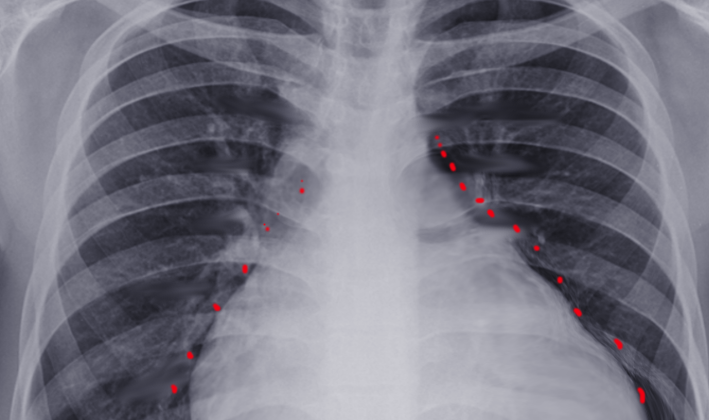
A chest X-ray may also be ordered. This can reveal an increased cardiac silhouette, indicating that there might be a buildup of fluid (effusion) around your heart. Other imaging options that can be used to diagnose pericarditis include cardiac magnetic resonance imaging (MRI) and computed tomography (CT scan). However, for patients with advanced kidney disease, gadolinium, a contrast agent used in MRI, should be avoided due to the risk of a condition called nephrogenic systemic fibrosis.
An echocardiogram, which uses sound waves to create images of the heart, is another important test. It could show a restrictive pattern due to the stiffness of the pericardium caused by adhesions, which are bands of scar-like tissue. Up to half of the patients with uremic pericarditis show a buildup of fluid around the heart on the echocardiogram.
It’s important to note that diagnosis of pericarditis is primarily based on clinical symptoms, and while all these tests can help, they are not always necessary to make the diagnosis.
Your doctor might also order routine blood tests like complete blood count (CBC), tests to check inflammation levels, kidney and liver function tests, and creatine kinase troponins. They might also look for an increased erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which are common in inflammation.
In some instances, a pericardial biopsy may be done. This involves taking a small sample from the pericardium for examination under a microscope. It might show non-necrotizing or necrotizing fibrinous pericarditis in constrictive pericarditis, or it might look normal.
Treatment Options for Uremic Pericarditis
The typical first-line treatment for uremic pericarditis, a heart condition caused by severe kidney disease, is to start or enhance dialysis, which is a treatment to filter waste and excess fluids from the blood. Dialysis often helps reduce chest pain and fluid buildup around the heart (pericardial effusion) in people with uremic pericarditis.
If dialysis doesn’t work sufficiently, anti-inflammatory medications and steroids are sometimes recommended. These help reduce inflammation and can offer some pain relief. However, they don’t always successfully treat uremic pericarditis. Besides, using steroids can be a bit controversial as they may relieve symptoms but could also increase the chance of the disease coming back. Plus, they may have side effects like higher blood sugar levels, the risk of osteoporosis (a condition that weakens bones), and potential effects on brain function in older people. People who cannot take non-steroidal anti-inflammatory drugs (NSAIDs) for various reasons may use low-dose steroids. Certain treatments, like injecting steroids directly into the pericardial space (the area around the heart), have been tested but are rarely used due to possible complications like bleeding into the chest, infections, collapsed lung, heart rhythm problems, and air in the pericardial space.
If the disease doesn’t improve with dialysis, the next step could be pericardiocentesis–a procedure where a needle is used to remove the excess fluid from around the heart. This could relieve symptoms and prevent complications. This procedure is typically done within 7 to 14 days, but if the condition is severe and causing a dangerous situation where fluid is putting pressure on the heart–called a cardiac tamponade–emergency pericardiocentesis is recommended.
Last up is pericardiectomy, which is a surgery to remove part or all of the pericardium (the outer layer of the heart). This is typically reserved for cases where the pericarditis keeps coming back and causing fluid buildup. It’s recommended to get an echocardiogram, a type of ultrasound of the heart, every 3 to 5 days during key stages of the disease to keep track of the pericarditis and the fluid accumulation.
What else can Uremic Pericarditis be?
In diagnosing uremic pericarditis, which mostly affects patients with advanced kidney disease or on dialysis, it’s important to rule out other potential causes of pericarditis. This is because numerous factors can lead to this condition such as:
- Infections, which can be viral, bacterial, or fungal in nature
- Inflammatory conditions like systemic lupus erythematosus, scleroderma, or vasculitis
- Metabolic issues, such as hypothyroidism
- Cancer, whether it originates in the heart (primary) or spreads from other body parts (metastatic)
- Heart injuries, resulting from blunt or penetrating trauma
- Heart diseases, including postpericardiotomy syndrome, heart attack, or aortic dissection
- Certain medications, such as hydralazine, methyldopa, procainamide, and minoxidil, which can induce pericarditis
Therefore, an exhaustive medical evaluation is crucial for the correct diagnosis.
What to expect with Uremic Pericarditis
In general, most people, around 85% to 90%, recover completely from uremic pericarditis, a condition associated with kidney disease that causes inflammation of the pericardium – the sac-like membrane that surrounds the heart. However, with each episode of this condition, the chances of it happening again increase.
Uremic pericarditis can lead to serious health complications and occasionally it can result in death. It’s also important to note that between 3% to 5% of patients with uremic pericarditis might develop hemorrhagic pericarditis – a severe form of pericarditis where the pericardium fills with blood, which can be potentially life-threatening.
Possible Complications When Diagnosed with Uremic Pericarditis
The most dangerous complication of uremic pericarditis is the onset of cardiac tamponade. This happens when there is an increase in fluid around the heart because of uremic pericarditis, which can stop the heart from pumping blood to the other parts of the body. When the pressure around the heart increases, it prevents the heart from contracting and pumping blood effectively. Symptoms typically associated with cardiac tamponade include low blood pressure, swelling in the neck veins, a specific type of irregular pulse called pulsus paradoxus, and muted heart sounds.
Another tell-tale sign of cardiac tamponade can be seen in an electrocardiogram, a test of the heart’s electrical activity. It might demonstrate ‘electrical alternans’ – a variation in the electrical signals from the heart because the heart is floating within the excess fluid around it. The immediate treatment for this condition is pericardiocentesis, a procedure to remove the excess fluid from around the heart.
Common Symptoms:
- Low blood pressure
- Swelling in the neck veins
- Irregular pulse (pulsus paradoxus)
- Muted heart sounds
- Variation in the heart’s electrical activity
Preventing Uremic Pericarditis
Uremic pericarditis is a heart condition that can occur because of harmful toxins building up in your body. This often happens if you have kidney problems and your body isn’t able to effectively remove these toxins. The primary treatment for this condition is dialysis, which is a procedure that replicates some of the functions of the kidneys, and taking your medication as directed by your healthcare provider.
It’s important for people with chronic kidney disease to be aware that they might be at risk of uremic pericarditis. If you experience chest pain, it’s crucial to seek medical attention immediately as it could be a sign of this condition. If you’re already receiving dialysis, it’s vital to follow your treatment plan because not doing so can lead to multiple complications, including uremic pericarditis.